Print Entire Issue
Columns
Directly Speaking
President's Message
Crank's Corner
ICHPeople
Board of Pharmacy Update
Government Affairs Report
ICHP Leadership Spotlight
ICHP Leadership Spotlight
New Practitioners Network
Hi-Tech
Public Education & Awareness Outreach Publication Subcommittee
Attention ASHP Pharmacist Members
Educational Affairs
Educational Affairs
Educational Affairs
Educational Affairs
Professional Affairs - CPE Opportunity!
Organizational Affairs
Features
Staff Changes
Passing The Baton To Our Team
ICHP's Newest Affiliate Leaders
Opioid Task Force - CPE Opportunity
Annual Meeting Recap
College Connection
Midwestern University Chicago College of Pharmacy
Rosalind Franklin University College of Pharmacy
Southern Illinois University Edwardsville School of Pharmacy
University of Illinois Chicago College of Pharmacy
More
Upcoming Events
Welcome New Members!
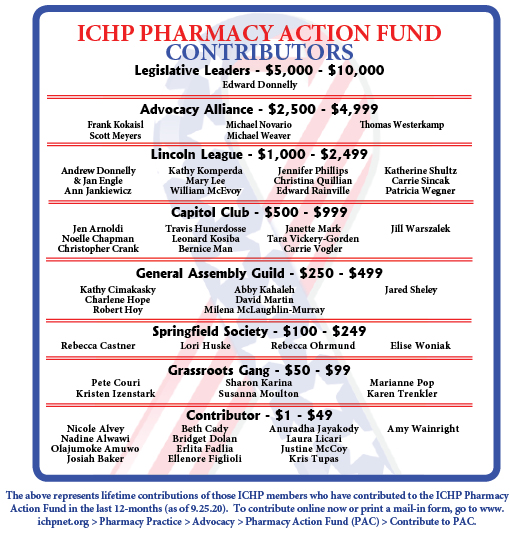
Pharmacy Action Fund Contributors
Board of Directors

Illinois Council of Health-System Pharmacists
4055 North Perryville Road
Loves Park, IL 61111-8653
Phone: (815) 227-9292
Fax: (815) 227-9294
ichpnet.org
KeePosted
Official News journal of the Illinois Council of Health-System Pharmacists
EDITOR
Jennifer Phillips
ASSISTANT EDITOR
Milena Murray
MANAGING EDITOR
Scott Meyers
ASSISTANT MANAGING EDITOR
Trish Wegner
DESIGN EDITOR
Melissa Dyrdahl
ICHP Staff
EXECUTIVE VICE PRESIDENT
Scott Meyers
VICE PRESIDENT - PROFESSIONAL SERVICES
Trish Wegner
DIRECTOR OF OPERATIONS
Maggie Allen
INFORMATION SPECIALIST
Heidi Sunday
CUSTOMER SERVICE AND
PHARMACY TECH TOPICS™ SPECIALIST
Jo Ann Haley
BOOKKEEPER/VENDOR LIASON
Kim Anderson
COMMUNICATIONS MANAGER
Melissa Dyrdahl
LEGISLATIVE CONSULTANTS
Liz Brown Reeves
Mitch Schaben
ICHP's Mission Statement
Advancing Excellence in
Pharmacy
ICHP's Vision Statement
ICHP dedicates itself to
achieving a vision of pharmacy practice where:
·
Pharmacists are
universally recognized as health care professionals and essential providers of
health care services.
·
Pharmacists use their
medication expertise and leadership skills to optimize the medication use
process and patient outcomes.
·
Pharmacy technicians are
trained and PTCB certified to manage the medication distribution process.
ICHP's Goal Statements
·
Raising awareness of the
critical role pharmacists fulfill in optimizing medication therapy and ensuring
medication safety in team-based, patient-centered care.
·
Providing high quality
educational services through innovative continuing pharmacy education and
training programs, and sharing evidence-based best practices.
·
Developing and nurturing
leaders through mentorship, skill development programs, and leadership
opportunities.
·
Working with national
and state legislators and policymakers to create or revise legislation and
regulation critical to pharmacy practice and quality patient care.
·
Urging pharmacy
technician employers to require successful completion of an accredited pharmacy
technician training program and PTCB certification of all pharmacy technicians.
Approved by the ICHP
Board of Directors May 30, 2018.
KeePosted Vision
As an integral publication of the Illinois Council of Health-System
Pharmacists, the KeePosted newsjournal will reflect its
mission and goals. In conjunction with those goals, KeePosted will
provide timely information that meets the changing professional and personal
needs of Illinois pharmacists and technicians, and maintain high publication
standards.
KeePosted is an official publication of, and is copyrighted by, the
Illinois Council of Health-System Pharmacists (ICHP). KeePosted is
published 4 times a year. ICHP members received KeePosted as
a member benefit. All articles published herein represent the opinions of the
authors and do not reflect the policy of the ICHP or the authors’ institutions
unless specified. Advertising inquiries can be directed to ICHP office at the
address listed above. Image disclaimer: The image used in the Pharmacy Tech
Topics™ advertisement is the property of © 2017 Thinkstock, a division of Getty
Images. Some images are property of © 2020 Adobe Stock.
Copyright © 2020, Illinois Council of Health-System Pharmacists. All rights
reserved.
Columns
 Directly Speaking
Directly Speaking
So Long, Farewell, Auf Wiedersehen, Goodbye!
by Scott A. Meyers, Executive Vice President
I leave and heave a sigh and say goodbye. For some reason, that song has found its way into my head this fall. At the start of 2020, the Swedish rock band Europe’s 1986 release The Final Countdown was rocking through my head. It didn’t take long though - mid-March I believe - and the 1987 R.E.M. piece It’s the End of the World as We Know It resounded daily, if not hourly! If you haven’t figured out from my many columns, I love song titles, their lyrics, and movie quotes and I use them whenever I can.
And in case you missed the news, this is my last Directly Speaking, as my retirement fast approaches at year’s end. Probably, the most appropriate song title for my last column should be one made famous by Bob Hope (a comedian, TV, and movie star form the 1930’s through the 1970’s for our millennial and Gen X members) in 1938, "Thanks For The Memories". By the way, no, I wasn’t alive back then! But it became Hope’s signature song and he sang it regularly on his TV show, countless concerts, and most importantly, USO trips visiting US armed forces, all over the world. Like that song, I would like to thank ICHP, its members and its staff for more memories than I can count!
Because of my tenure as the first Executive Director and eventually, Executive Vice President, I’ve done some things and met many people I would probably have missed without this job! Actually, without my tenure first as a member of ICHP, I would have missed even more!
My first ASHP Midyear Clinical Meeting was a result of the 1986 version of FOMO (Fear of Missing Out. Yes, we had it back then, we just didn’t call it that!). And that FOMO was fueled even early with my attendance at my first ICHP Annual Meeting, where I sat at a back table in the Awards Luncheon, thinking to myself, “Someday, I want to say I know the people at the head table!” Now, I have a role in deciding who sits there!
I have vivid memories of the multiple trips to Washington, DC in 1992 through 1995 when ICHP, the Michigan Pharmacists Association, ASHP, and APhA hammered out the details of a project we now know as PTCB! Twenty-five years later and more than 700,000 technicians are certified. PTCB is a shining example of what pharmacy can accomplish when it comes together to work on a common goal!
Through PTCB, I’ve met, gotten to know, and become friends with Joseph A. Oddis (ASHP), John Gans (APhA), Lucinda Maine (APhA, now AACP), Larry Wagenknecht (MPA), Carmen Catizone (NABP), Tom Menighan (APhA), and more. I left off Henri Manasse (ASHP and before that UIC) because while we worked together with PTCB, we were already friends from a long time ago in pharmacy school. And I can’t forget William “Bill” Zellmer, who spent dozens if not hundreds of hours helping us hammer out the details of PTCB on behalf of Dr. Oddis and ASHP, but we too, were already acquaintances by then! But those PTCB hours galvanized our friendship.
I know almost as many ASHP Past Presidents as I do ICHP Presidents and I dine with several of the former ASHP royalty each year at the Midyear and Summer Meetings as part of a very informal social group of the pharmacy family from around the entire country. I know the Executive Director of the Louisiana Board of Pharmacy personally and have never held a pharmacist license in that State!
I’ve traveled to Midyears in the current big four (Las Vegas, Orlando, Anaheim, and New Orleans) multiple times and add visits to Atlanta, Dallas and Miami too! Not to mention the ASHP Summer Meetings in Washington DC, San Diego, Minneapolis, Reno, Seattle, Chicago (Rosemont, actually), Denver, Las Vegas, Philadelphia, Baltimore, San Francisco, Nashville, Boston, Orlando, Tampa, and Los Angeles. Thank you ICHP and ASHP for adding States to my list of “Been there!”.
More importantly, I’ve met so many Illinois pharmacists, pharmacy technicians, pharmacy students, and pharmacy educators over the past 28-plus years, many of whom are now friends or very close friends! You have to be a close friend to put up with the way I play golf! For those of you who attend ICHP Annual and Spring Meetings, you know I spend most of the meeting talking with old friends and making more new ones. It’s often hard to force myself into the educational sessions, not because they aren’t good, they’re great (as Tony the Tiger would say) but because the education isn’t as important as the networking for me.
Most importantly, this job that I am handing over to our new EVP, Chris Crank, gave me the opportunity to go to Springfield and to Washington, to carry our messages over and over again to the General Assembly and the Congress. I can even say that I’ve met a President because of ICHP, but there is an asterisk, Illinois and U.S. Senator Barack Obama hadn’t gotten that far yet when I met him in Springfield and in Washington! And, I can even smile when remembering Senator Durbin saying, “Oh yes, you’re Mary Moody’s friend!” But I’ve had all these experiences on behalf of you!
I would be remiss if I didn’t mention the all-knowing (sometimes too much) and dedicated ICHP staff! I’ve worked with a cadre of outstandingly dedicated and faithful individuals. From Connie Miller, ICHP’s first full-time employee, followed by Heidi Sunday, who Connie hired while I was at a Midyear Meeting in Miami, and who is still with us today, over 26 years later, to a couple dozen in between then and the crackerjack team we’ve assembled today! ICHP members should be thankful for their current staff of Trish Wegner, Maggie Allen, Heidi Sunday, JoAnn Haley, Melissa Dyrdahl, and recent additions Kim Anderson and Chris Crank. I know I am very thankful for all of them! I should mention a special thank you too, to Jan Mark, our very recently retired bookkeeper and meeting greeter and to Barb Yahn, former Communications Director and current office cleaning lady! I know I will be back to see them from time to time but not as early in the morning or as often as now!
I have written this column a couple of weeks ahead of this year’s Annual Meeting, this year’s VIRTUAL Annual Meeting, and a movie that keeps coming to mind is the 1980 classic Airplane!. It was intended as a spoof of a series of movie dramas, Airport, Airport 1975, Airport ’77, and The Concorde…Airport 1979, but it became a cult classic spoof of its own following similar to Dumb and Dumber. In Airplane!, one of the supporting characters, an air traffic controller, Steve McCrosky, is played by Lloyd Bridges (father of Jeff and Beau Bridges, hopefully the younger crowds have heard of the sons, if not dad) and as the drama and tension mount throughout the movie, McCrosky confides in his co-workers that he picked a bad week to first “quit smoking”, later to “quit drinking”, next to “quit taking amphetamines” and finally to “quit sniffing glue”. In 2020, I feel like I picked a bad year to retire! With this year’s virtual Annual Meeting and no Spring Meeting, there’s no chance to say goodbye in person. So I guess that’s why the song with the same name as the title of this column keeps echoing in my head.
It’s been a pleasure serving as the ICHP and “Your” Executive Director and Executive Vice President. I can only say what so many others before have said, “You truly receive more than you give!” Thank you all and I look forward to seeing many of you when I come to an ICHP meeting as an attendee! And I might see if the staff will get me a “Retired Staff” ribbon for my name tag. I know they’ll be happy to give me the one that says, “Has Been”! ☺■
Pictured Top Row (left to right):
- Harland Lee installing Scott Meyers as President (1988)
- Scott's 10-year Anniversary as Executive Director - Scott Meyers
- Breaking Ground on the ICHP Building (2005) -
Nancy Shapiro, Chris Quillian, Trish Wegner, Ed Donnelly, Diana Johnson (Parks Chamber of Commerce), Loves Park City Treasurer, Mike Rajski, Mike McEvoy, Michael Kalodemis (Chase), Scott Meyers
- PTCB Board of Governors (2009)
Scott Meyers, Larry Wagenknecht, Melissa Murer Corrigan, John Gans, Henri Manasse, Carmen Catizone
- ICHP Fall Gathering (1992)
Scott Meyers and his father, Stanley Meyers
- Leg Day (2015)
Governor Bruce Rauner, Chris Quillian, Trish Wegner, Kathryn Schultz, Scott Meyers
- Leg Day (2007)
Senator Dick Durbin, Scott Meyers, Cheri Gallagher, Miriam Mobley Smith, Trish Wegner, Senator Barack Obama
 President's Message
President's Message
Incoming Address
by Jennifer Arnoldi, PharmD, BCPS Clinical Associate Professor, SIUE School of Pharmacy President of ICHP
Thank you for taking a moment out of your busy day to enjoy this edition of KeePosted™. I wish I was addressing you live at our Annual Meeting, but I appreciate the opportunity to connect with you here. Each year, the incoming President of ICHP identifies a theme to signify their presidential year; I have struggled in making my decision. What words of inspiration or optimistic slogan should I choose to encompass what I hope we accomplish this year as an organization, during one of the most challenging years in recent memory?
The COVID-19 pandemic has racked our world in unimaginable ways. There is no moving forward without acknowledging that, in many ways, we are forever changed. When I first saw news of the virus in Wuhan, never did I imagine that we would all spend the next days, weeks, and months worrying about access to masks, hand sanitizer, and bleach wipes. I didn’t suspect that we would shelter in place, work from home when possible, and limit our contact with the outside world. I couldn’t fathom a world in which I wouldn’t see my parents, my niece and nephew, or many of my friends for months on end except for on a screen.
I could in no way imagine the way this pandemic would rock the world of health system pharmacy. In some areas of the state, it seemed that combating the virus was all-consuming, taking with it hard-to-find PPE, staff morale, and ultimately, some of our patients’ lives. In other parts of the state that were less affected by the virus, voluntary suspension of non-emergent procedures and admissions brought pharmacy departments to their knees, requiring voluntary or involuntary furloughs and in some cases, layoffs. Our students’ educational experiences were disrupted, abruptly transitioned to virtual learning for both classroom and on-the-ground training. Our graduates faced one of the most exciting days of their lives in a way that they had never imagined: virtually and socially distanced. Would they be able to take their board exams? When would student loans started coming up for repayment?
As a dedicated book worm, I felt the struggles we have been facing seem like they are something conjured up in science fiction or a dystopian tale. I come by my love of books honestly. Growing up, my very patient father read The Lord of the Rings series by J.R.R. Tolkien to my brother and I, a little bit each night. I only found out as an adult that those books contained many songs, as my dad was sure to skip over those while he read. Even for his children, the man could only go so far. Why do I bring this up? During the past few months, I kept coming back to a quote from The Two Towers. In it, Sam is offering words of encouragement to his best friend during a mission that challenges them in every sense of the word. Despite their difficulties, Sam says, “Because how could the end be happy? How could the world go back to the way it was when so much bad had happened? But in the end, it’s only a passing thing, this shadow. Even darkness must pass. A new day will come. And when the sun shines it will shine out the clearer.”1
Just like Sam, I can see the glimmers of light amidst the shadows. At every stage of these challenges, despite the sometimes-overwhelming feelings of fear, anxiety, and exhaustion, I have seen hope and humanity at every opportunity. We have banded together in ways that we didn’t think possible until we were forced into it. We have leveraged the use of technology to connect, communicate, and create. When the world ran out of hand sanitizer, we compounded it. When we didn’t have masks, we made them. We pulled together and found out what it really meant to be a pharmacy family.
As an organization, ICHP was there for us as a bridge to connect us to one another. We continued the important work of meeting in our regular Divisions and Networks. While we were not able to meet for the Spring Meeting, the Division of Educational Affairs and ICHP staff worked diligently to bring us a virtual Annual Meeting. The Diversity in Pharmacy series has offered us the opportunity to amplify the voices of our BIPOC members and colleagues, connecting us with their stories and experiences. The sense of connectedness and community that we have been able to maintain is something that I hope we don’t lose sight of as the darkness passes and the sun shines out the clearer. With that in mind, I selected the theme of “Building Bridges” and hope that we can highlight all the ways we can connect, unite, and extend the impact of our profession into the world. I hope that we can all build bridges together.
And if you decide to read The Lord of the Rings, don’t skip the songs. It’ll help you live in that world just a little while longer. ■
Reference
Tolkien, J.R.R. The Two Towers. New York: Houghton Mifflin Company, 1994. Print.
Crank's Corner
Positive Thinking: An Important Skill for Stressful Times
by Christopher W. Crank, Executive Vice President Designee
If you are like me, the COVID-19 pandemic and social injustices happening in the United States have caused you to feel a flurry of emotions. At times, I have felt angry, sad, isolated, frustrated, helpless, and hopeless. On the other hand, I have felt joyful, grateful, thankful, hopeful, and proud. It appears as though we have witnessed some of the best and the worst of humanity. Through all of the stresses and troubles, I have tried to keep an overall positive attitude. This is because having a positive attitude and mindset are key to being able to developing resilience and being able to successfully cope with challenges. Positive thinking does not mean pretending that everything is “sunshine and rainbows”. It is also not ignoring problems and stressful situations, hoping that they will go away. Positive thinking means approaching problems in a more positive and productive way.
To understand what positive thinking looks like, it helps to know what negative thinking looks like. Characteristics of negative thinking include:
- Focusing only on the negative aspects of a situation. For instance, a person thinks their presentation was terrible because there was a technical difficulty. Positive thinking would acknowledge the technical issue but also include other aspects in the assessment of the presentation, such as audience engagement, the quality of the material, and how the presentation was received.
- Blaming only oneself when bad things happen. An example would be blaming oneself for the failure of a group project. The person believes that they are the only reason the project was unsuccessful. Positive thinking acknowledges the failure, but involves a more objective assessment of the causes, which would then be used to form a plan to avoid making the same mistake again.
- Using a catastrophizing approach. Catastrophizing is when someone exaggerates the negative impact of an event. For instance, when one thing goes wrong in the day, they may think that the whole day was terrible. Positive thinking, in this instance, would not mean ignoring the negative event. Rather, it would mean keeping the single negative event in the perspective or framework of the entire day. Positive thinkers acknowledge the positives and the negatives from the day.
- Believing things can only be good or bad. There is no middle ground. Perfectionism is a great example of this behavior. If it isn’t perfect, it’s terrible. In this example, positive thinking would involve performing a critical assessment of what worked well and what did not.
Positive thinking requires framing and perspective. Like many things, a person is not always a positive or a negative thinker. Attitudes and mindsets change according to the topic, day, and/or situation. If you find yourself in a negative mindset, there are several ways you can try to adjust your thinking:
- Think about the areas where you have the negative mindset. Try to think of ways that you can find positive aspects about the situation. Adjust your thinking to include an assessment of the positives and the negatives.
- Check yourself throughout the day with periodic assessments. If you find yourself stuck in a negative mindset, look for ways to put a positive spin on the situation. Keep things in perspective.
- Find humor around you. Look for funny situations in your everyday life. Watch a funny video, or have a humorous conversation with someone.
- Avoid negative people when possible. Associating with a negative person can bring down even the most positive people. We have all had experiences with a negative coworker or acquaintance. It is important to support a person who is being negative, but not at the expense of your well-being. If the person’s negativity goes beyond a reasonable venting session, try changing the subject. If the negativity persists, remove yourself from the person’s vicinity if possible. Use the negativity as a reason to take a quick break or get away. If the problem persists, you may need to kindly explain to them that their negativity is impacting you.
- Connect with those that support you. It’s easy to feel negative and isolated right now. It is harder to be social with each other. Make a concerted effort to connect with those who support you. When is the last time you talked to your best friend from high school? Give them a call. Participate in virtual events that are not related to work. Trivia nights or having a drink with friends, even if it’s on an online platform, can help you feel more connected.
- Take care of yourself. Your ability to take a positive approach and manage stress is diminished when you are not taking care of your body. Getting enough exercise and sleep are essential for maintaining the coping skills and resiliency needed to routinely approach stressful situations with positive thinking. Plan for your exercise like you plan for your professional activities. If you find yourself ruminating on something negative, use meditation, mindfulness, exercise, or a hobby to shift your thinking. Excessive nicotine, caffeine, or alcohol may exacerbate stress, so avoiding or minimizing use is also key to effectively managing stressful situations
- Avoid too much social media or news. It is hard to go through a day anymore without reading or seeing something upsetting in the news or on social media. As a society we have unprecedented access to information, which can be overwhelming. We can find ourselves getting more and more upset as we listen to the news or read more comments on a social media post. If you find yourself getting too upset, angry, or negative while consuming media, the best approach is to step away. In addition, think about how much time you want to spend on social media and the news. Set limits based on your assessment and stick to them.
Positive thinking requires you to assess your current mindset. Once the assessment is completed, you can begin to take steps to adjust the mindset. Know that it is OK to feel overwhelmed or negative about what is going on. The negative feelings are a normal and appropriate response to the situation. However, it is important to not let negative situations and thoughts drive your whole perspective and the framework of your day-to-day life. If you feel that you cannot get out of your negative mindset or if you are experiencing depression, know that it is OK to seek help. Reach out to a professional for assistance. Taking the first steps towards getting help is not a sign of weakness; it is a sign of strength. A list of resources from the CDC is provided below.
CDC: Get immediate help in a crisis
- Call 911
- Disaster Distress Helpline: 1-800-985-5990 (press 2 for Spanish), or text TalkWithUs for English or Hablanos for Spanish to 66746. Spanish speakers from Puerto Rico can text Hablanos to 1-787-339-2663.
- National Suicide Prevention Lifeline: 1-800-273-TALK (8255) for English, 1-888-628-9454 for Spanish, or Lifeline Crisis Chat.
- National Domestic Violence Hotline: 1-800-799-7233 or text LOVEIS to 22522
- National Child Abuse Hotline: 1-800-4AChild (1-800-422-4453) or text 1-800-422-4453
- National Sexual Assault Hotline: 1-800-656-HOPE (4673) or Online Chat
- The Eldercare Locator: 1-800-677-1116 TTY Instructions
- Veteran’s Crisis Line: 1-800-273-TALK (8255) or Crisis Chat or text: 8388255
Find a health care provider or treatment for substance use disorder and mental health
- SAMHSA’s National Helpline: 1-800-662-HELP (4357) and TTY 1-800-487-4889
- Treatment Services Locator Website
- Interactive Map of Selected Federally Qualified Health Centers
References
- Mayo Clinic Staff. (2020, March 21). Stress management Stress basics. Retrieved September 28, 2020, from https://www.mayoclinic.org/healthy-lifestyle/stress-management/basics/stress-basics/hlv-20049495
- Mental Health and Coping During COVID-19. (n.d.). Retrieved September 28, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
ICHPeople
 Congratulations to Rebecca Ohrmund, CPhT.
Congratulations to Rebecca Ohrmund, CPhT. Becky was nominated as the chair of the ASHP Pharmacy Technician Forum Practice Advancement and Advocacy group for the 2020-2021 term. Thank you Becky for sharing your voice!
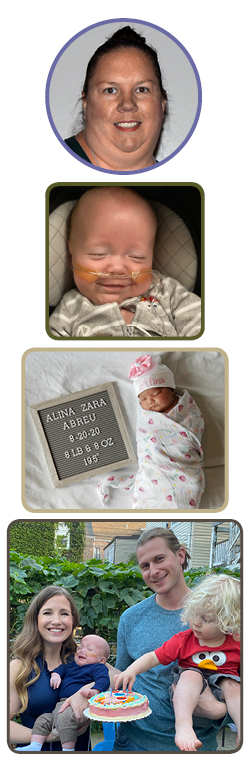
Welcome Baby Campbell!
Congratulations to ICHP Members Bryan McCarthy and his wife Sarah Sokol on the birth of their second baby boy, Campbell Bryan McCarthy. Campbell was born April 9th, 2020 weighing 3lbs 2oz and measuring in at 15.5" long. Campbell (also known as “Champ”) loves snuggling, playing with his big brother Hudson, and Motown music. Congrats, Bryan & Sarah!
Welcome Baby Alina!
On August 20, 2020, ICHP members Tamkeen & Pedro Aramis Abreu and brother Mikail (age 2) added Alina Zara Abreu (8 lbs 8 oz; 19.5") to their family. Welcome to the world little Alina!
Farewell McCarthy Family!
We bid a bittersweet farewell to ICHP Secretary and University of Chicago Medicine Director of Inpatient Pharmacy Services, Bryan McCarthy, as he and his family - including ICHP member and Bryan’s wife, Sarah Sokol, and their two boys Hudson and Campbell - are headed to Rhode Island. There, Bryan will assume the Director of Inpatient Pharmacy Services role for the 5-hospital system Lifespan, primarily based in Providence. Originally from upstate New York, this will make family visits much quicker and easier and provide Bryan with another excellent career opportunity. We wish them well and will miss them a lot.
Are you celebrating?
Let ICHP know so we can feature you in our upcoming issue of
KeePosted!
Email us at
MelissaD@ichpnet.org
Board of Pharmacy Update
Highlights of the September Meeting
by Scott A. Meyers, Executive Vice President
The September 8th Board of Pharmacy Meeting was held via conference call due to COVID-19 pandemic. These are the highlights of that meeting.
NABP District IV Meeting – The Annual NABP/AACP District IV Meeting is being held virtually on Thursday, October 8th from 1-5 pm. It is co-hosted by Ohio State University College of Pharmacy and the Ohio Board of Pharmacy. It will be a shortened event that will include a discussion on pharmacy responses to the COVID-19 pandemic. Several Board members indicated that they will participate.
Department Update - Staff member and Board General Counsel, Munaza Aman was asked questions related to the HHS Executive Order regarding pharmacist-provided immunizations. The Executive Order allows pharmacists to provide COVID-19 immunizations to patient 3 years of age and older. This conflicts with the Illinois Pharmacy Practice Act, which only allows pharmacist-provided immunizations for patients 14-years and older. The Department staff is aware of the Order but has not yet developed any guidance to Illinois pharmacists.
The rules allowing pharmacy technicians to administer immunizations are being developed, but will not be completed in a timely manner unless they are implemented as emergency rules. It is unlikely that an emergency rule will be drafted. The Department does not feel any urgency with these rules.
Legislative Update – IPhA Executive Director, Garth Reynolds presented the Legislative Update to the Board and reported that there was no new activity by the General Assembly. There is a working group drafting language for the Veto Session to make the HHS Executive Order on immunizations permanent in Illinois.
Public Comments – A brief report was provided on an IDPH Mass Vaccination Planning Group. The group has just begun to meet to create plans for the anticipated COVID-19 vaccine.
Next Meeting – The next meeting of the Board of Pharmacy is scheduled for November 10th, tentatively - potentially in Chicago but most likely via virtual call. Interested individuals should monitor the Department’s pharmacy webpage www.idfpr.com for more information. These meetings are open to the public and pharmacists, pharmacy technicians, and pharmacy students are encouraged to attend or listen in.
Government Affairs Report
A Report on the Final Meeting of the Collaborative Pharmaceutical Task Force
by Scott A. Meyers, Executive Vice President
The Task Force met via conference call on Tuesday, September 8th for its final meeting. In October, the Illinois Department of Financial and Professional Regulation will provide a report of this year’s Task Force recommendations to the Illinois General Assembly for possible implementation during the November and December Veto Session. While the final report has not been completed at the time of this writing. The following is a summary of the recommendations that will be contained in the Task Force Report.
The 2020 Task Force Report will contain the following recommendations:
- Establishment of a process to create standing orders through the Illinois Department of Public Health.
- Creation of an exemption to the 12-hour shift length limit for residents participating in nationally accredited residency programs.
- Revision of the Pharmacy Practice Act to clarify when mandatory meal breaks must be taken, and exempting non-dispensing pharmacists from meal and rest break recordkeeping.
- Revision of the Pharmacy Practice Act to require all pharmacies to establish and maintain a continuous quality improvement program with protections for those programs from subpoena of work documents for state or federal civil or criminal litigation.
- Appointment by the General Assembly of a new Task Force, charged with identifying a new reimbursement and remuneration model for pharmacist-provided patient care services.
When the Task Force’s final official report becomes available, ICHP will post it (or a link to it) on the ICHP website and announce its availability to the membership.
(Author’s Note: During last year’s Veto Session, the General Assembly expanded the original Task Force by 6 members, including 4 legislators. During this year’s deliberations, only three of the four legislators were actually appointed to the Task Force and no legislator participated in any meeting of the group.)
ICHP Leadership Spotlight
Meet Marianne Pop, PharmD, BCPS
What is your leadership position within ICHP?
I am the Chair-Elect of the New Practitioner Network.
Where is your practice site?
I am at the University of Illinois College of Pharmacy and OSF Saint Anthony Medical Center
How do you know that choosing pharmacy as a career was the right choice for you?
Pharmacy is for me because it allows me to pursue my interests in patient care, education, and public health. Also, as a pharmacist, your role is always expanding. My PharmD degree and post-graduate training in emergency medicine allowed me to combine my passions for solving acute patient care issues and ambulatory care. As clinical faculty for the University of Illinois College of Pharmacy, I have been given opportunities to educate future pharmacists. I have also been able to go beyond individual care by improving community health through vaccination programs. Although health careers offer opportunities for diverse roles, pharmacy is one field where the sky is the limit.
What is a challenge that you face in your practice?
A challenge that I face at my practice is having the ability to optimize medication regimens, but then identifying issues with affordability. As a pharmacist, we are able to learn the tricks of the trade such as drug savings cards, prior authorizations, medication coupon websites, and copay cards, among others. As a health-system pharmacist, I rely on my community pharmacy colleagues to stretch my patients' dollars. Community pharmacy staff are helpful every time, but it is challenging when you exhaust all modes of reducing a patient’s medication costs and the patient does not have the means to pay for necessary medications.
What makes ICHP great?
ICHP is a great organization because it is one of the most involved pharmacy organizations. This is evident in the student, technician, and pharmacist membership. Each meeting (live or virtual) is filled with innovative ideas from members who are vying to improve the profession. The organization also offers many opportunities from policy, education, and networking. As a Chair-Elect of the New Practitioner Network, I was able to learn how ICHP works closely with state officials to promote the profession. ICHP provides many modes of continuing education for pharmacists and technicians, making it easy to maintain your license. Lastly, ICHP holds multiple networking opportunities for all members at the local, regional, and state level.
What initially motivated you to get involved in ICHP?
I was motivated to join ICHP because I wanted to get involved in pharmacy advocacy at a local level. I was involved with the ASHP Section Advisory Group in Emergency Medicine for multiple years, but wanted to know more about what Illinois was doing to support the profession and my ideals. I found that ICHP matches my vision for pharmacy practice.
Is there an individual you admire or look up to, or a mentor that has influenced your career?
Special thanks to my dad, Thomas Platt, for making me who I am today in my career. He not only introduced me to pharmacy, but also instilled the work ethic that has made me successful.
What advice would you give to student pharmacists?
My advice for student pharmacists is to take every opportunity to learn what pharmacy has to offer by shadowing, networking, and challenging yourself.
Do you have any special interests or hobbies outside of work?
My special interests or hobbies outside of work include reading, traveling, and trying new foods. I am part of a monthly book club that meets to discuss books and try new restaurants. I am currently reading Just Mercy by Bryan Stevenson.
My favorite restaurants are fusion restaurants.
What is your favorite place to vacation?
My favorite place to vacation is Oregon. My family travels every summer to Oregon, where we hike and get to enjoy the beautiful beaches.
ICHP Leadership Spotlight
Meet Erin Shaughnessy, PharmD, MBA, BCPS
What is your leadership position within ICHP?
I am the Treasurer of NISHP.
Where is your practice site?
I am the Director of Pharmacy at Rush University Medical Center.
What is a pharmacy issue that keeps you from sleeping at night?
As we all know, COVID-19 and other societal challenges have put immense pressure on our healthcare system and our teams this year. Sustaining a parallel between providing high quality patient care, balancing pharmacy practice models, and having a culture that encourages team members’ wellness is at the forefront of my mind. Finding that consistent stability is a challenging opportunity, but it is important for all of us.
How do you apply ICHP learning and resources into your work?
I find the NISHP educational dinners and the ICHP Reverse Expos to be especially useful in my practice. The NISHP educational dinners are a great way to refresh clinical knowledge and compare processes with colleagues. The ICHP Reverse Expo “speed dating” format allows me to explore a multitude of vendors and products in an expedited time frame. Each time I attend an educational dinner or a Reverse Expo I walk away with 1-2 new insights, products, and/or vendors that I may never have found otherwise.
What makes ICHP great?
ICHP is great because it provides a way for all of us to get involved in advocating for our profession. There are many changes and challenges in the future and ICHP helps us to ensure pharmacy needs are heard. It also provides diverse opportunities for leadership development and growth at many levels.
Is there an individual you admire or look up to, or a mentor that has influenced your career?
I have been fortunate to have had a group of strong role models and coworkers throughout my career. They have shown me how to be a leader through example, encouraged me to take on new challenges, engaged in vigorous discussions and debates, and supported me during tough times. Even when our professional paths have advanced on different courses, we have continued to keep in touch and support each other’s successes. Thank you to the UIC pharmacy team, the MetroSouth pharmacy team, the AdvocateAurora pharmacy and respiratory care teams, and the Rush University Medical Center pharmacy team for being outstanding colleagues!
What advice do you have for pharmacy students?
Don’t forget to start networking immediately and broadly. ICHP is a great place to begin networking within our profession. Meet a wide range of pharmacists and pharmacy technicians and then start networking outside of pharmacy. It’s important for nurses, physicians, and hospital leadership to understand how integral our role is to the success of the healthcare team. It’s also important for pharmacists to understand the perspectives and the roles of other professions in order better collaborate on patient care.
Do you have any special interests or hobbies outside of work?
Outside of work I am an avid hiker, camper and yogi. I love to go on long backwoods hikes and camping trips with my friends and family. A sky full of stars and a roaring campfire is my favorite way to spend a weekend.
What is the most interesting/unique fact about yourself that few people know?
I am also a yoga and meditation instructor! My favorite classes to teach are hatha and restorative yoga.
New Practitioners Network
The Power of Mentorship: A Student's Perspective of Connection and Advancement
by Michael Forst, Third Year Student Pharmacist University of Illinois at Chicago College of Pharmacy Co-President of UIC's College of Pharmacy Student Chapter, Chicago Campus
While an individual may accomplish immense achievements on his or her own, a mentor provides an invaluable experience of growth and development. Mentors share their time, expertise, and perspective in what could become a lifetime, transformational relationship. Mentors offer wisdom, encouragement, and leadership to allow individuals to become the best version of his or herself. Among others, a mentor’s role is to provide support, encouragement, and honest vision and insight. They aid in the development of leadership competencies and identify growth opportunities. As a result, a mentor will build a trusting and meaningful relationship with an individual as well as develop self-esteem, self-belief, and self-confidence. Ultimately, the impact of mentorship is seen through results achieved and relationships formed by the mentor and mentee.
As I began my pharmacy career at the University of Illinois at Chicago (UIC) College of Pharmacy, I had the mindset of creating a far-reaching network for myself within and outside the field of pharmacy. To embed myself within the UIC College of Pharmacy network, I focused my efforts on obtaining my first mentor within the faculty at UIC. Two years ago, the ICHP student chapter at UIC initiated a mentorship program throughout the Illinois Medical District and the city of Chicago. Pharmacists, residents, and students completed a questionnaire regarding organizational involvement, current occupation, and career and academic goals. The questionnaire allowed individuals to be paired based on similar attributes. This is in alignment with published data on pharmacy student mentorship programs. For example, a 2017 study analyzed students’ thoughts on a mentorship program. Seventy-seven percent of second year student pharmacists and 77% of fourth year student pharmacists who participated in a college of pharmacy mentorship program found the program to aid in professional growth.1 The study showed students benefited from a mentorship program and having a mentor was conducive to professional development.
The ICHP student chapter at UIC has directed its efforts to participating in the ICHP NPN Mentorship Program that includes students, residents, and pharmacists. All participants of the program can benefit because the program will occur throughout the entire state. As a student, I want both myself and my mentor to have a beneficial and productive connection. I want a mentor who is willing to commit to an engaged and enduring relationship, so I must establish that I want to remain engaged throughout multiple academic years and school breaks. I want my mentor to listen, push me to be the best version of myself, and embrace the idea that I can also help him or her develop and grow personally and professionally. A mentor should have a clear understanding of what the mentee wants to experience and accomplish. Both the mentee and mentor must have clear communication to allow both individuals to optimally understand personal and career ambitions. Clear communication also allows a mentor to help with the mentee’s actual goals and desires rather than focusing on what the mentor thinks the mentee wants. A mentor who strives for immense success of his or her mentee shows that he or she is supportive and encouraging. Establishing these sentiments early in the relationship allows both individuals to be honest with each other when offering advice and perspective. When a mentor and mentee view each other as a valuable resource for growth and development, both individuals may feel more encouraged to offer personal insight and perspective within and outside of pharmacy. Overall, the above qualities allow my mentor and I to engage in consistent, honest, and genuine conversations.
Upon participation in the ICHP NPN Mentorship Program, I will look to advance myself and my mentor to the best that I can. ICHP has an extremely far-reaching network, which will result in a mentoring program that promotes many perspectives within and outside the field of pharmacy. Each mentee and mentor will gain additional opportunities if they begin their pairing with a productive mindset. Mentees and mentors must establish clear desires, ambitions, and goals for themselves. In doing so, both individuals will naturally promote optimal outcomes. By actively participating in the relationship and seeking opportunities for evolvement, both the mentor and mentee will flourish.
Reference
Raub JN, Fiorvento A, Franckowiak TM, Wood T, Gortney JS. Implementing and sustaining a mentorship program at a college of pharmacy: The keys to successful mentorship. Curr Pharm Teach Learn. 2017;9(2):296-301. doi:10.1016/j.cptl.2016.11.017
Hi-Tech
Technician Hurdles
by Becky Ohrmund, CPhT, Pharmacy Technician Specialist; Northwestern Memorial Hospital; ICHP Technician Representative
What are some of the hurdles that you encounter as technicians? How do you overcome these hurdles? Do you want to be a part of a technician group, but your leadership doesn’t see the value?
For those of you who are able to participate in anything that you want, whether that is conferences, conference calls, or the ASHP Midyear, what advice do you have for those who want to participate but might not be able to because of cost or other barriers?
Throughout my career as a pharmacy technician, I have been lucky to have great leaders who are more than happy to allow me to attend conferences and conference calls while I am working. I am also able to integrate projects that I am working on outside of work into my work life. I know that not everyone is that lucky. With PTCB rolling out the new Advanced Credential I see this as a way for those who might not feel valued to really leverage for what they deserve. Now that the Annual Meeting has concluded, did you attend? If you did, you may have attended my presentation on Advanced Credentials. If you were not able to attend, please don’t hesitate to reach out to me via email and I can answer any questions you may have.
Also please don’t forget about our Technician Network. We are a new group and we need members. I want to hear from you and how we can make ICHP work for you. Currently I have a member reaching out to the chapter affiliates to see how they can include technician topics in affiliate programming as this particular issue was brought to my attention during a recent survey. I am also working on reaching out to pharmacy directors and leaders to encourage them to allow their technicians to get involved with ICHP and the Technician Network.
Are you an active ICHP member? Do you know anyone who you think would like to attend network calls and participate in other ICHP activities? Don’t hesitate to encourage them to join ICHP.
I know this article sounds like a giant commercial for ICHP. It’s ok if you think so as well. I do some of my best shopping based on commercials. How about you?
Public Education & Awareness Outreach Publication Subcommittee
PEARLS
by Scott Drabant, BS - Zoology/Chemistry; BS Pharmacy; President, Medication Therapy Analytica, Inc. Chair of ICHP PEARLS
The Public Education & Awareness outReach pubLication Subcommittee (PEARLS) is a new addition to ICHP. PEARLS originated from discussion at last year’s ICHP Leadership Retreat.
Traditionally, whenever medication is presented in the media, the image of the blue counting tray and a pharmacist counting by fives is depicted. At the ICHP Leadership Retreat the question was asked, “Is this the image we want the public to have of pharmacists?” And if this perception is not an accurate portrayal of the current role of health-system pharmacists, then what can be done to educate the general public on both public health information and the role of a health-system pharmacist?
PEARLS was formed under the Division of Marketing Affairs for the purpose of presenting clinical health information on various public health issues to the general public while also integrating the clinical role of health-system pharmacist into this information. Fourteen ICHP members joined PEARLS and developed the purpose, mission, objectives, and goals of the subcommittee.
The mission statement for PEARLS is for ICHP to be a conduit of clinical health information to the public including, but not limited to, medications, medical conditions, and preventative health measures. The subcommittee then formulated the following goals:
- Promote and expound on the role of pharmacists as healthcare providers
- Promote the role of the pharmacist as a source of clinical health information
- Promote ICHP as source of health information to the public
- Utilize all forms of communication (print, video, social media, etc.) to reach different demographics
- Develop a database of press releases, social media posts, etc. which will be available to ICHP members
PEARLS is already hard at work developing clinical education pieces to teach the public about the intricate work health-system pharmacists perform on a daily basis to optimize the medication outcomes of their patients.
PEARLS meets monthly and is developing the infrastructure to ensure all conent is peer reviewed and distributed by ICHP. For ICHP members who want to help prepare and review content, the subcommittee has developed a training guide to assist in sending out press releases/social media posts. This training guide recommends guardrails to ensure all educational materials meet the highest standards. Currently the committee is developing several draft social media posts/press releases. To fulfill the goal of having a bank of educational material (press releases/social media posts), the committee is inviting all pharmacists, pharmacy technicians, pharmacy residents and pharmacy students to write press releases and/or social media posts based on their specific expertise (e.g., diabetes, cardiology, pediatrics, women’s health, etc). Volunteers are most welcome to share their talents in preparing, peer reviewing, or distributing material in various media formats. The educational material may be clinical in nature, and/or address timely or seasonal issues. Current event topics will arise from time to time, but having a bank of material will allow for continuous dissemination of educational information to the public.
We invite all ICHP members to contribute to the efforts of PEARLS as authors or reviewers of draft press releases or social media posts. If interested, please contact the ICHP office at:
members@ichpnet.org.
Attention ASHP Pharmacist Members
It's Time To Elect Delegates for ASHP's House
by Scott A. Meyers, Executive Vice President
The ASHP Summer meeting for 2021 will hopefully be held in Long Beach, California from June 5-9 and in 2022 it will be in Phoenix, AZ from June 11-15! It’s the first time for both of these cities to ever be sited for this annual event! ICHP needs to elect three delegates to join Bernice Man and Charlene Hope as the Illinois delegation for 2021 and then continue on in 2022. ASHP’s House of Delegates is the policy making body within ASHP and is responsible for approving all ASHP position statements and practice guidelines. While currently the meeting is planned as an in-person event, we have learned from this year that this can change.
Delegate candidates must be ASHP pharmacist members who plan on attending the ASHP Summer Meetings for both 2021 and 2022 at their own expense. In addition, they must attend one of the Rosemont-based Regional Delegate Conferences typically held each year in late April or early May (for which delegates and alternate delegates will be reimbursed by ICHP for their expenses). Interested individuals should provide their own nomination via e-mail, fax or mail to the ICHP office by November 15, 2020.
Nominees must provide nomination statements (limited to 250 words or less), which include years of membership in ASHP, current employment position, pharmacy association memberships, volunteer experiences related to pharmacy associations, and any other relevant information the potential candidate would like to include. The ICHP Committee on Nominations will select up to six candidates for this year’s ballot. The two candidates receiving the highest vote totals will be credentialed as delegates for 2021 and 2022 and the remaining candidates will serve as alternate delegates for 2021 only.
This is a great opportunity for someone who has served at the state level for some time and wishes to move up within ASHP. It is probably not a good match for someone with no pharmacy association volunteer experience.
Elections will be held at the end of November, with all ASHP pharmacist members eligible to vote on-line. Election results will be announced in the February KeePosted. Interested individuals should send their letter of intent and candidate’s statement to Scott Meyers by November 15th, at the ICHP office via fax at (815) 227-9294 or e-mail to
scottm@ichpnet.org.
Educational Affairs
Call for Posters!
Are you working on a project that others could learn from?
Please consider sharing the outcomes with your colleagues at the poster session during the ICHP/MSHP Virtual Spring Meeting March 19-20, 2021. This is a great opportunity to share innovative ideas with others and learn about trends in Illinois health-system pharmacies.
Categories/Presentations/Eligibility:
All ICHP members are eligible to submit abstracts to be considered for presentation at the Spring Meeting.
Submission:Members wishing to submit a poster should use the online submission form. Be sure to click "Submit" after completing your form. The deadline for submissions is January 10, 2021. Please direct any questions to Trish Wegner at
TrishW@ichpnet.org.
Deadlines:
Submission deadline is January 10, 2021. Authors will be notified of acceptance of their poster via email in February 2021.
More information will be available at a later date.
Criteria determined by the Division of Educational Affairs
Educational Affairs
Let's talk about it: Health Equity, Racism, and Cultural Humility
by Klodiana Myftari, PharmD, BCACP Assistant Professor of Pharmacy Practice; Midwestern University Chicago College of Pharmacy; Sally Arif, PharmD, BCPS, BCCP Associate Professor of Pharmacy Practice; Midwestern Univer
The year 2020 has really highlighted our limitations as a society, exacerbated our fears and insecurities, and shined a spotlight on inequity. Over the last several months, many of us have paused and asked, “How did we get here?” For many, including some of our patients, the fear, insecurity, and disparities have been present for generations. The current year has simply made things more visible and brought to light the work that needs to be done to combat racism and its impact on healthcare.
Health equity, defined as the opportunity for everyone to attain their highest level of health, is a concept that is taught in every healthcare professional school.1 However, it is not always understood and is difficult to implement. Health equity cannot exist without racial and social justice. Unfortunately, disparities fundamentally fueled by race/ethnicity, gender, sexual orientation/gender identity, and disability status, persist across our nation. Racism and long-term discrimination have precipitated social and economic issues that are pillars of health inequity. “Racism” is a system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call “race”) that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources.2 This definition speaks to a system designed by individual social interpretation of assigned value. The question we should all ask ourselves is, “What is my individual interpretation of assigned value based on how one looks?” This self-reflection moves the conversation from the system to the individual. We must challenge ourselves to think beyond our role as a healthcare provider to our moral responsibility as individuals when it comes to serving those who are marginalized in our society. This challenge starts by gaining self-awareness and reflecting on our individual journey towards cultural humility.
Cultural Humility, Self-Awareness, and Biases
Cultural humility is part of lifelong learning that requires consistent self-reflection. It can be defined as the “ability to maintain an interpersonal stance that is other-oriented (or open to the other) in relation to aspects of cultural identity that are most important to the [person].”3 The journey towards cultural humility starts with self-awareness, which is a key component of cultural awareness. Understanding our own values, beliefs, norms, and customs also comes with uncovering what stereotypes and biases we may unintentionally carry.
Healthcare professionals have been found to have the same degree of implicit bias - otherwise known as unconscious bias- as the general population.4 Unlike explicit biases, of which one is aware, implicit biases exist in the subconscious, are learned by associations over a lifetime, and can unintentionally contribute to unequal care of disadvantaged populations. They can lead to quick judgments about others and are often rooted in unsupported assumptions about race, ethnicity, socio-economic status, sexual orientation, or gender. The good news is that many of our implicit biases do not align with our outward explicit values or feelings; however, they can still unconsciously influence the degree of active listening and empathy we may provide to our patients. Unconscious biases can unintentionally lead to the under-treatment of pain, cardiovascular disease, asthma, and mental health, especially for racial minorities.
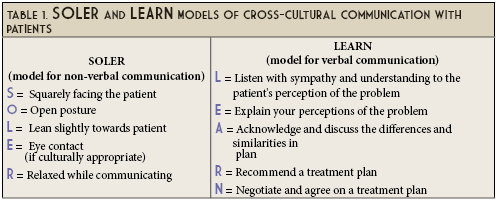
Cross-Cultural Communication
Engaging with “others” who are different from you is a de-biasing strategy that can assist with reducing negative stereotypes that can impact interactions with patients.5 Cultural identity is central to all patient interactions. However, culture goes beyond the obvious characteristics of race, ethnicity, gender expression, and language to include deeper parts of our identities such as belief systems, world views, and attitudes. Understanding a patient’s culture, which dictates human behavior and action, allows us to build a better rapport and uncover health beliefs that can impact adherence with health plans. Enhancing our cross-cultural communication skills requires practice and time. Models such as SOLER and LEARN provide strategies to cultivate genuine, culturally sensitive relationships with our patients.6,7 (See Table 1).
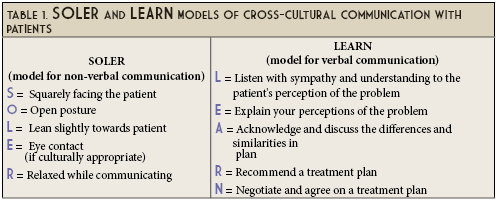
Cross-cultural communication strengthens our cultural awareness. It is a catalyst on one’s journey toward cultural humility. As individuals and healthcare providers, we move from cultural awareness to cultural knowledge when we are able to analyze the similarities and differences between our culture and that of others.8 Conversations with our patients and fellow healthcare professionals around values and beliefs that affect one’s health moves us towards cultural sensitivity. Finally, cultural competency is when we can adjust how we think and behave to support our diverse patients.8
Our challenge in the path towards cultural humility, health equity, and anti-racism will be to continue the conversations without these words losing their true meaning. Keep talking and asking uncomfortable questions. Let us continue the journey toward cultural humility together. It is our responsibility as healthcare professionals to recognize and challenge power imbalances and demand institutional accountability for all our patients.9
References
- American Public Health Association. Health Equity. Available at https://www.apha.org/topics-and-issues/health-equity. Accessed October 6, 2020.
- Jones CP. Toward the science of practice of antiracism: launching a national campaign against Racism. Ethn Dis. 2018;28(suppl 1):231-234.
- Hook JN, Davis DE, Owen J, Worthington EL, Utsey SO. Cultural humility: measuring openness to culturally diverse clients. J Couns Psychol. 2013;60(3):353-366. [published correction appears in J Couns Psychol. 2015 Jan;62(1):iii-v].
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. J Exp Soc Psychol. 2012;48(6):1267-1278.
- Berlin EA, Fowkes WC. A teaching framework for cross-cultural health care. W J Med. 1983, 139:934-938.
- Egan G. The skilled helper: a problem management and opportunity approach to helping. Pacific Grove, CA: CambridgeBrooks/Cole; 2002.
- The Winters Group, Inc. Cultural Competence ModelTM. Available at: http://www.theinclusionsolution.me/what-is-inclusion-part-2-inclusion-starts-with-i/. Accessed October 6, 2020.
- Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117-125.
Educational Affairs
Use of Direct Oral Anticoagulant Medications For Atrial Fibrillation: Current Recommendations in Valvular Heart Disease
by Brian Cryder, PharmD, BCACP, CACP Associate Professor and Clinical Pharmacist; Midwestern University Chicago College of Pharmacy and Advocate Medical Group; Austin Ballew, PharmD, BCPS Ambulatory Care Clinical Pharmacist; Advocate Medical Group (Sykes Center)
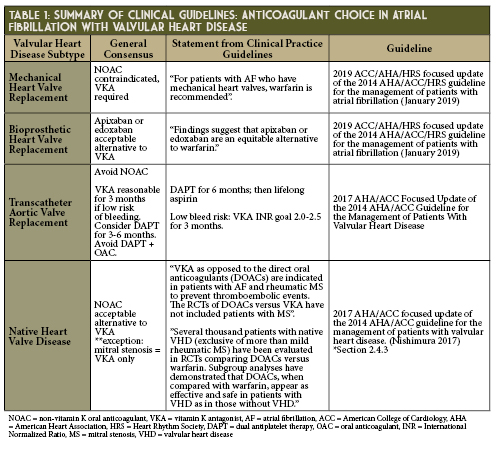
Alternatives to warfarin have been long sought as more practical and safer options for stroke prevention in patients with atrial fibrillation (AF). As oral direct thrombin inhibitors and factor Xa inhibitors were introduced for use in the United States - starting with dabigatran’s approval in 2010 - it has been with the caveat of “non-valvular” atrial fibrillation. However, which specific heart valve conditions contraindicate the use of direct oral anticoagulants (DOACs) has not been consistently delineated in medical practice. Guidelines from the American Heart Association and American College of Cardiology1-2 provide recommendations regarding the choice of oral anticoagulant in many patient subgroups with concomitant AF and valvular heart disease (VHD), but the emergence of transcatheter aortic valve replacement (TAVR) has added a new wave of evidence to consider. (See Table 1). This article aims to outline considerations when using DOACs in the treatment of valvular AF.
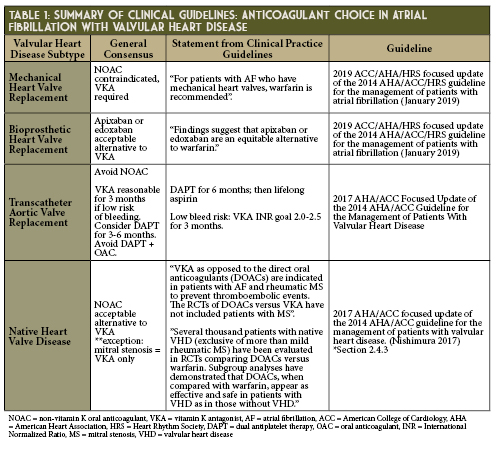
Mechanical Prosthetic Heart Valves
Warfarin has long been the sole oral anticoagulant used in patients with mechanical prosthetic valve (MPV) replacements, but in the past decade DOACs have been studied as an alternative. To date, no past DOAC studies have included patients with concomitant AF and MPV.
The phase 2 RE-ALIGN study sought to compare dabigatran (dosed to meet plasma trough levels > 50 ng/ml) to warfarin.3 RE-ALIGN primarily aimed to study the pharmacokinetics of dabigatran in this population, but the trial required early discontinuation due to excess in both thromboembolic and hemorrhagic complications when compared to warfarin. Researchers now attribute this therapeutic failure to localized thrombin generation triggering thrombosis in MPV-associated clotting rather than tissue factor as seen in non-valvular atrial fibrillation (NVAF) and venous thrombosis.3-5 Jaffer and colleagues discovered that MPV required dabigatran concentrations > 200 ng/ml to suppress thrombin generation to the same extent that warfarin does when maintained at INR levels between 2.0-3.5 thus RE-ALIGN’s target of 50 ng/ml was insufficient.4
More recently, researchers have tested the theory that moving upstream in the clotting cascade to factor Xa inhibition may have greater success in mitigating MPV-associated thrombosis, such as the common practice of using low molecular weight heparins when a patient cannot take warfarin.6-11 Small studies (< 10 patients) and case series utilizing apixaban or rivaroxaban have shown mixed results, but enough positive outcomes for investigators to initiate plans for a larger phase 2 trial comparing rivaroxaban 15 mg twice daily to warfarin.6-11
In vitro laboratory testing performed with apixaban and rivaroxaban revealed that neither anticoagulant suppressed thrombin generation sufficiently at clinically relevant concentrations.12 However, when Xa and thrombin were inhibited simultaneously (rivaroxaban and dabigatran in this investigation) effectiveness was improved, possibly explaining why heparin derivatives remain effective in clinical practice. This leads many investigators to be pessimistic that rivaroxaban or apixaban alone will consistently provide sufficient anticoagulant coverage.
Bioprosthetic Heart Valves
DOACs may have a place in therapy for patients with AF and bioprosthetic valves (BPV). Bioprosthetic valves are considered to be less thrombogenic than MPV and guidelines recommend short term anticoagulation (3-6 months) with VKA plus long term aspirin to discourage valve thrombosis.1-2
Initial data for DOAC use in patients with BPV and AF was limited since it came from the small subgroup analyses of the ARISTOTLE13 and ENGAGE-AF-TIMI 4814 trials, but a later meta-analysis15 pooled a more substantial cohort for analysis. Compared to VKA, DOACs demonstrated reduction of stroke and systemic embolization (0.59 HR [0.13-2.69 95%CI]), lower risk of major bleeding (0.67 HR [0.27-1.63 CI]) and decreased all cause mortality (0.82 HR [0.24-2.81 CI]). In a combined safety analysis with BPV and VHD, intracranial hemorrhage (0.46 HR [0.24-0.86 CI]), myocardial infarction (0.70 HR [0.50-0.99 CI], and major adverse cardiovascular events (0.91 HR [0.81-1.01 CI]) were reduced in the DOAC groups. The overall findings of the analysis in BPV mirror the larger population of patients with VHD. While all DOACs were similar in reducing stroke or systemic embolism (SSE), edoxaban 30 mg was associated with less bleeding and rivaroxaban was associated with increased risk of major bleeding including intracerebral hemorrhage (ICH).
These findings are congruent with the recently updated guidelines. Based on evidence provided, anticoagulation with apixaban or edoxaban in patients with AF after bioprosthetic valve replacement is reasonable as supported by the AHA 2019 focused update on Atrial Fibrillation guideline.2
Transcatheter Aortic Valve Replacement
Use of Transcatheter Aortic Valve replacement (TAVR) has increased rapidly from 2.6% of all patients admitted with aortic valve disease in 2012 up to 12.5% of admissions in 2016.16 Approximately 40% of patients requiring TAVR frequently have pre-existing AF or develop new-onset AF post-operatively; both groups carrying increased mortality risk after TAVR.17 Current guidelines recommend a combination of antiplatelet and oral anticoagulation to reduce valve leaflet thrombosis after TAVR.1 These recommendations are supported by limited data, so elucidating preferred antithrombotic options from emerging clinical studies should be prioritized. One limiting factor in applying existing data is that many studies - such as GALILEO18 and ADAPT-TAVR19 - exclude patients with pre-existing indications for anticoagulation, such as AF. Two ongoing studies that included AF patients are the ATLANTIS20 and ENVISAGE-TAVI AF.21
The GALILEO study did not show favorable outcomes for DOACs as it was terminated early due to increased risk of bleeding (1.50, 95% CI 0.95-2.37) and mortality (1.69, 95% CI 1.13-2.53) with rivaroxaban in patients without a pre-existing indication for anticoagulation. A study by Seeger and colleagues revealed that at thirty days post-operatively, patients with AF taking aspirin and apixaban were less likely to develop life threatening bleeding (3.5% vs 5.3% p<0.01) and had fewer early safety endpoints (13.5% vs. 30.5% p< 0.01) compared to VKA.22 Another smaller study including patients undergoing TAVR with preexisting indications for anticoagulation (not exclusively AF) showed no significant difference in combined endpoint of death, stroke, embolism and bleeding between the DOAC and VKA groups (11% vs. 0.8%, p = 0.45).23 The data trends favored DOAC use over VKA, but was underpowered to produce statistically significant differences.
While there are suggestions of improved bleeding risk with DOAC compared to current practices, further studies are needed to explore duration of therapy and longer observation times while on DOAC therapy. Careful consideration should be taken regarding patient’s thrombotic and bleeding risk. The next year will bring results from a few large randomized controlled trials and may help shed light on this topic.
Native Valve Pathologies
Despite the “non-valvular” inclusion criteria to the large-scale DOAC clinical trials, there were several VHD subtypes that were represented in the study populations. From the combined cohorts of ARISTOTLE, ENGAGE-AF-TIMI 48, RE-LY, and ROCKET AF there were 10,633 patients with mitral regurgitation, 324 patients with mild mitral stenosis, 2,559 patients with aortic regurgitation, 1,238 patients with aortic stenosis, and 3,303 patients with tricuspid regurgitation.24 A meta-analysis of these four studies showed that in the cohort of VHD patients with AF, DOACs were not significantly different from warfarin in outcomes of overall mortality rate (HR 1.01, 95% CI 0.91-1.12) and major bleeding (HR 0.93, 95% CI 0.67-1.28). DOACs collectively were better than warfarin in reduction of SSE (HR 0.70, 95% CI 0.60-0.82) similar to what was seen in the strictly non-valvular heart disease population. Real-world studies have also demonstrated positive outcomes in both the Medicare population25 and a Midwest United States single- center outpatient cardiology practice.26 This data further reinforces the AHA/ACC recommendation “It is reasonable to use a DOAC as an alternative to a VKA in patients with AF and native aortic valve disease, tricuspid valve disease, or MR and a CHA2DS2-VASc score of 2 or greater.”1
Conclusion
Over the next decade, as the DOAC patents expire and become financially accessible to a larger pool of patients, it will be important to ensure efficacy and safety in the appropriate patient population. Few experts anticipate major changes in current guidelines for DOAC use in MPV, BPV and most VHD, but post-TAVR anticoagulation will be shaped largely by the arrival of new research over the next several years.
References
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 2017; 135: e1159-e1195. DOI: 10.1161/CIR.0000000000000503
- January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. Circulation 2019; 140: e125-e151. DOI: 10.1161/CIR.0000000000000665
- Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013; 369: 1206-1214. DOI: 10.1056/NEJMoa1300615
- Jaffer IH, Stafford AR, Fredenburgh JC, et al. Dabigatran is less effective than warfarin at attenuating mechanical heart valve-induced thrombin generation. J Am Heart Assoc. 2015; 4: e002322. DOI: 10.1161/JAHA.115.002322
- Chan NC, Weitz JI, Eikelboom JW. Anticoagulation for mechanical heart valves: Will oral factor Xa inhibitors be effective? Arterioscler Thromb Vasc Biol 2017; 37: 743-745. DOI: 10.1161/ATVBAHA.117.309223
- Lester PA, Coleman DM, Diaz JA, et al. Apixaban versus warfarin for mechanical heart valve thromboprophylaxis in a swine aortic heterotopic valve model. Arterioscler Thromb Vasc Biol 2017; 37: 942-948. DOI: 10.1161/ATVBAHA.116.308649
- Roost E, Weber A, Alberio L, et al. Rivaroxaban in patients with mechanical heart valves: A pilot study. Thrombosis Research 2020; 186: 1-6. DOI: 10.1016/j.thromres.2019.12.005
- Duraes AR, Bitar YSL, Lima MLG, et al. Usefulness and safety of rivaroxaban in patients following isolated mitral valve replacement with a mechanical prosthesis. Am J Cardiol 2018; 122: 1047-1050. DOI: 10.1016/j.amjcard.2018.06.015
- Duraes AR, Bitar YSL, Filho JA, et al. Rivaroxaban versus warfarin in patients with mechanical heart valve: rationale and design of the RIWA study. Drugs in R&D 2018; 18: 303-308. DOI: 10.1007/s40268-018-0249-5
- Carvalho Silva DM, Braga A, de Jesus I, Neves J. Mechanical prosthetic heart valve thrombosis in a patient receiving rivaroxaban. Cardiology 2019; 143: 116-120. DOI: 10.1159/000501361
- Kumar V, Kelly S, Raizada A, et al. Mechanical valve thrombosis on rivaroxaban: Are novel anticoagulants really an option? Methodist Debakey Cardovasc J 2017; 13 (2): 73-75. DOI: 10.14797/mdcj-13-2-73
- Jaffer IH, Fredenburgh JC, Stafford A, Whitlock RP, Weitz JI. Rivaroxaban and dabigatran for suppression of mechanical heart valve-induced thrombin generation. Ann Thorac Surg 2020; epub ahead of print. DOI: 10.1016/j.athoracsur.2019.10.091
- Guimaraes PO, Pokorney SD, Lopes RD, et al. Efficacy and safety of apixaban vs warfarin in patients with atrial fibrillation and prior bioprosthetic valve replacement or valve repair: Insights from the ARISTOTLE trial. Clinical Cardiology 2019; 42: 568-571. DOI: 10.1002/clc.23178
- DeCaterina R, Renda G, Carnicelli AP, et al. Valvular heart disease patients on edoxaban or warfarin in the ENGAGE AF-TIMI 48 trial. J Am Coll Cardiol 2017; 69 (11): 1372-1382. DOI: 10.1016/j.jacc.2016.12.031
- Malik AH, Yandrapalli S, Aronow WS, Panza JA, Cooper HA. Oral anticoagulants in atrial fibrillation with valvular heart disease and bioprosthetic heart valves. Heart 2019; 105: 1432-1436. DOI: 10.1136/heartjnl-2019-314767
- Goldsweig AM, Tak HJ, Chen LW, et al. The evolving management of aortic valve disease: 5-year trends in SAVR, TAVR and medical therapy. Am J Cardiol 2019; 124: 763-771. DOI: 10.1016/j.amjcard.2019.05.044
- Sherwood MW, Vora AN. Challenges in aortic stenosis: Review of antiplatelet/anticoagulant therapy management with transcatheter aortic valve replacement (TAVR): TAVR with recent PCI, TAVR in the patient with atrial fibrillation, and TAVR thrombosis management. Curr Cardiol Rep 2018; 20: 130. DOI: 10.1007/s11886-018-1073-9
- Dangas GD, Tijssen JGP, Wohrle J, et al. A controlled trial of rivaroxaban after transcatheter aortic-valve replacement. N Engl J Med 2020; 382: 120-9. DOI: 10.1056/NEJMoa1911425
- Park DW. Anticoagulation versus dual antiplatelet therapy for preventing leaflet thrombosis and cerebral embolization after transcatheter aortic valve thrombosis (ADAPT-TAVR). Retrieved from: https://clinicaltrials.gov/ct2/show/record/NCT03284827?view=record
- Collet JP, Berti S, Cequier A, et al. Oral anti-Xa anticoagulation after trans-aortic valve implantation for aortic stenosis: The randomized ATLANTIS trial. Am Heart J 2018; 200: 44-50. DOI: 10.1016/j.ahj.2018.03.008
- Van Mieghem NM, Unverdorben M, Valgimigli M, et al. Edoxaban versus standard of care and their effects on clinical outcomes in patients having undergone transcatheter aortic valve implantation in atrial fibrillation - Rationale and design of the ENVISAGE-TAVI AF trial. Am Heart J 2018; 205: 63-9. DOI: 10.1016/j.ahj.2018.07.006
- Seeger J, Gonska B, Rodewald C, Rottbauer W, Wohrle J. Apixaban in patients with atrial fibrillation after transfemoral aortic valve replacement. J Am Coll Cardiol Intv 2017; 10: 66-74. DOI: 10.1016/j.jcin.2016.10.023
- Geis NA, Kiriakou C, Chorianopoulos E, Uhlmann L, Katus HA, Bekeredjian R. NOAC monotherapy in patients with concomitant indications for oral anticoagulation undergoing transcatheter aortic valve implantation. Clin Res Cardiol 2018; 107: 799-806. DOI: 10.1007/s00392-018-1247-x
- Pan KL, Singer DE, Ovbiagele B, et al. Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: A systematic review and meta-analysis. J Am Heart Assoc 2017; 6:e005835. DOI: 10.1161/JAHA.117.005835
- Briasoulis A, Inampudi C, Akintoye E, Alvarez P, Panaich S, Vaughn-Sarrazin M. Safety and efficacy of novel oral anticoagulants versus warfarin in medicare beneficiaries with atrial fibrillation and valvular heart disease. J Am Heart Assoc 2018; 7: e008773. DOI: 10.1161/JAHA.118.008773
- Hampton ML, Tellor KB, Armbruster AL, Theodos G, Schwarze MW. Evaluation of the safety and effectiveness of direct-acting oral anticoagulants in patients with atrial fibrillation and coexisting valvular heart disease. Am J Cardiovasc Drugs 2020; Epub ahead of print. DOI: 10.1007/s40256-020-00398-x
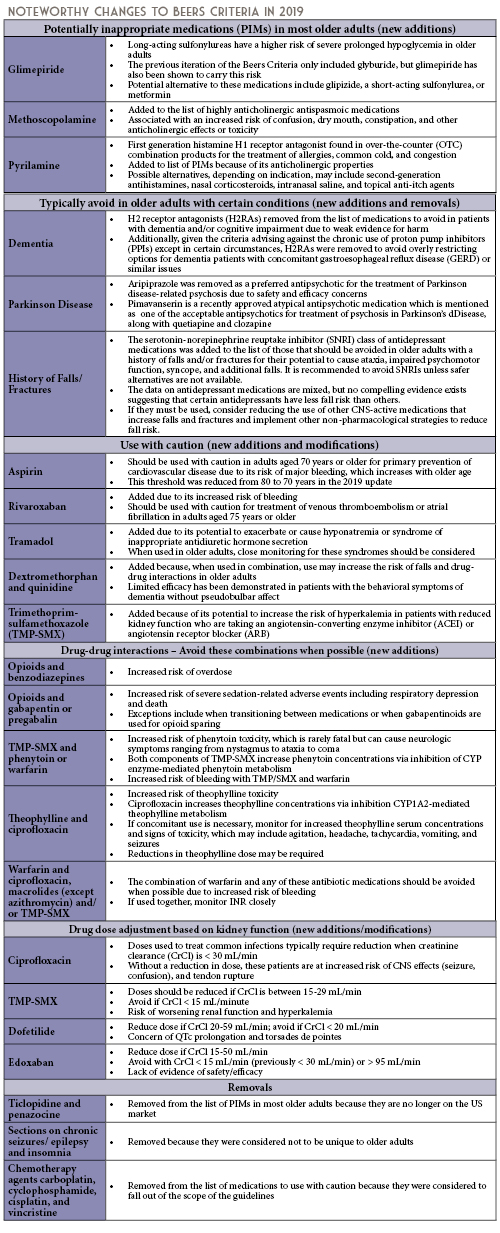
Educational Affairs
BEERS Criteria 2019 Update: A Summary of Notable Changes
by Candace Bishop, PharmD, MPH PGY2 Pharmacy Administration Resident; Advocate Aurora Health, Lutheran General Hospital; Jen Phillips, PharmD, BCPS, FCCP, FASHP; Associate Professor; Midwestern University Chicago College of Pharmacy
Older Adults and Medication Use Safety
As the proportion of the United States population over the age of 65 years continues to grow, it is imperative that healthcare providers recognize and understand the intricacies of caring for older adults.1 As part of the normal aging process, a number of changes occur in the human body. Among these changes are pharmacokinetic (PK) and pharmacodynamics (PD) effects of medications. One of the most clinically relevant changes is a decline in renal elimination pathways and liver metabolism of certain medications.2 These changes often necessitate dose reductions based on the function of these vital organs. Regarding pharmacodynamics, older adults are generally more prone to exaggerated responses to medications, more commonly side effects than therapeutic effects.2 This is especially true for medications affecting the central nervous system. Because of these PK and PD changes, it is vital that healthcare professionals be especially vigilant in monitoring older adults for both therapeutic and adverse effects of medications.
In addition to the PK and PD changes that naturally occur over the life course, additional factors have been identified as negatively affecting the medication use safety of elderly patients. One of these medication safety issues is polypharmacy, which is defined as taking 5 or more medications at one time.3 Polypharmacy affects approximately 30% of older adults in developed countries.3 In the United States, older adults purchase 33% of all prescription drugs despite making up only 14.5% of the US population. This proportion of prescription purchasing is expected to increase to 50% by the year 2040.3 Polypharmacy has been associated with worsening of geriatric syndromes and adverse drug events. Additionally, complex medication regimens heighten the potential for drug-drug interactions, which can cause additional adverse reactions with a wide range of severity.
Given the aforementioned challenges in caring for older adults, there are some medications that should generally be avoided in all older adults, and some that should be avoided or modified in certain older adult populations. These are outlined in the Beers Criteria, which is an explicit list of potentially inappropriate medications that are typically best avoided in adults aged 65 years or older.4 Updates to these criteria are produced by the American Geriatrics Society (AGS) on a 3-year cycle, with the most recent update published in April 2019. The 2019 update represents the 5th update since the original list was published in 1991. The intent of the Beers Criteria is to improve medication selection by clinicians in patients aged 65 years or older, reduce adverse drug events in these patients, and to serve as a tool for evaluating the quality of care, cost, and patterns of drug use in older adults.4 The criteria are categorized into 5 types, and noteworthy changes for each criterion since the last published edition are outlined in the following sections.
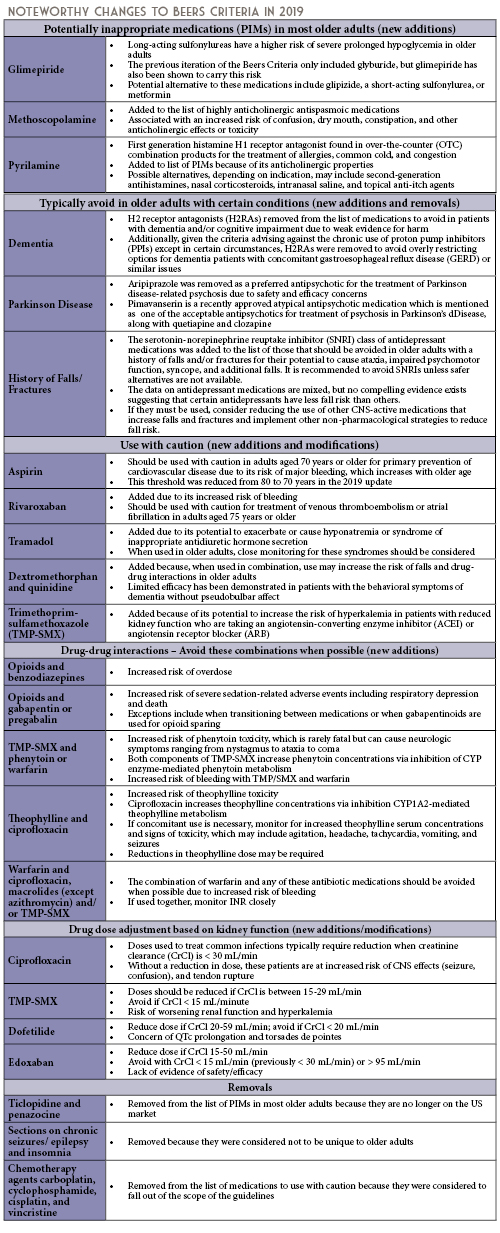
Pharmacist Roles in Ensuring the Medication Safety of Older Adults
The AGS Beers Criteria are intended to be applied to the care of older adults in all ambulatory, acute, and institutionalized settings except for hospice and palliative care settings.4 Using the Beers Criteria in combination with clinical judgment is essential. There may be situations when medications on this list may need to be administered due to clinical situations. In these instances, the risk to benefit ratio should always be considered.
Pharmacists are uniquely poised as the most accessible healthcare providers, with the ability to influence the care of older adult patients in all of these settings. Potential strategies for pharmacist intervention include: suggesting alternative medications, reducing doses, and/or recommending shorter courses of therapy, when appropriate. For OTC medications, pharmacists should consider whether it is appropriate to continue scheduled or as needed dosing at home during care transitions, given that there may be less monitoring at home, less supervision and oversight, and less control of the environment. Pharmacists in community or ambulatory care settings can assist older adults in choosing appropriate OTC medications, avoiding combination products with certain ingredients, and providing counseling to monitor for adverse effects.
Armed with their clinical knowledge, expertise, and guidance from the AGS, pharmacists can assist in improving medication selection, educating clinicians and patients, and reducing adverse drug events due to potentially inappropriate medications in older adults.
References
- Sade RM. The graying of America: challenges and controversies. J Law Med Ethics. 2012;40(1):6-9.
- Delafuente JC. Pharmacokinetic and pharmacodynamic alterations in the geriatric patient. Consult Pharm. 2008;23(4):324-334.
- Kim J, Parish AL. Polypharmacy and medication management in older adults. Nurs Clin North Am. 2017;52(3):457-468.
- 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
Professional Affairs - CPE Opportunity!
Pharmacist Role in a Pediatric Lupus Clinic (Best Practice Award Winner)
by Shannon M Rotolo, PharmD, BCPS, Clinical Pharmacy Specialist, UChicago Medicine, Chicago, IL; Grace Lynn Cameron, PharmD, Clinical Pharmacy Specialist, UChicago Medicine, Chicago, IL; Constantina Talevski, BA, CPhT, Ambulatory Medication Access Coordinator, UChicago Medicine Chicago, IL
Introduction, Purpose, and goals of the program
Pediatric systemic lupus erythematous (SLE) is an autoimmune disease in which the body produces pathogenic autoantibodies that cause inflammation and tissue damage.1,2 Children with pediatric SLE often require complex regimens of immunosuppressive medications to control the disease and prevent flares.3 In recent years, the incorporation of pharmacists as a part of the ambulatory care team for patients with chronic conditions, including cystic fibrosis, HIV, and others, has been described in the literature.4,5,6 The benefits vary depending on the patient population and setting, but pharmacists have been shown to improve patient and physician satisfaction, improve patients’ medication understanding and adherence, and decrease drug or vaccine related errors.7 Our institution established a Pediatric Complex Lupus Clinic in January 2019. Patients (term refers to patients, families and/or caregivers) of this clinic were scheduled to meet with a multidisciplinary care team, including a pharmacist, at their initial visit and subsequent quarterly visits. Although there is literature regarding pharmacist interactions and interventions with patients who have rheumatologic diseases, it is confined primarily to inpatient or specialty pharmacy settings, and often focused on an adult patient population.8,9,10 The purpose of this project is to describe the ambulatory pharmacist’s role in a Pediatric Complex Lupus Clinic and the impact of pharmacist involvement in clinic on patient care.
Description of the Program
Patients were scheduled for time with a pharmacist during their clinic appointments. Multiple visits were booked for the same start time, and the various care team members, including a research assistant, social worker, clinical pharmacist, advanced nurse practitioner, and attending physician rotated between rooms. When warranted, the patient’s schedule for the day might also include laboratory time for necessary blood work or an attending nephrologist. At the completion of the visits, all patients and families were encouraged to attend support groups coordinated by the Child Life Team. Two rooms were reserved: one for a patient only support group and one for a family/caregiver support group.
The amount of scheduled time with the pharmacist during an initial visit ranged from 20-30 minutes. This variation was due to adjustments made to the overall clinic workflow during the first several months. The actual time required to complete the initial pharmacist visit ranged from 7 to 40 minutes. Each patient was provided a pill organizer during the initial pharmacist visit. Pharmacist assessments were performed at initial and follow-up visits, and included medication reconciliation, adherence review, and medication management tasks review. Questions on the medication management tasks questionnaire (Figure 1) were age-based, and modified from a tool previously used in the Pediatric Cystic Fibrosis Clinic. Patients were given the opportunity to ask questions. If appropriate, medication management task “homework” was assigned to encourage patients to practice an additional 1-2 age-appropriate tasks prior to the time of the next visit. All patients were offered the option of transferring their prescriptions to the on-site outpatient pharmacy, which offers in-person pick-up or mail order services (e.g., refill reminder calls and free delivery). Additionally, the pharmacy team enrolled eligible patients in financial assistance programs such as manufacturer copayment savings cards, manufacturer patient assistance programs for free drug, or non-profit charity-based financial assistance programs.
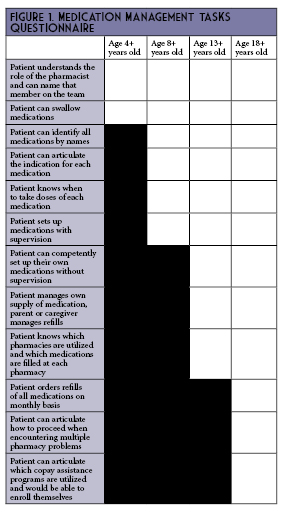
The clinic was scheduled for a half-day each week, accounting for approximately 4 hours of pharmacist time. The team also conducted weekly meetings for 1 hour as a pre-huddle for the upcoming week and post-clinic discussion, in addition to using this time to touch base about on-going research, quality improvements, or other planned activities (e.g., fundraisers or patient and family events). In preparation for clinic each week, the pharmacist reviewed the patient’s chart and obtained a refill history, which accounted for an additional 1 hour of effort on average. This total time equated to a 0.15 FTE dedicated to supporting this new service line.
Experience with and Outcomes of the Program
Among the 34 patients seen by a pharmacist during the 12 month study period, the median patient age was 16 years old (range 5 to 20 years old), 88.2% were female, and 47.1% were Black (Table 1). Across all visits, a barrier to medication access or affordability was identified 41% of the time (Table 2). Although the study was insufficiently powered, medication adherence did improve with subsequent pharmacist visits. At the time of the first appointment, only 67.7% of patients or parents/caregivers reported already having a relationship with a pharmacist (Table 3). The most common pharmacist education topics were review of indication for drug(s) and bone health recommendations. The most common pharmacist interventions were weight-based dose adjustment of hydroxychloroquine and de-escalation of long-standing stress ulcer prophylaxis (SUP) regimens.
Discussion of Innovative Aspects of Programs and Achievement of Goals
This is the first Pediatric Complex Lupus Clinic in the state of Illinois with a multidisciplinary model that includes a pharmacist. Our team was able to predefine the pharmacist role in this setting based on collaboration and input from other pediatric clinics at our site that already incorporate a pharmacist, such as the Cystic Fibrosis Center, and outside institutions with a Pediatric Complex Lupus Clinic supported by clinical pharmacy services, such as Nationwide Children’s Hospital in Columbus, Ohio.
A majority (75%) of questions or concerns about medication regimens were expressed to the pharmacist on the first visit, but the on-going presence of these questions through the 4th follow-up visit and persistence of barriers related to medication access /affordability reinforced our decision to have a pharmacist evaluation as a recommended component at all follow-up visits, instead of an initial pharmacist screen only.
The most common pharmacist education topics – review of indication for drug(s) and bone health recommendations – highlight the lack of prior exposure to pharmacists and dietitians for many of these patients. This is consistent with previous literature suggesting that few pediatric patients interact with community pharmacists,11 and a lack of pharmacist or dietitian involvement in the pediatric rheumatology clinic prior to the establishment of the Pediatric Complex Lupus Clinic and accompanying multidisciplinary care team. These findings were likely also influenced by the decision not to include a dietitian as part of the care team during this pilot period.
The most common pharmacist interventions – weight-based dose adjustment of hydroxychloroquine and de-escalation of long-standing SUP regimens – are also somewhat unsurprising. The American Academy of Ophthalmology updated their guidelines on the maximum recommended weight-based dose of hydroxychloroquine from 6.5 mg/kg to 5 mg/kg in 2016, based on increased risk of ocular toxicity with higher doses.12 While there was a modest decline in prescribed doses following those recommendations, higher doses remain prevalent even in 2018.13 In terms of stress ulcer prophylaxis, there is limited literature to evaluate this practice in pediatric populations outside of the pediatric intensive care unit, which likely contributes to variation in prescribing practices. Future projects for this clinic may include development of a protocol for SUP initiation and de-escalation.
Our study is limited by a small sample size and a low number of patients who completed all four quarterly visits with a pharmacist during the 12 month study period. Despite these limitations, we did see a numerically higher percentage of patients completing medication management tasks and improvements in medication adherence. Additional limitations include incomplete data on monthly prescription copayment amounts for patients who filled at outside pharmacies prior to the initial visit, all patients not completing the recommended four quarterly visits during the study timeline, and variability in the number of pharmacy staff participating in a visit due to presence of pharmacy learners rotating through this practice setting.
Conclusion
Our initial findings demonstrate that there is an opportunity for pharmacists in the outpatient Pediatric Complex Lupus Clinic setting to be involved in improving patients’ understanding of non-pharmacologic and pharmacological therapies, improving patient adherence, optimizing weight-based doses, and providing support to patients as they take on additional medication management tasks.
References
- Rahman A, Isenberg DA. Systemic Lupus Erythematosus. N Engl J Med. 2008;358:929-39.
- Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365:2110-21.
- Weiss JE. Pediatric systemic lupus erythematosus: more than a positive antinuclear antibody. Pediatrics in Review. 2012;33(2):62-74.
- Young DC, et al. Patients and Families Experience With Pharmacist Care at Cystic Fibrosis Foundation Accredited Clinics. Pediatr Pulmonol. 2019 Aug;54(8):1216-1224.
- Samuel O, et al. Interdisciplinary Care Team with Pharmacist in a Community-based HIV Clinic. J Natl Med Assoc. 2018 Aug;110(4):378-383.
- Farmer EK, et al. The Pharmacist's Expanding Role in HIV Pre-Exposure Prophylaxis. AIDS Patient Care STDS. 2019 May;33(5):207-213.
- Haas-Gehres A, Sebastian S, Lamberjack K. Impact of pharmacist integration in a pediatric primary care clinic on vaccination errors: a retrospective review. J Am Pharm Assoc (2003). 2014 Jul-Aug;54(4):415-8.
- Al Hussaini M, Hammouda EI, Hammouda AE. Optimizing pharmacotherapy of systemic lupus erythematosus: the pharmacist role. Int J Clin Pharm. 2014 Aug;36(4):684-92.
- Hall JJ, Katz SJ, Cor MK. Patient Satisfaction with Pharmacist-Led Collaborative Follow-Up Care in an Ambulatory Rheumatology Clinic. Musculoskeletal Care. 2017 Sep;15(3):186-195.
- Naqvi AA, et al. Impact of pharmacist educational intervention on disease knowledge, rehabilitation and medication adherence, treatment-induced direct cost, health-related quality of life and satisfaction in patients with rheumatoid arthritis: study protocol for a randomized controlled trial. Trials. 2019 Aug 9;20(1):488.
- Abraham O, et al. Pediatric medication use experiences and patient counseling in community pharmacies: Perspectives of children and parents. J Am Pharm Assoc (2003). 2017 Jan-Feb;57(1):38-46.e2.
- Marmor MF, et al; American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun;123(6):1386-94.
- Jorge AM, et al. Hydroxychloroquine prescription trends and predictors for excess dosing per recent ophthalmology guidelines. Arthritis Research & Therapy. 2018, 20:133.
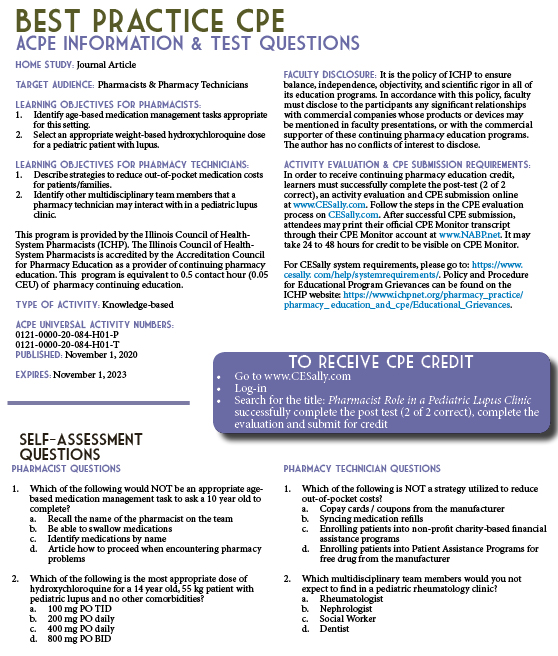
Organizational Affairs
Annual Meeting Fun Facts
by Elise Wozniak, PharmD; Director of Organizational Affairs
We hope that you enjoyed the first virtual ICHP Annual Meeting in 2020! ICHP meetings have changed over time. Below are some interesting facts about ICHP meeting history:
- Annual Meetings began in the 1960s and used to be in the SPRING! The meeting moved to the fall in 1997.
- Fall Gatherin’ was a more informal meeting in the fall during the 1980s.
- The Spring Meeting began in 2001 when the combined Congresses between ICHP and IPhA ended.
Features
Staff Changes
Best Wishes, Jan! Welcome, Kim!
In August of 2020 ICHP accountant Jan Mark retired. Jan worked for ICHP for more than 18 years.
During those years, Jan handled our meeting exhibit showcases and helped to make our Reverse Exhibit program the success it is today. She was the friendly voice you talked to when you needed to pay over the phone and you probably spoke with her a time or two when checking in to a meeting.
We all wish her the best and hope she enjoys the fruits of retirement and more time with her grandchildren.
Before Jan left, she helped train her replacement. ICHP is excited to introduce our new bookkeeper/vendor liaison, Kim Anderson.
(Pictured Left to Right: Jan Mark, Kim Anderson)
A little about Kim...
Kim is a graduate of the University of Wisconsin - Whitewater where she obtained a BBA in accounting.
She's been married to her husband Bob for 24 years. They have 3 sons, stepsons Robert (32) and Matthew (30) and their son Jalen (19).
Her hobbies include spending time with her family and friends. traveling, working out, home décor and decorating and shopping!
Kim has been a great addition to the ICHP staff and she's excited to meet everyone once we can resume in-person events!
Passing The Baton To Our Team
by Carrie Vogler, PharmD, BCPS; Immediate Past Presdient, ICHP
I was told that my time serving you as President of ICHP would go by quickly and I can’t believe the time has come to step into my new role of Immediate Past President and pass the baton to Dr. Jennifer Arnoldi, your new ICHP President. This past year’s theme – “Our Team” -- was a perfect fit for pulling everyone together to accomplish great things during unprecedented times. We started strong by engaging key leaders within ICHP during a leadership retreat. I charged our leaders to find ways to engage members, engage the public, and recruit new members. We developed and launched a mentorship program within the New Practitioners Network led by Natalie Tucker. We started the Public Education & Awareness outReach pubLication Subcommittee (PEARLS) led by Scott Drabant so that we can begin teaching the public about medications and health issues, and explain what health-system pharmacists do. New networks for residency directors and technicians were created. We changed our communication strategies to reach you at home with our first ever virtual Annual Meeting.
I encourage you to continue to promote the great things that pharmacists and technicians do each day for our patients. Thank you for the care you have provided to patients, for investing in the profession of pharmacy, and for supporting ICHP. Thank you to the ICHP Board, ICHP staff, and Scott Meyers for the guidance you provided me this year.
I want to pass the baton to YOU and I want to ask again, will you join Our Team, ICHP? ■
ICHP's Newest Affiliate Leaders
New leadership was voted in this fall for our Affiliate chapters.
Northern Illinois society of Health-System pharmacists (NISHP) -
President - Andrew Merker
President-Elect - Jason Alegro
Immediate Past-President - Milena Murray
Secretary - Radhika Polisetty
Treasurer - Erin Shaughnessy
Technician Representative - Vera Kalin
Sangamiss society of Health-System Pharmacists -
President - Ashley Kallal
President-Elect - Kayla (Dubois) Muench
Immediate Past-President - Megan Stoller
West Central society of Health-System Pharmacists-
President - Elizabeth Harthan
Metro East Society of Health-System Pharmacists -
President - Jared Sheley
Opioid Task Force - CPE Opportunity
How to Assess Health-System Implementation of the CDC Recommendations for Prescribing Opioids
by Mark E. Greg, PharmD, RPh Director, Ambulatory Pharmacy Management, Northwestern Medicine Physician Network Oak Brook, IL
Introduction
In recent years, prescription opioid misuse and especially prescription opioid-related deaths have received significant media attention. Health systems are uniquely qualified to implement programs to improve opioid prescribing. A structured approach is essential for assessing pain management practices including opioid prescribing, with the expectation that these efforts will lead to more effective pain management with lower risks of opioid-related morbidity and mortality. Although this discussion will focus on opioid prescribing taking place in ambulatory settings, primarily physician practices, the overall process is applicable to any inpatient or ambulatory setting. For integrated delivery networks (IDNs), ongoing collaboration between system inpatient and ambulatory opioid initiatives is highly recommended.
The United States Department of Health and Human Services - Centers for Disease Control and Prevention (CDC) issued the “CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016” in March 2016 (
https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm).
1 This was followed by “Quality Improvement and Care Coordination: Implementing the CDC Guidelines for Prescribing Opioids for Chronic Pain” in September 2018 (
https://www.cdc.gov/drugoverdose/pdf/prescribing/CDC-DUIP-QualityImprovementAndCareCoordination-508.pdf).
2 The reader is encouraged to review and become familiar with these documents as an in-depth review of this material is beyond the scope of this article. Similarly, the impact of Healthcare Effectiveness Data and Information Set (HEDIS), Centers for Medicare & Medicaid Services (CMS), and payer opioid-related measures, as well as recent updates to State of Illinois laws and related regulations, are beyond the scope of this discussion.
“Implementing the CDC Guidelines for Prescribing Opioids for Chronic Pain” provides a detailed overview of how to assess and implement an appropriate opioid prescribing program. The document is broken down into an overview, three chapters, references, and six appendices. The publication encourages the use of an interdisciplinary team including pharmacists. The chapter titles are: 1) Evidence-based Opioid Prescribing, 2) Clinical Quality Improvement (QI) and Opioid Measures and Protocols, and 3) Practice-level Strategies for Care Coordination. This discussion will focus on Chapter 2.
Chapter 2, Page 10 of “Implementing the CDC Guidelines for Prescribing Opioids for Chronic Pain” includes Exhibit 1: Clinical QI Opioid Measures, a table containing 16 potential measures in alignment with CDC Prescribing Guideline Recommendation statements. In addition to potential improvement in quality, many payers measure and may financially incentivize health systems to meet or exceed certain opioid prescribing goals. The first five measures address starting an opioid in a new or opioid-naïve patient (termed New Opioid Prescription Measures) and the remaining eleven address long-term opioid therapy. By clicking on each measure listed in Exhibit 1, a link takes the reader to Appendix B in the document containing details on how to operationalize the measure using the electronic health record (EHR) and other data. Table 1 is an adaptation of Exhibit 1 in the Guideline which includes yes/no columns that may be helpful when conducting an opioid measure assessment of your organization.
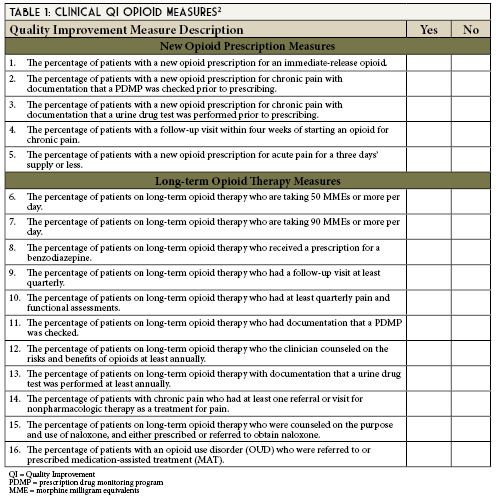
Chapter 2, Page 11 identifies five steps for implementing an opioid QI effort in a healthcare system or practice.
Key Quality Improvement Steps
Step 1: Obtain Leadership Support and Identify a Champion
- Obtain leadership support as a critical first step
It is likely appropriate opioid-related initiatives are currently taking place within your organization. If not, you may be the catalyst for that initiative. Leadership support may be obtained from various departments including administration, pharmacy, nursing, medical director, quality, physician practices, emergency department, immediate care, and others.
Regardless of your role, a first step may be to ask your manager or other key contacts within your organization where appropriate opioid prescribing falls as an organizational priority. Perhaps there is an active committee examining pain management or opioid prescribing. If not, you may be the person to promote this as a Pharmacy & Therapeutics, Quality Improvement, Utilization Management, Patient Safety, Emergency Medicine, Immediate Care Center initiative, or Ambulatory Primary Care Initiative. Leadership reacts to metrics including quality, cost-avoidance, and financial performance.
- Identify a champion(s) to drive the change process
In general, an administrative champion or one or more physician champions are key individuals to engage. Granted, in many cases, pharmacists may be the drivers of quality improvement initiatives and are highly respected by physicians, yet physicians may be more likely to listen to and accept direction from fellow physicians. Securing physician champion support may be aided by informing them that they work will be shared among the team. That is the role of the multidisciplinary change or quality improvement team as discussed below.
- Form a change team (if appropriate) or at least engage key staff
Representatives may include providers (e.g., physicians, advanced practice nurses, physician assistants, pharmacists), nursing, quality, administration, electronic health record support, and IT/analytics. Your providers will be able to share what their needs are based upon the challenges they encounter in daily practice. Meetings involving the physician champion(s) may require early morning or late afternoon times to accommodate clinic hours/patient care activities. Ongoing collaboration between system inpatient and ambulatory opioid initiatives is highly recommended.
- Obtain needed resources and determine readiness
Key resources will include meeting time, a meeting location/virtual meeting, IT/analytics support, EHR support, and data. Key questions to ask your champions and key participants include, “Does the organization identify a problem with current pain management/opioid prescribing?” and “Is the organization willing to make changes in pain management practices?” Changing culture takes time.
Step 2: Assess Current Approaches to Opioids and Identify Areas for Improvement
- Assess current policies and practices
Does the organization have any? If not, create your own. What do you need? How detailed do you want them to be? What do your providers need to make them successful? What have your peers in other health systems developed? The internet includes postings by many health systems that may serve as policy templates.
- Complete the self-assessment questionnaire
An organizational self-assessment is included in Appendix C (pages 52-56) of the guidelines.
- Collect data on your patient population and opioid therapy
Decide what data you wish to collect. What opioids are being prescribed? What is the morphine milligram equivalent (MME) count? Are opioids in combination with benzodiazepines being prescribed? Is naloxone being prescribed for at-risk patients? Your EHR may be able to capture prescription claims data. Some organizations may also receive prescription claims data or reports from payer partners. Review of data may require manual calculation of morphine milliequivalents per day as well as screening for other concomitant CNS-depressant medications.
- Determine access to specialists and other resources
What resources are available? Mental health, pain specialist, substance use programs, and providers of Medication Assisted Therapy (MAT) are just a few important resources. If providers are uncertain how to connect patients requiring substance abuse treatments with available resources, a major “win” may be for the organization to prepare and provide printed lists of substance use providers or EHR links for referrals to MAT providers.
- Identify areas for improvement
What are your greatest needs? Reporting data will accomplish the following: 1) provide baseline measure performance; 2) identify outliers (under- and over-prescribers); and 3) identify those prescribers and patients who may benefit from opioid prescribing assistance. Use the data to help guide your team.
Step 3: Select and Prioritize Guideline Recommendations
Pick a few key areas where you may have the greatest short-term impact, “wins.” Perhaps it will be reducing the number of patients receiving more than 90 MMEs per day or it will be increasing the number of at-risk patients receiving ≥ 50 MMEs/day who are also prescribed naloxone. Perhaps it will be increasing the number of patients receiving chronic (≥ 90 continuous days) opioid therapy that have a signed opioid treatment agreement (OTA) in place. Keep in mind that these guidelines are suggestions and any initiatives should be based upon the unique needs of your health system.
- Determine which guideline recommendations to implement
Appendix B (pages 33-50) of the guidelines entitled, Operational Clinical Quality Improvement (QI) Opioid Measures provides short and long-term opioid measure operational definitions. Operational definitions include the criteria used to build reports. These will assist your data and analytics architects when creating your reports.
- Prioritize what will be implemented
What will you be able to accomplish within your organization? What is the most pressing need? Be realistic given the resources available within your organization and expected time frame to see results.
Step 4: Define System Goals
- Set measurable goals
These goals will vary based upon your baseline data and what may be realistically accomplished within your organization. Administrative and physician leadership prefer metrics.
Step 5: Develop a Plan, Implement, and Monitor Progress
- Develop a plan for implementing selected guideline recommendations
- Implement the changes
- Monitor progress using QI measures and other data
- Review metrics for assessment of opioid prescribing practices
Methods for Obtaining Data That Can Be Used When Analyzing Opioid Prescribing
Appendix B of the guidelines includes 16 operational definition templates. The criteria included in the operational definitions are listed in Table 2.
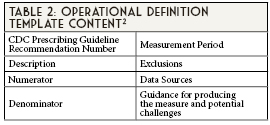
In most cases, the EHR will be the best source for this data. Many individuals and departments within health systems struggle with obtaining reports given the number of requests submitted to the EHR and IT/analytics teams. Obtaining the support from the health system population health team, quality team, executive administration, and chief medical officer for any opioid-related reports will be critical to raising the priority of your request and successfully obtaining your reports. The health system’s data architects will work with you to build your reports according to the operational definitions developed. Validating the data once the report is built will be required to be certain the data elements reported match the actual EHR results. This process may be labor-intensive depending upon the sample size and number of EHR records that need to be reviewed. It is critical to be certain that the report is accurately capturing the intended data required. Trust, but verify. The data needs to be accurate so that when reports are shared with various groups and prescribers, the information appropriately reflects what is taking place in clinical practice.
Case 1
You are a pharmacist in a health-system with an integrated delivery network (IDN). The IDN Medical Director invites you to be a member of the ambulatory pain management quality team. You attend the meetings as the pharmacy representative. One of the measures the team has chosen is the percentage of patients with a new opioid prescription for acute pain for a three-day supply or less. You suggest using the EHR prescribing data. The team agrees.
Case 1 Discussion
You work with the quality team to define the operational definition content for the measure and use the health system’s EHR as the source of your opioid prescribing data. You support the data architects and data analyst team building the reports according to the operational definitions developed. After the reports are created, you assist with validating the accuracy of the report data by reviewing patient profiles in the EHR.
How to prepare a quality improvement algorithm to assist with assessing opioid prescribing quality improvement
The following discussion is based on Step 5 of the above process as described on page 19.2 After defining your goals and determining the area of focus, the next step will be to develop your plan. A standardized process is needed to guide the project and to measure progress (or lack thereof). This should include some type of Plan-Do-Study-Act (PDSA) cycle quality improvement tool (See Figure 1).3 One example is the DMAIC (Define, Measure, Analyze, Improve, Control) methodology.4 DMAIC methodology is a core tool used to drive Six Sigma projects. Included below is a sample DMAIC process used for examining the impact of an ongoing prescriber awareness campaign on hydrocodone/acetaminophen (H/A) prescribing over time. Actual H/A prescription claims (fill) data from a specific payer population was chosen because the data was consistent, accurate, and available quarterly. The DMAIC process may be used and results shared within your quality team, prescribers, and other committees and key individuals to inform them of your progress.
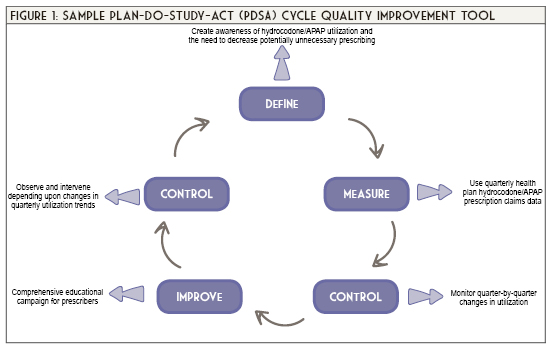
Case 2
Your team’s reports are accurate and the data reveals H/A is the most frequently prescribed opioid in the ambulatory setting. The medical specialties in order of greatest H/A prescribing volume are: primary care, emergency medicine, immediate care, and orthopedics. The average days’ supply prescribed is 5. Data breakdown reveals: 10% ≤ 3 days’ supply prescribed, 70% ≤ 5 days’ supply prescribed, and 20% ≤ 7 days’ supply prescribed.
Case 2 Discussion
The quality team establishes the first year project goal to be 50% ≤ 3 days’ supply prescribed, 45% ≤ 5 days’ supply prescribed, and 5% ≤ 7 days’ supply prescribed. Your team’s plan includes an educational campaign to encourage prescribing a ≤ 3 days’ supply of H/A (assuming an opioid is required). You will also be working with the EHR team to change the default days’ supply for H/A from 5 days to 3 days in the prescribing software. Prescribers will still have the option of selecting a 5 days’ supply. The team decides to meet quarterly to review the data and discuss project feedback. You begin to meet with your prescribers to inform them of the project, share their baseline H/A prescribing, how they compare to their peers in the same medical specialty, and the first-year program goal. Your first quarter results are as follows: 25% ≤ 3 days’ supply prescribed, 55% ≤ 5 days’ supply prescribed, and 20% ≤ 7 days’ supply prescribed. Congratulations! You’re making progress toward your first-year goal. Now continue the PDSA process until you meet or exceed your goal.
Conclusions
Implementing an appropriate opioid prescribing initiative within your health system offers a tremendous opportunity for pharmacists to apply their expertise to improve the quality and safety of patient care. “Implementing the CDC Guidelines for Prescribing Opioids for Chronic Pain” provides a detailed overview to assist organizations with implementing an appropriate opioid prescribing program. Use of a structured approach with the Plan-Do-Study-Act (PDSA) cycle quality improvement process is highly recommended.
References
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep. 2016;65(No. RR-1):1-49. doi: http://dx.doi.org/10.15585/mmwr.rr6501e1
- Centers for Disease Control and Prevention. Quality Improvement and Care Coordination: Implementing the CDC Guideline for Prescribing Opioids for Chronic Pain. 2018. National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention, Atlanta, GA. Available at: https://www.cdc.gov/drugoverdose/pdf/prescribing/CDC-DUIP-QualityImprovementAndCareCoordination-508.pdf. Accessed June 6, 2020.
- Plan-Do-Study-Act (PDSA) Worksheet. Institute for Healthcare Improvement. Cambridge, MA. http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx. Accessed June 6, 2020.
- The Define, Measure, Analyze, Improve, Control (DMAIC) Process. American Society for Quality. https://asq.org/quality-resources/dmaic Accessed June 6, 2020.
Annual Meeting Recap
2020 Annual Meeting
by Melissa Dyrdahl, BA; Communications Manager, ICHP
That’s a wrap! The 2020 ICHP Annual meeting is officially done (well technically you have until November 15, 2020 to submit your CPE credits – don’t delay!).
This year’s meeting, much like this year in general, was unlike anything we’ve ever experienced. The Covid-19 pandemic had ICHP staff on a mission to figure out how we could safely bring you the high-quality pharmacy education that you’ve come to expect from our meetings. We researched various platforms and eventually decided to work with MCSV. (Sound familiar? MCS is the company we work with at our Annual Meeting each year at Drury Lane for our AV and booth needs).
Overall we welcomed 350 attendees for our live programming in addition to a Reverse Exhibit for our pharmacy vendors and a Residency Showcase for students. More have registered for on-demand only continuing education. We had specialized technician programming, the latest in clinical research and even heard from ASHP’s Chief Executive Officer, Paul Abramowitz.
Working hand-in-hand with MCSV we were able to offer up to 26.25 hours of programming (23.5 credit hours for pharmacists and 16.25 credit hours for pharmacy technicians) on the virtual platform, Pheedloop. Our meeting consisted of on-demand, live and semi-live presentations. After the meeting all programming was transferred to on-demand for the remainder of the month – so if attendees missed a live session they could still check it out.
Opening the meeting, ICHP’s president, Carrie Vogler announced our NEW officers, who include:
President – Jennifer Arnoldi
Immediate Past President – Carrie Vogler
Secretary – Bryan McCarthy
Director of Marketing Affairs – Denise Kolanczyk
Director of Educational Affairs – David Martin
Technician Representative – Rebecca Ohrmund
Chair of the New Practitioners Network – Marianne Pop
Chair of the Ambulatory Care Network – Bridget Dolan
Chair of the Pharmacy Informatics and Technology Network – Heather Harper
Chair of the Residency Leaders Network – Nora Flint
These officers will join our current roster of ICHP board member. We also want to thank our outgoing board members, Noelle Chapman, Ed Rainville, Bernice Man, Kristine VanKuiken, Natalie Tucker and Daniel Majerczyk for all their hard work over the last couple of years.
Carrie also took the opportunity to announce this year’s ICHP award winners. They are as follows:
The President’s Award – Bernice Man
Outstanding Volunteer – Milena Murray
New Practitioner Leadership Award – Natalie Tucker
Pharmacist of the Year – Starlin Haydon-Greatting
Amy Lodolce Mentorship Award – Jennifer Phillips
Pharmacy Technician of the Year – Richard Puccetti
Past President’s Award – Carrie Vogler
Shining Stars:
- Jason Alegro
- Scott Drabant
- Brooke Griffin
- Elizabeth Harthan
- Denise Kolanczyk
- Daniel Majerczyk
- Andrew Merker
- Justin Moore
- Rebecca Ohrmund
- Ehsan Tavassoli
- Karin Terry
- Tran Tran
Best Practice Award – Shannon Rotolo of UChicago Medicine for research on “Pharmacist Role in a Pediatric Lupus Clinic”
Student Chapter Award – University of Illinois Chicago College of Pharmacy (Chicago & Rockford).
Following the meeting we announced our 2020 Platform Presentation winners:
Megan Malone - Pharmacist Driven Immediate Discharge on Direct Oral Anticoagulant for Venous Thromboembolism from the Emergency Department
Aisha Shajee - In Vitro Activity of Imipenem-relebactam Alone and in Combination with Fosfomycin Against Imipenem-nonsusceptible Pseudomonas aeruginosa
All in all, while this year’s meeting felt quite different (admit it – who watched Saturday’s session in their sweatpants? ☺), we feel proud that we were able to bring you great programming from some truly remarkable presenters.
The 2021 ICHP/MSHP Spring Meeting is also going virtual. Planning is in the works. We hope you’ll join us for another virtual venture - March 19 & 20, 2021. Please stay safe and take care and hopefully by next fall we’ll be meeting face-to-face again.
College Connection
Midwestern University Chicago College of Pharmacy
How Getting Involved in Student Organizations Helped Me Gain the "Pharmacy School Experience"
by Nisreen Elagha, PharmD candidate 2022, SSHP Treasurer; Midwestern Universty Chicago College of Pharmacy
More than half way through my pharmacy school experience, I am able to look back on the experiences that make up my fondest memories. Midwestern University hosts an annual organization fair that showcases the various students run projects and clubs. As an eager first year student, I attended in hopes of finding my niche in pharmacy school. I found a few organizations that caught my interest and signed up. By the end of my first year of pharmacy school, I gained several leadership and committee member positions.
Through joining these organizations, I gained clinical, therapeutic, and interpersonal skills outside of the classroom and in a real-world setting. I learned how to manually take blood pressure readings and how to do blood glucose screenings a year before I was introduced to the concept in class. I was able to apply these skills that I had learned to community service clinics. At these clinics, I was able to screen patients, assess their results, and discuss how to improve their current disease states. This gave me the confidence to communicate with patients effectively and improve their overall health. I was also able to gain therapeutic knowledge and counseling skills on the various hypertension and diabetic medications before my therapeutics course. My clinical and therapeutic skills also helped me thrive during IPPE rotations as I was able to recognize medications, health conditions, and important counseling points. I was also given the opportunity to join an organization that focuses on substance use disorders which introduced the severity of the current opioid crisis. This organization also trained the community on how to respond to an overdose event, and how to administer naloxone, a potentially life-saving drug. Just as other organizations taught me clinical skills and therapeutic knowledge in advance, this organization educated me about opioids before therapeutics. Gaining the confidence to apply the skills that I had learned eventually helped me to thrive in my therapeutics and clinical skills classes.
By getting involved in organizations on campus, I was able to develop skills that put me ahead of my colleagues. I felt as though it was an advance because it gave me more exposure, practice, and networking opportunities. Being an active member of ICHP has been a rewarding experience. I joined the ICHP mentorship program where I was paired with a first-year student to offer social and educational guidance in graduate school. Our SSHP chapter also offered a burnout panel where alumni were able to share their experiences on how to avoid burnout as a graduate student and during residency. This was a great panel to attend as it gave me insight on ways to mentally and physically survive challenging times in my pharmacy career.
Beyond the educational purpose of joining organizations on campus, I made lifelong friends. Finding a group of people that share my same interests allowed me to stay passionate about my career, and also to discover more about various pharmacy settings and careers. Social events that were held within ICHP for its members allowed us to come together and release stress after a long week of exams and classes. I found that sharing the good, bad, and the ugly, while also motivating each other to achieve success, was in itself rejuvenating.
Overall, through my organizational involvement on campus, I have made unforgettable memories and I have also developed many skills as a pharmacy student. I encourage all students to get involved on campus to experience unique pharmacy practices and to create an unforgettable graduate school experience.
Rosalind Franklin University College of Pharmacy
Making Mental Health a Priority
by David Courteau, PS-3, ICHP Member, Rosalind Franklin University College of Pharmacy
According to the World Health Organization (WHO), “every 40 seconds, someone loses their life to suicide.”1 In light of this disturbing statistic, the International Association for Suicide Prevention collaborated with the WHO in 2003 to develop a World Suicide Prevention Day. This awareness day is observed annually on September 10th. Locally, Rosalind Franklin University (RFU) participates in National Suicide Prevention Week, which encompasses the week surrounding World Suicide Prevention Day. This year, with the efforts of our college’s Student National Pharmaceutical Association (SNPhA) chapter, students are encouraged to share positive notes and favorite quotes on social media platforms using the hashtag “#keepgoing”.
Mental health is equally as important for our patients as it is for their healthcare providers. To increase awareness, the SSHP chapter at RFU has developed a Mental Wellness Chair position that will strive to ensure our student body is confident in recognizing mental health warning signs. The Mental Wellness Chair will be responsible for connecting with guest speakers to discuss holistic treatment approaches in achieving mental well-being. Additionally, our chapter’s Mental Wellness Chair hopes to shed light on the pharmacists role in psychiatry by educating students from a resident and practicing pharmacist’s point-of-view. We are excited to see how this position will affect local advancements in mental health stigma-reduction efforts, as well as regional partnerships with other local colleges of pharmacy!
Despite the COVID-19 pandemic remaining in full-force, the Student Counseling Services at RFU have remodeled their delivery of care to ensure mental health services go uninterrupted. With the utilization of HIPAA-compliant platforms, telepsychology sessions allow licensed clinicians on our campus to ensure no student is lost to follow-up. Furthermore, clinicians have expanded their appointment hours to accommodate for the dynamic schedules with remote learning. To complement mental health, the Office of Fitness and Recreation at RFU highlights the importance of “wellness” throughout these unprecedented times. With the goal of improving psychological balance, weekly “Mindfulness Meditation” sessions are held virtually via Zoom for any student who is seeking to achieve stress-reduction or improve focus techniques. Additionally, these sessions are recorded for campus-wide community access.
While the end of this pandemic remains obscure, the RFU student body remains resilient and adaptable. It is with great hope that our profession can be a key player in the preventative vaccination efforts against COVID-19. In the meantime, however, it is crucial that current and future healthcare professionals ensure their mental health is effectively addressed. We can all play a part, whether it be advocating for national suicide prevention or developing a Mental Wellness Chair in your local SSHP chapter! ■
Reference
- World Suicide Prevention Day. World Health Organization. https://www.who.int/news-room/events/detail/2019/09/10/default-calendar/world-suicide-prevention-day-(wspd). Published 2019. Accessed September 5, 2020.
Southern Illinois University Edwardsville School of Pharmacy
Pharmacy School in a Virtual World
by Sara Gardner, P2, President-Elect, SIUE School of Pharmacy
The unprecedented pandemic of SARS-CoV-2 has altered the lives of people worldwide in more ways than can be counted. Everyone can provide a different perspective through their unique experiences during this pandemic, and an interesting perspective to consider is that of pharmacy students and faculty members. I spoke with a student from each class at the SIUE School of Pharmacy, as well as several faculty members, about their experiences with navigating the academic world of pharmacy in the time of COVID-19.
The P1 students at the SIUE School of Pharmacy have had very different experiences with applying to pharmacy school than previous students who had traditional application experiences. I asked Angela Whalen, a P1 student, if a virtual interview day made her more or less nervous than a traditional interview day would have. Angela said that she would have been nervous either way, but her interview day was her very first experience using Zoom, which added a little bit more pressure. Despite feeling nervous, Angela handled her interview day well. She said, “My interview went very smoothly! The faculty and staff were wonderful, and they all made me feel confident and at ease. I could not have asked for a better experience.”
The P2 and P3 students at SIUE have a bit of experience with virtual learning under their belts, as they spent most of the 2020 spring semester learning remotely. The P2s are enrolled in a Physical Assessment course this semester and were able to visit campus in small groups to practice blood pressure and heart rate screening for this course. Deborah Lindquist, a fellow P2 student, said that in order to successfully transition to online learning, she has tried to create a routine at home, including waking up at the same time every day, and assigning certain times of her day to studying. “A perk of online learning is that I don’t have to wake up as early and pick out a coordinated outfit! A downside is that I’m not getting as much movement in my day as I used to when we went to class in person.” Deborah said meal planning and taking short walks between classes have helped her feel less stressed. She also recommends setting up Zoom social calls with friends to help feel connected. Renae Oelrich, a P3 student, said she feels she has more independence with her schedule, but she also realizes that it takes more discipline to watch lectures when there are distractions at home. Renae said, “I also really like being at home with my dog, and he loves it, too!” She is taking an elective course that meets on campus every other week and has also taken exams on campus.
While the time that P4 students spend on campus is already limited, APPE rotations have also been impacted by COVID-19. Kristen Ingold, a P4 student, completed a virtual infectious disease rotation, in which students worked-up patients on their own time, and met online to discuss recommendations and plans. She also listened to journal clubs and case presentations hosted by hospital staff during lunch hours. Kristen is currently on a general hospital rotation, and she is working on-site, experiencing opportunities mostly as normal. When asked if she has any advice for her peers on being successful with virtual learning, Kristen said, “Attend the live lectures and participate when you can. Virtual learning can be uncomfortable and is new for the instructors as well. Ask questions, show your face on camera, and obtain the most out of the learning that you are paying to receive.”
Pharmacy school students are not the only ones whose academic experience has been affected by the COVID-19 pandemic; faculty members have clearly felt an impact as well. Dr. Lisa Lubsch, a clinical professor at SIUE SOP, said “Our faculty have worked so well together by sharing knowledge and experiences to advance our use of Zoom, and enhance our teaching online. I do miss in-person lab, but we have adjusted.” A positive of virtual education for Dr. Lubsch is the time saved on her commute, allowing her more time to complete other work. Dr. Jingyang Fan, the Assistant Dean of Academic Affairs and a clinical professor at SIUE SOP, says that since most of her work is behind the scenes to support the faculty, she is familiar with working from home. When asked if she has noticed any positives to virtual education, she said, “With online synchronous classes, students can join us from anywhere with decent internet. In a way, it has made their lives more flexible. In addition, faculty are able to use different instructional technology that they normally wouldn’t with on-ground classes.” Dr. Fan recommends that faculty learn to use technology to enhance teaching, and to be understanding without compromising the quality of education that SIUE provides.
Despite the challenges that students and educators are facing during the COVID-19 pandemic, it has been inspiring to see how crucial the field of pharmacy is, particularly during our current state of affairs. Pharmacy students and faculty are a motivated bunch, and virtual learning gives us yet another opportunity to become resilient and trusted health care providers.
University of Illinois Chicago College of Pharmacy
The Case of Virtual Pharmacy Student Organizations
by Rachel Goldberg, P3, ICHP Fundraising Chair; University of Illinois Chicago College of Pharmacy
As an undergraduate student at a very large university, I regretfully did not get involved in student organizations. I felt swallowed up by the massive student body population and extremely unsure of my career interests. However, as I transitioned from my undergraduate life to a first-year professional pharmacy student at the University of Illinois at Chicago College of Pharmacy in September 2018, I intended to get involved to advance my career and network with other pharmacy professionals. UIC pharmacy student organizations have organized flu shot health clinics, hosted networking events, invited pharmacists to speak at general body meetings, and have ultimately fostered a strong network for students to collaborate with one another and others within the profession. Furthermore, organizations have helped many students, such as myself, develop a strong passion for pharmacy, make important connections, and establish ourselves as a future healthcare provider. However, as the pandemic has shifted our definition of normal, it has especially impacted student life on campuses across the nation, including pharmacy schools. While transitioning to a virtual semester, the case for pharmacy student organizations has an especially important implication for this academic year.
A 2019 study examined skill development at a number of university student pharmacy organizations using student surveys and interviews. The authors concluded that organizational involvement provided opportunities for students to develop core competency skills in the discipline of pharmacy. Among others, core skills developed were communication and collaboration.1 Emerging young professionals, such as pharmacy students, running an organization for the student body can build a strong professional network and foster essential skills. Student pharmacy organizations, such as the ICHP student chapter, will need to be run virtually with a strong platform that allows for interaction.
I am a third-year pharmacy student and this will be my third year as an active member of the Illinois Council of Health-Systems Pharmacists (ICHP) UIC Chapter. This year, I am faced with the challenge of navigating my involvement virtually and maintaining excitement for an organization that has helped my growth as a professional from behind a computer screen. However, this challenge must be accomplished if we want to provide students with opportunities to develop skills that cannot be taught in a lecture hall. The experience of hosting and listening to speakers in our field is important for us as we decide our own futures. Furthermore, networking events can be conducted virtually and will encourage students to follow-up with pharmacists through e-mail and LinkedIn. Online platforms allow students to create important business relationships and navigate a social media-driven age. Fundraising efforts may shift from fundraising for our chapter’s budget to online fundraisers for charities of our choice. The 2020 ICHP Annual Meeting was also conducted virtually; it was more important than previous years for students to attend because professional networking events will be limited this year.
Our student executive board members will undoubtedly face challenges as we move forward. Nonetheless, we will persevere in the best interest of our student body and especially for our new students. A pharmacist may know every single adverse reaction, PK/PD parameter, or dosing of a given drug, but the pharmacist must also have the communication and teamwork skills to be a successful practitioner. It is our student chapter’s goal to provide students with opportunities to develop core competencies.1 While opportunities this year may be offered via a Google Hangout or Zoom, it is a high priority this year for pharmacy student organizations to unite our student pharmacy body and establish our skills as future healthcare providers. ■
Reference
- Zeeman JM, Bush AA, Cox WC, Buhlinger K, McLaughlin JE. Identifying and mapping skill development opportunities through pharmacy student organization involvement. Am J Pharm Educ. 2019;83(4):6950. doi:10.5688/ajpe6950
More
Upcoming Events
Diversity in Pharmacy Webinar Series
November 5, 2020
Topic: Equity
Register online:
www.ichpnet.org/events/calendar/
Sangamiss Live Webinar
November 10, 2020
Topic: Hereditary Angioedema: What It Is & How to Treat It
Speaker: Erica Ridley, PharmD
ICHP Leadership Retreat (Virtual)
November 13, 2020
By Invitation Only
NISHP Live Webinar (Open to all Pharmacist members)
November 18, 2020
Topic: New Directions in Influenza Management: The Pharmacist's Guide to Patient Identification, Testing and Antiviral Use
Speaker: Katherine Lusardi, PharmD
ICHP CE Appetizer
November 24, 2020
Topic: Interoperability for Combating the Opioid Crisis: ILPMP
Speaker: Adam Bursua, PharmD, BCPS
Accredited for Pharmacists
ICHP CE Appetizer
January 20, 2021
Topic: COVID Updates
Speakers: Jason Alegro, PharmD, BCPS, BCIDP
& W. Justin Moore, PharmD
Accredited for Pharmacists
ICHP/MSHP Spring Meeting (Virtual)
March 19 & 20, 2021
Welcome New Members!
ICHP would like to welcome its newest members!
Pharmacy Action Fund Contributors
Thank you to everyone who donated to the PAC!
Board of Directors
Board of Directors
|
Jen Arnoldi
President
|
Julie Downen
Regional Director
Central
|
David Martin
Educational Affairs
Director
|
Bridget Dolan
Ambulatory Care
Network Chair
|
|
Carrie Vogler
Immediate Past
President
|
Alifiya Hyderi
Regional Director
Northern
|
Denise Kolanczyk
Marketing Affairs
Director
|
Tara Vickery Gorden
Small and Rural Hospital
Network Chair
|
|
Kathryn Schultz
President-Elect
|
Jared Sheley
Regional Director
Southern
|
Sharon Karina
Government Affairs
Director
|
Heather Harper
Pharmacy Informatics
and Technology
Network Chair
|
|
Michael Weaver
Treasurer
|
Becky Ohrmund
Technician
Representative/
Pharmacy Technician
Network Chair
|
Amy Boblitt
Professional Affairs
Director
|
Jennier Phillips
Editor & Chair,
KeePosted
|
|
Bryan McCarthy
Secretary
|
Elise Wozniak
Organizational Affairs
Director
|
Marianne Pop
New Practitioners
Network Chair
|
Milena Murray
Assistant Editor,
KeePosted
|
|
Scott Meyers
Executive Vice
President
ICHP Office
|
Chris Crank
Executive Vice
President Designee
ICHP Office
|

Nora Flint
Residency Leaders
Network Chair
|
|
Student Society Presidents
Justine McCoy
Chicago State University College of Pharmacy
|
Justin Shiau
Southern Illinois University Edwardsville School of Pharmacy
|
Ruba Samara
Midwestern University Chicago
College of Pharmacy
|
Michael Forst
University of Illinois at Chicago
College of Pharmacy
|
Ali Naserallah
Roosevelt University College of Pharmacy
|
Max Stone
University of Illinois at Chicago
Rockford Campus College of Pharmacy
|
Nadine Alwawi
Rosalind Franklin University
College of Pharmacy
|
|
Northern Illinois Society of Health-System Pharmacists (NISHP)
Andrew Merker
President
|
Jason Alegro
President-Elect
|
Milena Murray
Immediate Past President
|
Erin Shaughnessy
Treasurer
|
Radhika Polisetty
Secretary
|
Vera Kalin
Technician Representative
|
West Central Society of Health System Pharmacists
Metro East Society of Health-System Pharmacists (MESHP)
Sangamiss Society of Health-System Pharmacists
Ashlie Kallal
President
|
Kayla (DuBois) Muench
President-Elect
|
Megan Stoller
Immediate Past-President
|
Vacant Roles at Affiliates
President, Rock Valley Society
President, Southern IL Society
President, Sugar Creek Society
Print Entire Issue


 Directly Speaking
Directly Speaking
 President's Message
President's Message Congratulations to Rebecca Ohrmund, CPhT.
Congratulations to Rebecca Ohrmund, CPhT. 
 100x100.jpg)