Print This Article
Educational Affairs
BEERS Criteria 2019 Update: A Summary of Notable Changes
by Candace Bishop, PharmD, MPH PGY2 Pharmacy Administration Resident; Advocate Aurora Health, Lutheran General Hospital; Jen Phillips, PharmD, BCPS, FCCP, FASHP; Associate Professor; Midwestern University Chicago College of Pharmacy
Older Adults and Medication Use Safety
As the proportion of the United States population over the age of 65 years continues to grow, it is imperative that healthcare providers recognize and understand the intricacies of caring for older adults.1 As part of the normal aging process, a number of changes occur in the human body. Among these changes are pharmacokinetic (PK) and pharmacodynamics (PD) effects of medications. One of the most clinically relevant changes is a decline in renal elimination pathways and liver metabolism of certain medications.2 These changes often necessitate dose reductions based on the function of these vital organs. Regarding pharmacodynamics, older adults are generally more prone to exaggerated responses to medications, more commonly side effects than therapeutic effects.2 This is especially true for medications affecting the central nervous system. Because of these PK and PD changes, it is vital that healthcare professionals be especially vigilant in monitoring older adults for both therapeutic and adverse effects of medications.
In addition to the PK and PD changes that naturally occur over the life course, additional factors have been identified as negatively affecting the medication use safety of elderly patients. One of these medication safety issues is polypharmacy, which is defined as taking 5 or more medications at one time.3 Polypharmacy affects approximately 30% of older adults in developed countries.3 In the United States, older adults purchase 33% of all prescription drugs despite making up only 14.5% of the US population. This proportion of prescription purchasing is expected to increase to 50% by the year 2040.3 Polypharmacy has been associated with worsening of geriatric syndromes and adverse drug events. Additionally, complex medication regimens heighten the potential for drug-drug interactions, which can cause additional adverse reactions with a wide range of severity.
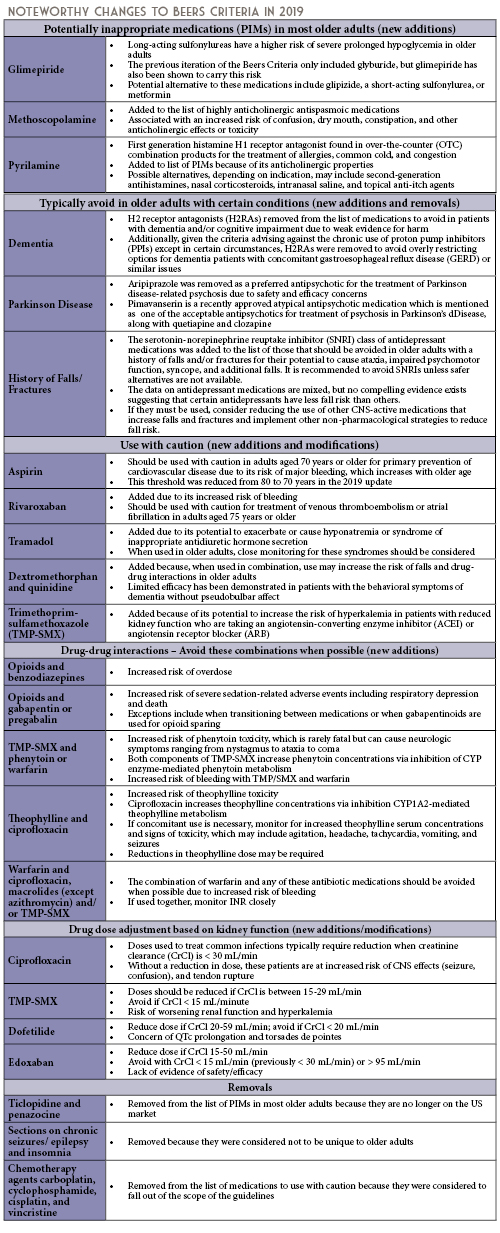
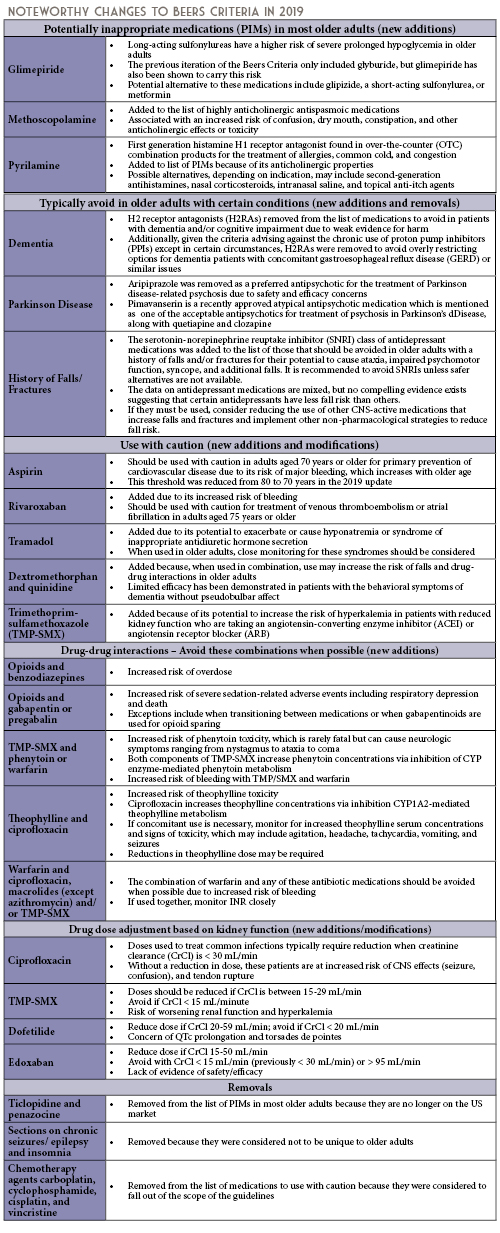
Given the aforementioned challenges in caring for older adults, there are some medications that should generally be avoided in all older adults, and some that should be avoided or modified in certain older adult populations. These are outlined in the Beers Criteria, which is an explicit list of potentially inappropriate medications that are typically best avoided in adults aged 65 years or older.4 Updates to these criteria are produced by the American Geriatrics Society (AGS) on a 3-year cycle, with the most recent update published in April 2019. The 2019 update represents the 5th update since the original list was published in 1991. The intent of the Beers Criteria is to improve medication selection by clinicians in patients aged 65 years or older, reduce adverse drug events in these patients, and to serve as a tool for evaluating the quality of care, cost, and patterns of drug use in older adults.4 The criteria are categorized into 5 types, and noteworthy changes for each criterion since the last published edition are outlined in the following sections.
Pharmacist Roles in Ensuring the Medication Safety of Older Adults
The AGS Beers Criteria are intended to be applied to the care of older adults in all ambulatory, acute, and institutionalized settings except for hospice and palliative care settings.4 Using the Beers Criteria in combination with clinical judgment is essential. There may be situations when medications on this list may need to be administered due to clinical situations. In these instances, the risk to benefit ratio should always be considered.
Pharmacists are uniquely poised as the most accessible healthcare providers, with the ability to influence the care of older adult patients in all of these settings. Potential strategies for pharmacist intervention include: suggesting alternative medications, reducing doses, and/or recommending shorter courses of therapy, when appropriate. For OTC medications, pharmacists should consider whether it is appropriate to continue scheduled or as needed dosing at home during care transitions, given that there may be less monitoring at home, less supervision and oversight, and less control of the environment. Pharmacists in community or ambulatory care settings can assist older adults in choosing appropriate OTC medications, avoiding combination products with certain ingredients, and providing counseling to monitor for adverse effects.
Armed with their clinical knowledge, expertise, and guidance from the AGS, pharmacists can assist in improving medication selection, educating clinicians and patients, and reducing adverse drug events due to potentially inappropriate medications in older adults.
References
- Sade RM. The graying of America: challenges and controversies. J Law Med Ethics. 2012;40(1):6-9.
- Delafuente JC. Pharmacokinetic and pharmacodynamic alterations in the geriatric patient. Consult Pharm. 2008;23(4):324-334.
- Kim J, Parish AL. Polypharmacy and medication management in older adults. Nurs Clin North Am. 2017;52(3):457-468.
- 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.