Print This Article
Educational Affairs
A review of Medical Marijuana and the Pharmacist's Role
by Chloe Majkowski, PharmD Clinical Pharmacist, Oncology Northwestern Medicine Huntley Hospital; Amanda N. Seddon, PharmD, BCPS, BCOP Assistant Professor of Pharmacy Practice Midwestern University, Chicago College of Pharmacy; Justin D. Fisher, PharmD Clinical Pharmacy Specialist, Hematology/Oncology/Cellular Therapy Rush University Medical Center
With increasing legalization at the state level for both medical and recreational marijuana, pharmacists are in a position to educate patients and other healthcare professionals on the risks and potential benefits of cannabis. While there continues to be much controversy on the clinical use of marijuana, pharmacists are an important resource in understanding disease states in which it may provide potential benefit, as well as risks, including drug-drug interactions and adverse effects.
The earliest written records of human cannabis use date back to the 6th century BC, but our understanding of its physiologic effects has only more recently become apparent.1 More than 104 chemical compounds that act on cannabinoid receptors have been identified in Cannabis. It is important to note the differences between cannabis and associated products. Cannabis is a botanical product, and most commonly utilized in the form of marijuana, or dried leaves of the cannabis plant. Cannabinoids are chemical compounds found in cannabis that act on cannabinoid receptors. Tetrahydrocannabinol (THC) and cannabidiol (CBD) are the most abundant cannabinoids and biologically active compounds found in cannabis. THC is a psychoactive compound associated with the commonly experienced “high,” and CBD is a non-psychoactive compound that tends to produce a relaxing effect. The most well-known species within the Cannabis genus are Cannabis sativa, which generally has higher concentrations of THC, and Cannabis indica, which usually contains more CBD.
Pharmacology and Physiologic Effects of Cannabis
Pharmacology
The human endocannabinoid system consists of two types of receptors, CB1 and CB2.1 CB1 receptors are primarily concentrated in the brain and central nervous system, while CB2 receptors are mostly found in peripheral organs, especially those associated with the immune system. CBD has a low affinity for both CB1 and CB2, but acts as an allosteric modulator at opioid receptors and is a known serotonin receptor agonist.1,2 THC binds with greater affinity to CB1 and CB2, which results in the typical effects associated with marijuana use.1
Administration
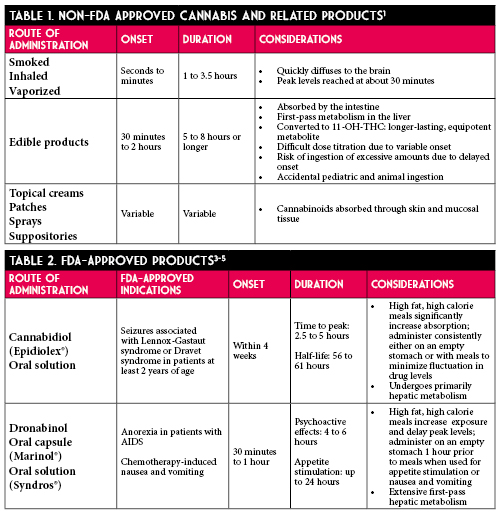
Various routes of administration are available for cannabis and associated products.1 Route of administration should be carefully considered due to implications of varying pharmacokinetic factors, such as the risk of overdose with edible products due to their delayed onset of action. Notable differences in onset, duration, and special considerations are summarized in Tables 1 and 2.
Metabolism and Drug Interactions
Both THC and CBD are metabolized by cytochrome P450 (CYP) 3A4 enzymes.6 Additionally, THC is metabolized by CYP2C9, and CBD by CYP2C19. Because of this, patients with altered CYP450 enzymes who are poor metabolizers may experience increased or prolonged effects of these compounds. Drug interactions with concomitant use of CYP450 inhibitors or inducers may also be relevant. Further, the physiologic effects of these compounds may be increased when used in combination with sympathomimetic drugs, CNS depressants, or anticholinergic agents.
Physiologic Effects
Acute effects of cannabis include enhanced sensitivity to stimuli, altered perception of time, increased appetite, decreased short-term memory, dry mouth, and impaired perception and motor skills.1 Very high blood levels of THC may result in panic attacks, paranoid thoughts, or hallucinations. Rarely, users may experience cannabinoid hyperemesis syndrome, a difficult to treat phenomenon characterized by cyclic vomiting associated with chronic cannabis use.7 The dosage of THC as well as individual variability in absorption and metabolism may influence the intensity and duration of intoxication.1 Additionally, desensitization with sustained use of cannabis may occur as chronic cannabis use leads to down-regulation of CB1 receptors, which may be reversed by abstinence.
Laws and Regulations
Marijuana remains a schedule I substance under the Controlled Substances Act due to its high potential for dependence and lack of a widely accepted medical use, making distribution of cannabis a federal offense.8 Because federal law prohibits prescriptions for marijuana, many states allow medical marijuana “recommendations” or “referrals” rather than prescriptions. In Illinois, the medical cannabis pilot operation was initiated in 2014, and over 80,000 people in Illinois participated in the program. The program was later made permanent, taking effect January 1, 2020.
In order to purchase medical marijuana in Illinois, patients must receive a certification from their provider confirming a qualifying debilitating condition.9 There are currently over 50 qualifying conditions in Illinois including cancer, chronic pain, migraines, irritable bowel syndrome, and seizures. Once certification is obtained, the patient may purchase a registry ID card which is valid for 3 years.8,10 Under this registry, patients may purchase up to 2.5 ounces of medical cannabis during a 14-day period, and may grow up to 5 plants at home. The new law also allows students to use medical cannabis under the supervision of a school administrator or nurse on school property; previously, a student could only receive medical marijuana from a parent or guardian on school grounds. Of note, recreational marijuana was also legalized in Illinois under a law that took effect January 1, 2020. Illinois is the 11th state to legalize recreational marijuana for adult use. Lastly, over-the-counter products containing CBD extracted from cannabis are available in all 50 states.11,12 It is only legal to sell or purchase these products if there is less than 0.3% THC in the product.
Medical Literature
High-quality evidence exists for FDA-approved products cannabidiol (Epidiolex®) and dronabinol (Syndros®, Marinol®). Epidiolex is a purified form of CBD used in the setting of childhood epilepsy,
specifically Lennox-Gastaut Syndrome (LGS) and Dravet Syndrome (DS). Studies found a 41-44% reduction in seizures versus placebo in patients with LGS and DS.13 Additionally, synthetic THC derivatives, nabilone and dronabinol, are widely accepted treatments for refractory chemotherapy-induced nausea and vomiting, though nabilone has since been discontinued.14
The FDA has not approved cannabis for treatment of any disease or condition and sites the need for additional clinical trials to assess safety and effectiveness.9 While no randomized controlled trials exist for the use of cannabis in the medical literature, there are smaller studies that may help guide our treatment decisions. A comprehensive review of available literature was conducted by the National Academies of Sciences, Engineering, and Medicine, and the group published a public health report in 2017 on the health effects of cannabis and cannabinoids.1 Several findings were considered conclusive or with substantial evidence for use. First, the Academy found that cannabis or cannabinoids are effective for the treatment of chronic pain in adults. Second, oral cannabinoids are considered effective antiemetics for the treatment of chemotherapy-induced nausea and vomiting. Lastly, oral cannabinoids are effective for improving patient-reported multiple sclerosis spasticity symptoms. However, the effects of cannabis and cannabinoids are modest for all of these conditions, and there is inadequate information to assess effects for all other indications that were evaluated. More recent prospective studies, although small, have demonstrated benefit of sublingual THC oil for neuropathic pain, and inhaled cannabis vapor for chronic fibromyalgia pain.15,16
Pharmacist’s Role in Patient Management and Cannabis Use
Pharmacists play an important role in educating patients that cannabis is not a replacement for evidence-based pharmacotherapy, and more research is needed to confirm the safety and efficacy of cannabis and related products. When considering cannabis products for clinical use, pharmacists should discuss both risks and benefits with the patient and provider. Patients who may benefit most would be those with chronic pain, chemotherapy-induced nausea and vomiting, and multiple sclerosis spasticity. Additionally, pharmacists should review patient medication lists and educate providers on potential drug-drug interactions. For instance, some patients receiving cancer treatment may also be receiving an azole antifungal, which may increase the concentration of both THC and CBD due to CYP3A4 inhibition. On the other hand, certain anticonvulsants (i.e. carbamazepine) may reduce THC and CBD concentrations, resulting in decreased effects of the cannabis product. Additionally, it is important to consider patient-specific factors when determining whether cannabis or cannabinoids would be useful, and what dosage form may be preferable. Patients with uncontrolled blood pressure or those with memory or attention deficits may not be the best candidates for cannabis-derived products. For patients with underlying respiratory issues, edible products may be preferred over inhaled formulations. Pharmacists should also educate patients on the risk of impairment and addiction, as well as obtaining products from a licensed source to minimize the risk of adulteration or contamination. Continued follow-up with the patient and monitoring for efficacy and side effects should be implemented if a cannabis product is initiated.
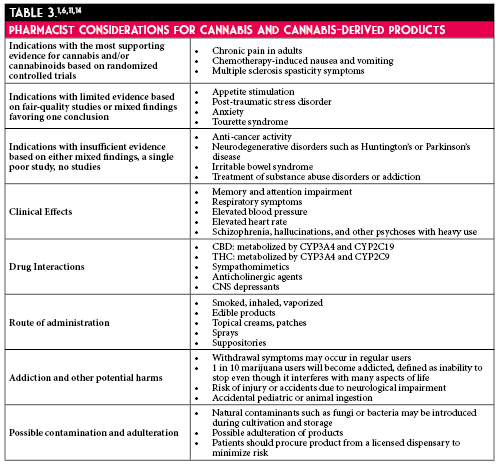
Considerations for pharmacists managing patients who choose to use cannabis and cannabis-derived products are summarized in Table 3.
As cannabis and related products become more widely used in both the recreational and medical settings, it is meaningful for pharmacists to have an adequate understanding of these substances. Open conversations on the risks and benefits, comprehensive medication and social histories, and routine monitoring are steps pharmacists can take as the use of these products continues to increase.
Additional Resources