Print This Article
Educational Affairs
A New Year and New Goals: Release of the 2017 ACC/AHA Hypertension Guidelines Provide Clarity to the Controversy of Blood Pressure Management
by Elizabeth Van Dril, PharmD, BCPS PGY-2, Ambulatory Care Resident Midwestern University Chicago College of Pharmacy; Ryan Bagnell, PharmD, Candidate Midwestern University Chicago College of Pharmacy; Jen Phillips, PharmD, BCPS, FCCP, FASHP Associate Professor, Pharmacy Practice, Midwestern University Chicago College of Pharmacy
In November, the American College of Cardiology (ACC) and American Heart Association (AHA) released the new clinical practice guideline on the management of hypertension at the AHA 2017 Scientific Sessions.
1 The guidance document, published simultaneously in the Journal of the American College of Cardiology and Hypertension, was a long-awaited update to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-7), which was issued in 2003 by the National Heart, Lung and Blood Institute (NHLBI).
2 The Eighth Joint National Committee (JNC-8) and several other individual organizations have published less comprehensive guidelines and expert consensus statements since the publication of the JNC-7. However, none were as extensive or widely endorsed in clinical practice.
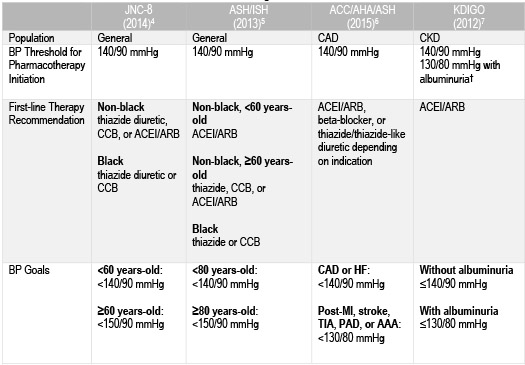
3 The JNC-8, American Society of Hypertension and the International Society of Hypertension (ASH/ISH), the International Society of Nephrology Kidney Disease, Improving Global Outcomes (KDIGO) guidelines, as well as the consensus statement from AHA/ACC/ASH for patients with comorbid coronary artery disease vary in their blood pressure (BP) thresholds for pharmacotherapy initiation, first-line therapy recommendations and BP goals (Table 1).
4-7 The 2017 ACC/AHA hypertension guidelines aimed to provide clear and concise recommendations for BP management to alleviate the controversy that was generated by often conflicting previous guidelines and consensus statements.
Table 1: Recommendations from Previous Guidelines and Organizational Consensus State
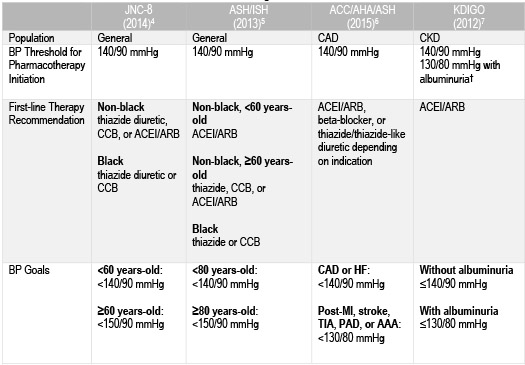
†Albuminuria: ≥30 mg/24h or urinary albumin-to-creatinine ratio (UACR) ≥30 mcg/mg creatinine
Abbreviations: CAD = coronary artery disease; CKD = chronic kidney disease; HF = heart failure; MI = myocardial infarction; TIA = transient ischemic attack; PAD = peripheral artery disease; AAA = abdominal aortic aneurysm
The ACC and AHA were given the stewardship by the NHLBI Advisory Council to develop a comprehensive, yet succinct resource for clinicians and public health practices.1 The new 2017 guidelines are a collaborative effort by ACC, AHA and nine other professional organizations: American Academy of Physician Assistants, American College of Preventive Medicine, American Geriatrics Society, American Pharmacists Association, American Society of Hypertension, American Society of Preventive Cardiology, Association of Black Cardiologists, National Medical Association and Preventive Cardiovascular Nurses Association.
The new 2017 ACC/AHA guidelines lower the BP threshold that defines hypertension and recommend a more stringent universal BP target of <130/80 mmHg.1 The change in BP goal is based largely on the results from the SPRINT trial, which demonstrated a decrease in cardiovascular events in patients treated to a systolic blood pressure (SBP) of less than 120 mmHg compared to routine management with a SBP goal of less than 140 mmHg.8 The new treatment goals are expected to increase the U.S. prevalence of hypertension from 32 to 46%.1 Additionally, upon initiation of pharmacotherapy, authors recommend that patients should be reassessed and medications titrated monthly until BP goals are achieved (COR I, LOE B-R). These recommendations may be challenging for primary care physicians to implement on their own. Therefore, the guidelines endorse a team-based care approach (COR I, LOE A), which carves out a role for pharmacists practicing with collaborative agreements to assist with the increased number of patients who may require BP management and provides the profession another avenue to demonstrate value through improved patient outcomes. Understanding the major recommendations of the ACC/AHA 2017 hypertension guidelines and the evidence that shaped them will aid pharmacists in being successful in the implementation of these recommendations and ultimately, lead to improvement in patient outcomes.
Changes in BP Classification and Recommendations for Treatment
The new guidelines separate BP into four separate categories: normal BP, elevated BP, and Stage 1 and 2 hypertension, which differ slightly from the categories designated by JNC-7 as described in Table 2.1,2 The shift in clinical definitions comes as a result of the mounting observational evidence indicating a progressively higher risk of cardiovascular mortality with an increase in BP. Specifically, the risk doubles for each 20 mmHg increase in SBP and 10 mmHg increase in diastolic blood pressure (DBP).9
Table 2. Blood Pressure (BP) Classification According to JNC-7 and 2017 ACC/AHA Guidelines
|
SBP and/or DBP (mmHg)
|
JNC-72
|
2017 ACC/AHA1
|
|
<120 and <80
|
Normal BP
|
Normal BP
|
|
120–129 and <80
|
Prehypertension
|
Elevated BP
|
|
130–139 or 80–89
|
Prehypertension
|
Stage 1 hypertension
|
|
140–159 or 90–99
|
Stage 1 hypertension
|
Stage 2 hypertension
|
|
> 160 or >100
|
Stage 2 hypertension
|
Stage 2 hypertension
|
The reclassification of BP is expected to result in an increase in the prevalence of patients diagnosed with hypertension. However, this may not translate to an equivalent increase in the number of patients being prescribed pharmacotherapy for hypertension.1 This is primarily due to the incorporation of the 10-year atherosclerotic cardiovascular disease (ASCVD) risk assessment into the decision to initiate treatment (Figure 1). Patients without established cardiovascular disease (CVD) should have their 10-year ASCVD risk calculated before deciding to start antihypertensive pharmacotherapy. Patients with a 10-year risk <10% can elect to utilize lifestyle modifications alone if they are in stage 1 hypertension; however, these lower-risk patients are indicated for treatment with BP-lowering medications in stage 2 hypertension for primary prevention of CVD (COR I, LOE C-LD). Patients with clinical ASCVD and those without clinical ASCVD with a 10-year risk ≥10% should be initiated on BP-lowering therapy, in addition to lifestyle modifications, immediately if they are classified as having stage 1 hypertension or greater for secondary and primary prevention of CVD, respectively (COR I, LOE A).
Figure 1. BP Thresholds and Treatment Recommendations
Adapted from Whelton et al. Hypertension.
One Goal: 130 is the “New 140” for Everyone
Regardless of the threshold for initiating pharmacological treatment, a BP target of <130/80 mmHg is now recommended for all adult patients with hypertension and clinical ASCVD or a 10-year ASCVD risk ≥10% (COR I, LOE B-R).1 Additionally, the guidelines state that it is reasonable to maintain this goal for patients without additional markers of increased CVD risk or with a 10-year ASCVD risk <10% (COR I, LOE B-NR). Historically, BP goals have been adjusted based on patient age and comorbidities, such as diabetes, cardiovascular disease and chronic kidney disease. The new ACC/AHA recommendation to target <130/80 mmHg includes patients with those comorbidities and provides more specific guidance as to what to consider as first-line agents in the presence of such disease states. Of note, the American Diabetes Association (ADA) 2018 Standards of Medical Care released this past December continued to recommend a BP target of <140/90 mmHg for patients with diabetes, with the option of decreasing that goal to <130/80 mmHg in patients with high risk for CVD.10 The ADA chose not to adapt the more stringent BP target since patients with diabetes were specifically excluded from the SPRINT trial.8 Whether the ADA continues to recommend the more lenient BP target will depend on their interpretation of the meta-analyses of randomized controlled trials and observational data that helped shape the ACC/AHA recommendation for lower targets, even in patients with diabetes.1 This universal recommendation does not preclude the use of clinical judgement; it is still necessary to assess the risk-benefit profile when considering a BP goal of <130/80 mmHg in older adults.
Preference for Out-of-Office BP Measurements
The use of out-of-office BP monitoring to confirm diagnosis of hypertension, guide titration of medications and rule out both white coat and masked hypertension is now preferred over in-office BP measurement (COR I, LOE A).1 This recommendation is based on the growing body of evidence that out-of-office BP measurement techniques, such as home BP monitoring and ambulatory BP monitoring, are better predictors of cardiovascular events compared to office-based BP measurement.11 The limitations of this recommendation are the cost of purchasing a home BP monitor to patients, the health-system costs of implementing ambulatory BP monitoring, as well as the concern for the lack of adequate training and improper use of these devices outside of the office setting. In the absence of out-of-office BP measurements, guidelines recommend that the diagnosis of hypertension and determination of BP control be made on the average of ≥2 readings from ≥2 different office visits (COR I, LOE C-EO).
Recommendations for Initial Treatment Options Remain Unchanged
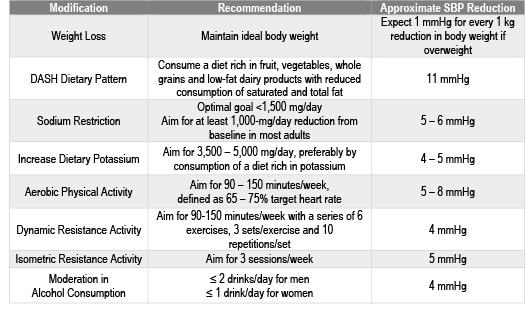
Non-pharmacologic therapy is indicated for all patients with elevated BP and confirmed hypertension.1 The BP-lowering that is anticipated as a result of these lifestyle modifications is now documented in the guideline (COR I, LOE A) and is a valuable tool for encouraging the implementation of these interventions (Table 3). It is important to note that these non-pharmacological interventions certainly do not have to be limited to patients with hypertension. Many patients with “normal” BP can also benefit from lifestyle modifications to prevent the onset of hypertension.
Table 3. Non-pharmacologic Interventions and Estimated SBP Reduction in Patients with Hypertension
Adapted from Whelton et al. Hypertension.
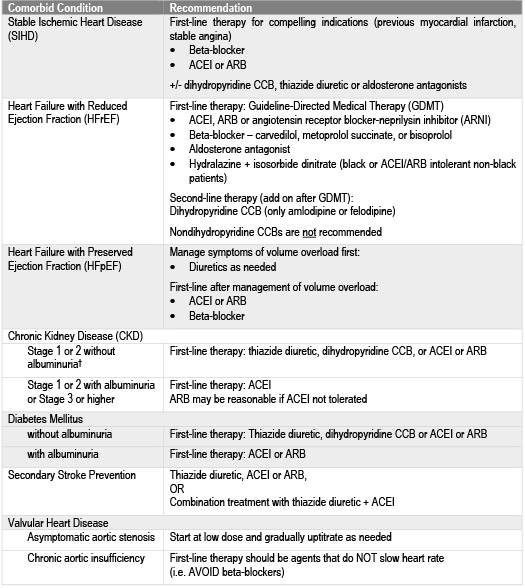
First-line pharmacotherapy for non-black patients without a compelling indication continues to be calcium channel blockers (CCBs), thiazide diuretics, and either angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) (COR I, LOE A).1 Thiazide diuretics or CCBs are considered first-line for black patients without a compelling indication (COR I, LOE B-R). These initial therapy options mirror the recommendation from JNC-8.1,4 The guidelines specifically state that chlorthalidone is preferred to hydrochlorothiazide on the basis of prolonged half-life and the CVD-reduction data from clinical trials.1 They also now explicitly recommend against the simultaneous use of ACEIs, ARBs and/or direct renin-inhibitors as a result of the ONTARGET and ALTITUDE trials, which demonstrated a lack of clinical benefit and increased adverse effects (e.g. hyperkalemia, hypotension and renal impairment) with combinations of these agents (COR III:Harm, LOE A).1,12,13 Clinical considerations for BP-lowering drug classes and individual agents are included within the guidance document, along with initial treatment recommendations for patients with hypertension and specific comorbid conditions (Table 4).
The guidelines have also reinforced the recommendation to initiate two BP-lowering agents from different classes in patients with stage 2 hypertension (COR I, LOE C-EO), which was originally recommended in the JNC-7 guidelines.1,2 This is based on the evidence supporting low-dose combination therapy in patients with a SBP >20 mmHg or DBP >10 mmHg above goal.1 Using a fixed-dose combination product titrated to a BP <130/80 mmHg to implement this recommendation is a reasonable approach while minimizing patients’ pill burden and costs of treatment.
Table 4: Initial Medication Therapy Recommendations Based on Comorbid Conditions
†Albuminuria: ≥30 mg/24h or urinary albumin-to-creatinine ratio (UACR) ≥30 mcg/mg creatinine
The Bottom Line
The 2017 ACC/AHA guidelines are the collaborative response to the almost 15-year gap in clinical practice guidance for the prevention, detection, evaluation and management of patients with hypertension. Since the publication of JNC-7, clinical trial and observational data has been accumulating without definitive recommendations from a comprehensive guideline on how to use the evidence in clinical practice. The reclassification of BP readings and endorsement of a lower universal BP goal reflects the aggregate of observational data demonstrating a graded increased risk in CV mortality with elevations in BP. This strong association, as well as the risk of other complications from uncontrolled hypertension, should be communicated to patients during collaborative discussions of when to start or adjust BP-lowering therapy.
Pharmacists and other healthcare clinicians should be aware of these recommendations when treating patients with hypertension. In addition, the dissemination of recommendations in the form of education to patients and other healthcare providers will determine the impact of the ACC/AHA guideline on the burden of CVD and serve as a potential opportunity for pharmacists to demonstrate their value in new collaborative models of care. While pharmacists continue to expand their presence in the ambulatory care environment, they are in a unique position to counsel patients not only on their drug therapy, but on the impact of non-pharmacological, lifestyle modifications on hypertension.
References:
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/ AHA /AAPA /ABC /ACPM /AGS /APhA /ASH /ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 13, 2017]. Hypertension.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and the treatment of high blood pressure. Hypertension. 2003;42:1206-52.
- Jeffrey S. Medscape: New ACC/AHA Hypertension Guidelines Make 130 the New 140.www.medscape.com/viewarticle/888560 (accessed 2017 Dec 10).
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National committee (JNC8). JAMA. 2014;311(5):507-20.
- Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15.
- Rosendorff C, Lackland DT, Allison M, et al. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation. 2015;131:e435-70.
- KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl, 2012; 2(5):337-414.
- SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015 Nov 26;373(22):2103-16.
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903-13.
- American Diabetes Association. Standards of Medical Care in Diabetes – 2018. Diabetes Care. 2018;41(1):S1-S159.
- Reino-Gonzalez S, Pita-Fernández S, Seoane-Pillado T, et al. How in-office and ambulatory BP monitoring compare: A systematic review and meta-analysis. J Fam Pract. 2017;66(1):E5-E12.
- Mann JFE, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372(9638):547-53.
- Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med. 2012;367(23):2204-13.