Print Entire Issue

KeePosted Info
Columns
President's Message
Directly Speaking
Government Affairs Report
Educational Affairs
Leadership Profile
Medication Safety Pearl
Board of Pharmacy Update
Hi Tech
New Practitioners Network
ICHPeople
College Connections
Chicago State University College of Pharmacy
Southern Illinois University Edwardsville School of Pharmacy
University of Illinois at Chicago College of Pharmacy
More
Welcome New Members!
Officers and Board of Directors
ICHP Pharmacy Action Fund (PAC) Contributors
Upcoming Events
KeePosted Info
Illinois Council of Health-System Pharmacists
4055 North Perryville Road
Loves Park, IL 61111-8653
Phone: (815) 227-9292
Fax: (815) 227-9294
ichpnet.org
KeePosted
Official Newsjournal of the Illinois Council of Health-System Pharmacists
EDITOR
Jacob Gettig
ASSISTANT EDITOR
Jennifer Phillips
MANAGING EDITOR
Scott Meyers
ASSISTANT MANAGING EDITOR
Trish Wegner
DESIGN EDITOR
Amanda Wolff
ICHP Staff
EXECUTIVE VICE PRESIDENT
Scott Meyers
VICE PRESIDENT - PROFESSIONAL SERVICES
Trish Wegner
DIRECTOR OF OPERATIONS
Maggie Allen
INFORMATION SPECIALIST
Heidi Sunday
CUSTOMER SERVICE AND
PHARMACY TECH TOPICS™ SPECIALIST
Jo Ann Haley
ACCOUNTANTS
Jan Mark and Trisha Blassage
COMMUNICATIONS MANAGER
Amanda Wolff
LEGISLATIVE CONSULTANT
Jim Owen
ICHP Mission Statement
Advancing Excellence in Pharmacy
ICHP Vision Statement
ICHP dedicates itself to achieving a vision of pharmacy practice where:
- Pharmacists are universally recognized as health care professionals and essential providers of health care services.
- Patients are aware of the training, skills, and abilities of a pharmacist and the fundamental role that pharmacists play in optimizing medication therapy.
- Formally educated, appropriately trained, and PTCB certified pharmacy technicians manage the medication distribution process with appropriate pharmacist oversight.
- Pharmacists improve patient care and medication safety through the development of effective public policies by interacting and collaborating with patients, other health care professionals and their respective professional societies, government agencies, employers and other concerned parties.
- Evidence-based practices are used to achieve safe and effective medication therapies.
- There are an adequate number of qualified pharmacy leaders within the pharmacy profession.
- Pharmacists take primary responsibility for educating pharmacy technicians, pharmacy students, pharmacist peers, other health professionals, and patients about appropriate medication use.
KeePosted Vision
As an integral publication of the Illinois Council of Health-System Pharmacists, the KeePosted newsjournal will reflect its mission and goals. In conjunction with those goals, KeePosted will provide timely information that meets the changing professional and personal needs of Illinois pharmacists and technicians, and maintain high publication standards.
KeePosted is an official publication of, and is copyrighted by, the Illinois Council of Health-System Pharmacists (ICHP). KeePosted is published 10 times a year. ICHP members received KeePosted as a member benefit. All articles published herein represent the opinions of the authors and do not reflect the policy of the ICHP or the authors’ institutions unless specified. Advertising inquiries can be directed to ICHP office at the address listed above. Image disclaimer: The image used in the Pharmacy Tech Topics™ advertisement is the property of © 2016 Thinkstock, a division of Getty Images. The image used in the Happy Holidays advertisement is the property of © 2016 Adobe Stock.
Copyright © 2016, Illinois Council of Health-System Pharmacists. All rights reserved.
Columns
 President's Message
President's Message
Baby Steps
by Charlene Hope, PharmD, MS, BCPS, ICHP President
Mathieu Mottrie, CEO at CREAX, an innovation consulting and research firm, defines innovation as making changes that add business value, in terms of either revenue growth or increased operational efficiency. This value can be created in four ways: introducing new products; optimizing operational processes; launching new business models; and entering new markets. Based on this definition, hospital/health-system pharmacies are constantly innovating whether it is adding a new drug to the hospital formulary, optimizing the automating dispensing units stocking process, starting a new ambulatory care service or expanding a specialty pharmacy program. To me, there is one word in his definition that is the “innovation-limiting step” – change. And maybe it is more like the fear of change.
“Baby Steps” is a mantra that I often use usually at the time I sense the fear of change starting to makes its way into a team discussion and usually after the team has participated and agreed with moving forward with a process change. It is fairly easy to detect fearful questions because they usually start with what if..? and end with numerous potential unforeseen situations that may or may not be under the control of the team. This is also known as Analysis Paralysis (AP) – overanalyzing a situation to the point where a decision or action is never taken and is thereby “paralyzed” or halted. Our ability to analyze is one of our core strengths and while striving for finding the perfect solution to a problem, we are especially prone to succumbing to AP as pharmacists. But I have found that responding to the what ifs? with my mantra “Baby Steps” often helps break the spell. I still acknowledge the concerns and potential barriers that are expressed by the team; however, I do not allow it to prevent us from taking the first step since it is the first small step that matters. As I was thinking about when I started using this mantra, I realized that there were more connections to be made between baby steps and leading change to innovation.
I am fortunate to be a member of very large extended family. My mom is one of the oldest of nine children and my dad, one of the oldest of a family of eleven. With over 40 first cousins, I have had my share of playing with baby cousins as they were learning how to walk. There is something about the process of learning how to walk. From rolling over, to crawling, standing up, holding on to the nearest chair or couch, to finally taking those first few wobbly independent steps. I think about along the way how parents, siblings and other family members or friends celebrate this journey to the first baby step wins along the way. We don’t wait until the baby is finally walking to cheer them on and shower them with hugs and kisses. It occurs over time by building the baby’s confidence throughout each phase of the process. Contrary to popular belief, innovation is not a once in lifetime light bulb moment. Innovating is about making small informed changes over time, building on small wins until successfully achieving the intended goal.
Most babies also do not walk long distances the first time. It starts with a series of a few confident wobbly steps and falling down over and over again. The most important thing babies do is get back up, and do it again. How many times do we give up on a new process change or project at the first signs of things going south – then abandon it all together? The truth is numerous attempts may be needed over time, addressing issues or barriers as they arise while building confidence. What do parents, siblings and family members do after baby falls down? Check for injuries, calm the crying baby and say a few soothing words of encouragement (slow down, you’re okay, etc.). Being innovative means being resilient and managing the fear associated with change one step at a time.
The next time you want to try an idea at work, consider running a pilot, which can be conducted with one patient, in one nursing area, over one hour, one shift, or one day. Take the baby step; if successful, celebrate and take the next step. Take the next baby step and perhaps this time there may be a wobble or a fall. Identify what went well, address and fix what did not (+/- crying), take a deep breath and take the next step. Who knew that learning to walk could teach us about change and innovation? So, the next time you or your team starts to feel the paralysis of fear creeping in…don’t forget, and repeat after me, “Baby Steps.”
 Directly Speaking
Directly Speaking
Does Your Doctor’s Office Have Its Own Pharmacist?
by Scott A. Meyers, Executive Vice President
It should! And if they don’t, are you doing anything about it? Most academic medical centers have placed pharmacists in physician clinics to add an important component to the team that already exists. Soon, if they haven’t already, many more non-academic health-systems will add their own pharmacists to these physician offices, and the evolution of the medical model will continue.
And that’s a great thing! With the changes in reimbursement models through Medicare Access and CHIP Reauthorization Act (MACRA) and CMS’s final rules for it, there will be new opportunities for pharmacists to become more involved in the medication use process with more emphasis on the prescribing, monitoring and adjusting of medication therapy in the same office as the physician.
If you’re not familiar with MACRA and its rules, don’t feel bad. It’s not a common topic for most pharmacists. But for those few whose job it is to monitor and respond to these types of issues, it is exciting news! Pharmacist provider status may not be as necessary as we have believed, although that’s not to say we won’t be working to change the Pharmacy Practice Act and Medicaid and Insurance Codes so that no matter what the payment model is, pharmacists can be an integral member of the team from both a care and a compensation standpoint. After all, the more we impact the bottom-line in both savings and revenue, the more valuable we are to the model and the team.
If working in a physician’s office is something you’re aiming for, it may not be far off. But even if the laws and rules are slow to change, you should always be discussing your or other pharmacists’ roles with every doctor you meet. As a matter of fact, thanks to an insurance provider change with ICHP, I’m meeting a new doctor in December. Depending on how our first interaction goes, I may encourage him to consider hiring a pharmacist in his clinic. I will do this knowing full well that he’s not going to be the decision maker on this and that because he is part of a large health-system, the decision will have to be made at a much higher level. However, I intend to plant a seed where perhaps none have been planted before and see if the ground is fertile.
It will be interesting to see how my first visit goes and whether he’s open to conversations like this. But I really think that’s how pharmacy is going to win this battle and move from the product to the patient – by talking with those who can use the expertise pharmacists provide as often as possible and in a non-confrontational way. Share what you know and what you see, both in their practice setting and in healthcare in general. Talk about the primary care shortage and how pharmacists can be physician extenders just like PAs and APNs only with much more knowledge of medications and the issues that surround them. There is always something we can do to move the needle on any issue. But we all have and work with doctors, so why not talk to them now?
Does your doctor’s office have its own pharmacist? It should!
Government Affairs Report
Presidential Election Shocker: Subtle Changes in the General Assembly
by Jim Owen and Scott A. Meyers
Very few prognosticators got it right. Half of America is disappointed, and the other half is excited. None of this should be news to any of you, but Donald Trump will be inaugurated on Friday, January 20th, 2017. He will become the 45th President of the United States of America.
Whichever side you stood on before the election, we encourage each and every one of you to respect the office of President and pray for his and the country’s success. And that’s all we’re going to say about that.
But in Illinois, the election results were a little more subtle or subdued. While the Democrats still maintain a majority in both chambers creating a stalemate with the Republican Governor, the numbers changed slightly in favor of the Republicans, which will have some repercussions for the next two years.
In the Senate, President Cullerton (D) held on to a one-vote supermajority, losing two previously democratic seats to republican challengers. On the House side, Speaker Madigan, in a very expensive battle with the Governor and his funds, lost four seats and his supermajority of one vote. So he now needs at least three republican lawmakers to side with him in order to override any Governor veto!
Perhaps this was Speaker Madigan’s plan all along, although we doubt that based on the money he spent to retain those seats. By losing his supermajority, one that he was unable to manage well against the Governor last session, he now can blame republicans for not pitching in to get the job done in Springfield.
What may have been the most troubling about this year’s election was that just under 62% of the seats up for election in both the House and the Senate were uncontested in the general election! This means Illinois residents did not really have a choice when selecting their representation in Springfield nearly two-thirds of the time! Whether you normally vote for democrats or republicans or you mix it up based on the best qualified candidate (which we always hope is the case), you’re cheated out of even considering a choice when there is none.
The lack of choice can be blamed primarily on the legislative districts map. For those who may not remember, in the State of Illinois there are 59 Senate districts and 118 House of Representative Districts. That’s two House districts per Senate district. If you want to see some creative boundaries, take a look at the map found at Illinois Legislative Districts. While the Senate districts downstate are somewhat rationally drawn, you will truly wonder if the map makers were crazy when drawing up the northeastern Illinois legislative districts. But the honest answer is that they were crazy like foxes! Many of the districts both downstate and in the Chicago metropolitan area have the boundaries they do so that one party or the other has a supermajority of voters in each. This makes it hard for the other party to find viable candidates in many districts and even harder to win elections.
While the change in the make-up of the General Assembly was subtle as mentioned, it will be interesting to see if there is no change or a dramatic change beginning on the second Wednesday in January of 2017. It is never too early or too late to get involved in the legislative process, and over 80% of the statutes and regulations governing pharmacy come from the State level, so get informed and get involved! After all, the next big election in Illinois is less than two years away!
Educational Affairs
A Split Decision? Considerations for Splitting Tablets
by Tanja Alavanja, PharmD Candidate, University of Illinois at Chicago; Lara Ellinger, PharmD, BCPS, Drug Information / Medication Safety Pharmacist, Northwestern Memorial Hospital
Introduction
The purpose of tablet splitting proposes the physical divisibility of a tablet into two equal halves.1 However, half tablets derived from tablet splitting may not be uniform in dose and, technically, may be considered an off-label use of the drug.2 The reasons reported for tablet splitting include dose flexibility or titration - specifically, in the geriatric and pediatric patient populations, facilitation of swallowing tablets that would otherwise be too large.3,4,5,6 Other reasons include reduced cost from splitting flat-priced tablets. It has been reported that splitting tablets may potentially reduce the cost per dose by approximately 50% when the cost among various tablet strengths of a medication are similar to one another.6,8 Even though some physicians and insurance companies recommend tablet splitting to their patients, professional organizations seem to disagree with this practice.5 In 2000, the American Society of Consultant Pharmacists released a position statement opposing policies by healthcare payers that require mandatory tablet splitting to get lower doses instead of reimbursing for lower strength whole tablets. The American Medical Association (AMA) and the American Pharmacists Association (APhA) followed with similar opposition.2,9,10,11 Similarly, the Institute for Safe Medication Practices issued a Safety Alert in 2006 advising against tablet splitting when lower strength dosage forms were available.12 If the desired dose for a patient was not commercially available, it provided guidance to inpatient and outpatient healthcare professionals to follow to ensure tablets were split safely. The U.S. Food and Drug Administration’s (FDA) Center for Drug Evaluation and Research has suggested possible safety issues surrounding tablet splitting.5 However, tablet splitting has been reported to be accepted by patients and not significantly interfere with their ability to adhere to a drug therapy regimen.7 The contention surrounding the practice of tablet splitting warrants a closer evaluation of the body of evidence that has emerged, which includes the FDA’s influence on regulating tablet splitting, tablet characteristics that influence tablet splitting, and the various methods available to split tablets.
FDA Guidance
In 2009, the FDA issued a Consumer Report addressing the practice of splitting tablets.13 It stated that the FDA and AMA, amongst other organizations, advised against tablet splitting unless specified in the drug’s labeling. Following this Consumer Report, a stimuli article was published proposing the inclusion of standards in the United States Pharmacopeia (USP) for the accuracy of subdivided parts of scored tablets in order to reduce the risk related to variable doses derived from tablet splitting.4 The authors of the article suggested that uniformity of mass and weight variation standards of the subdivided parts of a scored tablet could be extrapolated from USP General Chapter <905>, (Uniformity of Dosage Units), for whole dosage forms. Additionally, the authors advocated for scored tablets to meet certain criteria of accuracy and loss of mass during registrations in a New Drug Application (NDA) or Abbreviated New Drug Application (ANDA). Consequently, in 2013, the FDA issued a Guidance for Industry on tablet scoring, which indicated criteria that scored tablets would need to meet as part of the review of a NDA or an ANDA in order to bear the term “functional scoring” in the package insert.5 Some of the criteria provided in the guidance document reflect the standards set forth by the USP General Chapters <905> (Uniformity of Dosage Units) and <1216> (Tablet Friability). The guidance document indicates that a scoring feature or reference to one should be absent in the package labeling if the all the criteria outlined in the document are not met. Prior to the FDA guidance, the European Pharmacopoeia (2002), Health Canada (2003), and the International Pharmacopoeia, maintained by the World Health Organization, (2011), outlined standards for the characteristics of scored tablets and the handling of their subdivided parts.4,6,14,15
Tablet Characteristics
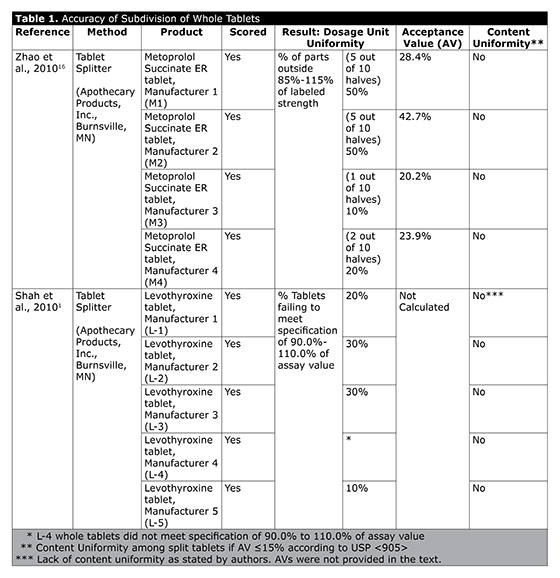
Research has shown that some tablets may be more appropriate to split than others.8 Tablets suitable for splitting contain drugs with long half-lives, wide therapeutic windows and are scored, flat, oblong, and larger in size (≥8 mm diameter). Tablets unsuitable for splitting include those that are enterically coated and small in size, have increased fragmentation and powdering upon breaking, or contain drugs with narrow therapeutic windows. In a study examining the content uniformity of scored extended-release (ER) metoprolol succinate half tablets that were split with a tablet splitter, it was determined that the metoprolol succinate coated beads were heterogeneously dispersed throughout the tablet.16 As a result of this uneven distribution of the active pharmaceutical ingredient, ER metoprolol succinate half tablets were determined to be greater than or less than the intended half-strength dose that a scored tablet should provide. Similarly, it was determined that splitting scored levothyroxine tablets, a drug with a narrow therapeutic window, by hand or with a tablet splitter, produced half tablets that were increasingly friable and failed content uniformity testing.1 A summary of the findings can be found in Table 1. A study examining the laboratory outcomes of atorvastatin, lovastatin, and simvastatin half-tablets resulted in no changes in total cholesterol and triglycerides, a statistically significant decrease in low density lipoprotein (P<0.001), a statistically significant increase in high density lipoprotein (P<0.001), and statistically significant increases in aspartate transaminase (AST) (P<0.001) and alanine transaminase (ALT) (P= 0.006).8 These results were measured before and after the patients were on a stable dose of one of the medications at least 6 weeks before and at least 6 weeks after the point of splitting the tablet. The authors reported that the increased values in AST and ALT were within normal limits and not clinically significant. They also concluded that the clinical significance of tablet splitting could not be determined in their setting due to the lack of control of lifestyle modifications which may have positively impacted improved LDL and HDL levels. However, these results seem to suggest that half tablets of agents with a wide therapeutic window may not be less effective than whole tablets of approximately equal strength.
Tablet Splitting Methods
The various methods to split tablets include by hand or with a splitting device, scissors, a razor blade, or a kitchen knife.8 Available literature seem to provide conflicting evidence for the method most likely to provide half tablets of similar weight and content uniformity. One study demonstrated that a splitting device was superior to hand splitting, while another study demonstrated that hand splitting provided better results than a splitting device or a kitchen knife.17,18
A tablet splitting program established in April 2000 at the Veterans Affairs Palo Alto Health Care System excludes a list of medications from the program because their physical or chemical characteristics deem them unsuitable for splitting.3 Through this program, patients receive education on how to split tablets with a tablet splitter prior to performing the practice individually; however, it has been noted that patients with cognitive and physical barriers may not be the best candidates to split tablets. Due to the conflicting evidence on the best available method to split a tablet, it has been suggested that patients receive instruction from pharmacists to learn how to accurately split tablets.8 Furthermore, pharmacists may split tablets for their patients as a compounding service in order to provide a drug product tailored to a patient’s needs.9 According to Section 503A of the Food and Drug Administration Modernization Act (FDAMA) of 1997, pharmacists may compound drug products that are not “copies of a commercially available drug product.”9,19 Therefore, splitting tablets to provide a dose of drug that is lower than the lowest commercially available strength seems to adhere to the FDAMA compounding statute.9
Conclusion
Since issuing the Guidance for Industry on tablet splitting, the FDA has also issued a Best Practice for Tablet Splitting which, among other recommendations, advises patients to speak to a healthcare professional before splitting a tablet and to split tablets one at a time as needed.20 When deciding to split tablets for patients, pharmacists may need to consider the legal aspects implicated in the practice, the time it may take to split the tablets, and the benefits of having a pharmacist perform the service versus the risk of having the patients split tablets at home without pharmacists’ supervision. The available evidence seems to support the practice of tablet splitting for a restricted list of medications bearing certain physical and chemical characteristics. Accordingly, prior to a pharmacist making the recommendation to split a tablet, the patient’s capacity to split tablets should be assessed and recommendations from the FDA and other primary literature should be consulted in order to completely evaluate the tablet’s characteristics to determine if it can be split to avoid potential compromise in efficacy or safety.
References
- Shah RB. Collier JS, Sayeed VA, Bryant A, Habib MJ, Khan MA. Tablet splitting of a narrow therapeutic index drug: A case of levothyroxine sodium. AAPS PharmSciTech. 2010;11(3):1359-1367.
- Noviasky J, Lo V, Luft DD. Which medications can be split without compromising efficacy and safety? J Fam Pract. 2006;55(8):707-708.
- Freeman MK, White W, Iranikhah M. Tablet splitting: a review of the clinical and economic outcomes. The Consultant Pharmacist. 2012;27(6):421-430.
- Green G, Berg C, Polli JE, Barends DM. Pharmacopeial standards for the subdivision characteristics of scored tablets. Pharmacopeial Forum. 2009;35(6):1598-1612.
- Guidance for industry tablet scoring: Nomenclature, labeling, and data for evaluation. Silver Spring, MD: U.S. Food and Drug Administration; 2013.
- Reddy YV, Venkatesh MP, Pramod Kumar TM. Tablet scoring and its regulatory perspective. Applied Clinical Research, Clinical Trials & Regulatory Affairs. 2014;1(2):107-110.
- Gee M, Hasson NK, Hahn T, Ryono R. Effects of a tablet-splitting program in patients taking HMG-CoA reductase inhibitors: Analysis of clinical effects, patient satisfaction, compliance, cost avoidance. J Manag Care Pharm. 2002;8(6):453-458.
- Helmy SA. Tablet splitting: Is it worthwhile? Analysis of drug content and weight uniformity of half-tablets of 16 commonly used medications in the outpatient setting. J Manag Care Pharm. 2015;21(1):76-86.
- Clark RT. Tablet splitting for cost containment. American Society of Consultant Pharmacists Web site. https://www.ascp.com/articles/tablet-splitting-cost-containment. Accessed August 20, 2016.
- ASCP Policy Statement on Mandatory Tablet Splitting for Cost Containment. American Society of Consultant Pharmacists Web site. https://www.ascp.com/articles/ascp-policy-statement-mandatory-tablet-splitting-cost-containment. Accessed August 20, 2016.
- Tablet splitting: Evaluating appropriateness for patients. J Am Pharm Assn. 2004;44(3):324-325.
- ISMP Medication Safety Alert. 2006;11(10).1-3.
- Food and Drug Administration. Tablet splitting: A risky practice. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm171492.htm. Published July 21, 2009. Accessed August 20, 2016.
- Drugs and Health Products. Quality Guidance: Applications for drug identification numbers (DINAs) for pharmaceuticals. Health Canada. http://www.hc-sc.gc.ca/dhp-mps/prodpharma/applic-demande/guide-ld/chem/dinas_ddin-eng.php. Published July 2003. Accessed August 20, 2016.
- World Health Organization. Revision of monograph on tablets. QAS/09.324. http://www.who.int/medicines/publications/pharmacopoeia/Tabs-GeneralMono-rev-FINAL_31032011.pdf. Published March 2011. Accessed August 20, 2016.
- Zhao N, Zidan A, Tawakkaul M, Sayeed VA, Khan M. Tablet splitting: Product quality assessment of metoprolol succinate extended release tablets. Int J Pharm. 2010;401(1-2):25-31.
- Habib WA, Alanizi AS, Abdelhamid MM, Alanizi FK. Accuracy of tablet splitting: Comparison study between hand splitting and tablet cutter. Saudi Pharm J. 2014;22(5):454-459.
- Van Riet-Nales DA, Doeve ME, Nicia AE, Teerenstra S, Notenboom K, Hekster YA, van den Bemt BJF. The accuracy, precision, and sustainability of different techniques for tablet subdivision: Breaking by hand and the use of tablet splitter or a kitchen knife. Int J Pharm. 2014;466(1-2):44-51.
- Food and Drug Modernization Act of 1997, 1 USC §503A (1997). http://www.fda.gov/RegulatoryInformation/Legislation/SignificantAmendmentstotheFDCAct/FDAMA/FullTextofFDAMAlaw/default.htm
- Food and Drug Administration. Best practices for tablet splitting. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/ucm184666.htm. Published August 23, 2013. Accessed August 20, 2016.
Leadership Profile
Clara Gary, CPhT, ICHP Technician Representative
 Where did you grow up and go to school?
Where did you grow up and go to school? I grew up in Chatham on the Southside of Chicago where I attended St. Felicitas Catholic School. I graduated from St. Willibrord Catholic in Roseland and then began to work on my bachelor’s degree in chemistry at Rosary College in Riverforest, IL. I recently returned to finish my degree at Governor’s State University in 2014 and am still working toward this goal.
Trace your work history: where have you trained / worked/ any special accomplishments?
I started out in 1988 at Northwestern Memorial Hospital under Desi Kotis and was trained in Wesley and then in Prentice by a great pharmacist, Greg Gregory, and by an awesome technician, Latrice Hardy. I worked there for two years and then went on to spend seven years at Michael Reese Hospital working in every area of the hospital and on all shifts, ending up in the OR Pharmacy. From there I left to go into long-term care at Neighbor Care Pharmacy as a Senior IV technician for seven years before coming to the University of Illinois where I have been for the last 11 ½ years. At UI Health, I started out as the Medication Assistance Program Technician, and then became the Lead Technician. Now I am the Pharmacy Discharge Prescription Service Technician.
Describe your current area of practice and practice setting.
As the Pharmacy Discharge Prescription Services Technician, I work as a Tech III for the department of UI Health Ambulatory Care Pharmacy at Wood Street Pharmacy and within the hospital, under the extraordinary direction of Sandra Durley and Kit Moy.
What initially motivated you to get involved, and what benefits do you see in being active in a professional association such as ICHP?
A pharmacy extern, Oksana Kucher, at UI Health asked me to give a presentation for the 2014 ICHP Annual Meeting after observing me at work. She thought it would be interesting for me to share what I do as part of the discharge transitions of care process with other technicians. So I JOINED ICHP! I want to thank Oksana, who is doing her residency at Princeton University Hospital, for encouraging me to get involved. I haven’t looked back since.
ICHP exposes technicians to people who work in all areas of pharmacy, you just have to come out and network, LEARN, and grow. Find an area that you are passionate about and find yourself a mentor then PARTICIPATE. Since I joined ICHP, I have gotten to work with many great people, but my time spent with the great and humble Dr. Nicholas Popovich for a presentation at the Annual Meeting was especially rewarding.
What advice would you give to a new technician eager to become more involved within ICHP?
ICHP is a gem! It is an organization that listens to technicians – where we can communicate our needs, our wants and our concerns. ICHP has programs to address these concerns and promote our professional growth. I want other technicians to know that you should not limit yourself. Since joining ICHP, I am learning to move outside of my comfort zone and try things that I feared, like public speaking and learning to blog! Go figure, I guess old dogs can learn new tricks!
Pharmacy is not only about counting pills and filling medications, of course those are the basics, but there are all kinds of OPPORTUNITIES out there. There are technicians in research, investigational drugs, nuclear medicine, accredited sterile clean rooms, operating and emergency rooms, procurement, continuous quality improvement, and medication assistance programs to name a few. The sky is the limit, so why limit yourself?
Come out and volunteer to be on a committee at ICHP, become an ICHP Champion and organize the technicians in your area for continuing education (CE) via conference call, or an online group or dinner CE session. One of the best ways is to ATTEND the Spring and Annual meetings, like I first did. Remember that the only way to improve your situation or make any meaningful changes is to GET INVOLVED!
Is there an individual you admire or look up to, or a mentor that has influenced your career?
I have been mentored by some of the BEST pharmacy technicians and pharmacists in the world! My technician mentors are Latrice Hardy, Angela Barnes, Wanda Peterson, Pushap Dhawan and Barbara Crawford! And my pharmacist mentors are Greg Gregory, Annie Hiram, Kit Moy, Ed Donnelly, Hillman Truss and Ravi Oberoi! I thank them each for their leadership and guidance throughout my 28 years; they all have a special place in my thoughts and prayers.
Do you have any special interests or hobbies outside of work?
I love to travel and read, though my life currently hasn’t allowed much of either but I will take a road trip in a heartbeat. And recently, I found that I like to write as well but I do tend to be a tad wordy.
Do you have a favorite restaurant or food?
I love food. I think of myself as lifelong foodie! Waffles or pancakes with strawberries, shrimp fettuccini alfredo or any fajitas are my particular favorites; and my sister makes the best homemade carrot cake ever! It’s delicious! I’m making myself hungry! LOL
What is your favorite place to vacation?
I love to float in the ocean anywhere, but especially in Jamaica, and one time I learned to ski in Winter Park, Colorado with the Sno Gophers Ski Club and it was a BLAST! I fell all down that mountain and loved every minute of it. Swoosh! AAAAAHHHH!
What is the most interesting/unique fact about yourself that few people know?
I am what is called a “House Head”, so I love to dance and go to see live music.
I envisioned, starred in, and then filmed a PSA at Michael Reese Hospital for a National Bone Marrow Registry Drive that I coordinated.
Also, I am the mother of 3 with a 15-year-old and 10-year-old boy/girl twins.
What 3 adjectives would people use to best describe you?
Friendly, helpful and hardworking.
Medication Safety Pearl
Intravenous Administration of Haloperidol
by Brandy Cooper-Kirby, PharmD, Health System Pharmacy Administration Resident; Matthew Dandino, PharmD, Health System Pharmacy Administration Resident; Zahra Khudeira, PharmD, MA, BCPS, CPPS, Medication Safety Officer; Sinai Health System, Mount Sinai Hospital, Chicago, IL
The U.S. Food and Drug Administration (FDA) issued an alert in 2007 revising the prescribing information for haloperidol. The statement recommends electrocardiogram (ECG) monitoring for patients receiving intravenous (IV) haloperidol due to case reports of QT prolongation, Torsades de Pointes (TdP), and sudden death. In addition to at least 28 case reports, a post-marketing analysis identified 229 reports of QT prolongation, including 73 cases of TdP, 11 being fatal. Of the fatal cases, eight involved IV haloperidol. Although adverse cardiac events have been reported in the absence of predisposing factors, the prescribing information advises particular caution in patients with QT-prolonging conditions, underlying cardiac abnormalities, hypothyroidism, familial long QT syndrome, or with drugs known to prolong the QT interval.1
Injectable haloperidol is only approved for intramuscular (IM) administration. Literature suggests the initial basis for IV administration evolved from a series of small, uncontrolled case studies.2 Similarly, the 2002 Clinical Practice Guidelines for the Sustained Use of Sedatives and Analgesics in the Critically Ill Adult recommended IV haloperidol for the treatment of delirium based on a small case series.2,3 Although the recommendation was removed in 2013 Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients (PAD Guidelines) due to lack of evidence, literature suggests that the “off-label” clinical practice of IV haloperidol administration may be relatively common for the management of agitation and delirium, particularly in the intensive care unit (ICU).4,5
A retrospective analysis conducted at Mount Sinai Hospital investigated the clinical practice of IV haloperidol and utilization of ECG monitoring. Mount Sinai Hospital is a safety net hospital located in Chicago, IL. It is a level I trauma center and serves a large psychiatric population. Its emergency department has approximately 65,000 visits per year. A chart review was completed from March 2015 through March 2016, analyzing patients who received at least one dose of IV haloperidol.
Baseline Patient Characteristics
|
N=32 |
Age
< 65 years
≥ 65 years
|
26 (81%)
6 (19%) |
| Male |
25 (78%) |
Unit
ICU
General floor
|
31 (97%)
1 (3%) |
| Baseline QTc (range) |
458 ms (417-634) |
| Number of patients with QTc >500 ms (%) |
3 (9%) |
| Total IV haloperidol administrations |
123 |
| Time from admission to first dose |
42 min |
Number of doses each patient received
One dose
Two doses
|
30
2 |
| Median first haloperidol dose (IQR) |
5 mg (2.5 mg, 5 mg) |
| Number of patients intubated (%) |
17 (53%) |
Comorbidities (%)
Chronic kidney disease
Delirium
Dementia
Depression
Diabetes
Drug/Alcohol Abuse
Epilepsy
Heart failure
Hyperlipidemia
Hypertension
Vascular disease
|
5 (16%)
5 (16%)
2 (6%)
6 (19%)
3 (9%)
13 (41%)
3 (9%)
2 (6%)
3 (9%)
5 (16%)
2 (6%) |
Concomitant QT prolonging medications no (%)
Zero
One
Two
Three
Four |
5 (16%)
9 (28%)
7 (22%)
7 (22%)
4 (13%) |
Baseline Characteristics & Dosing:
Over a one-year period, 49 IV haloperidol orders placed were verified by a pharmacist, resulting in 34 doses administered to 32 patients. Of the orders placed, 11 were scheduled and 23 were as needed. Most of these patients (97%) were located within ICUs; a large amount of patients were also male and <65 years of age. A majority (79%) of the orders were verified outside of the normal hours when a clinical pharmacy specialist is present in the unit. The median first dose administered was 5 mg (IQR 2.5 mg, 5 mg).
ECG Monitoring:
Only 56% (n=18) of patients had a baseline ECG within 7 days prior to the initial IV haloperidol administration. Furthermore, 9% (n=3) received an initial dose of IV haloperidol despite having a baseline QTc ≥ 500 ms. For patients with an elevated baseline QTc (450-499 ms), 25% (n=8) received a follow-up ECG within 24 hours following IV haloperidol administration for QT prolongation monitoring. Follow-up ECGs resulted with a QTc interval ranging from 404-514 ms.
QT-prolonging conditions:
Of the 32 patients reviewed, 15 patients (47%) who received IV haloperidol had one or more comorbidities that may have predisposed them to QT prolongation. More than half of patients with predisposing conditions (n=8) such as delirium, dementia, heart failure, coronary artery disease, and acute myocardial infarction, received an ECG within 7 days prior to IV haloperidol administration and 5 of these patients had a baseline QTc > 450 ms.
QT-prolonging medications:
At least 27 patients (84%) received one additional medication associated with QT prolongation within 24 hours of IV haloperidol administration. All medication lists were reviewed in entirety for QT prolonging medications. The most commonly observed drugs associated with QT prolongation were levofloxacin, ondansetron, dexmedetomidine, famotidine, methadone, erythromycin, quetiapine, risperidone, and sertraline.6
Other risk factors:
Multiple studies referenced by the American Heart Association and the American College of Cardiology Foundations have shown the risk for potentially fatal arrhythmias among hospitalized patients is significantly greater in women than in men.7 Of the seven female patients that received IV haloperidol, a QTc > 450 ms was recorded for four of the five (80%) that received baseline ECG monitoring. Besides gender, potentially fatal arrhythmias are also more common in patients greater than 65 years of age. Baseline ECG monitoring was obtained for four out of six (67%) patients greater than 65 years old and all four patients had a QTc > 450 ms.
Discussion & Recommendations:
Based on this analysis of IV haloperidol administrations over a year, the incidence of this “off-label” practice is low at our institution. However, this provides an opportunity to improve patient safety. After reviewing a limited number of cases involving IV haloperidol, the following recommendations have been developed and implemented at Mount Sinai Hospital:
- Remove override function for haloperidol at the automated dispensing cabinet.
- Implement clinical decision support to ensure proper prescribing of haloperidol and provide guidance to the frequency and timing of ECG monitoring.
- Create an alert during order entry to ensure proper route is ordered.
- Consider alternative therapies for first line; haloperidol is not recommended for the treatment or prevention of delirium.
- Avoid IV haloperidol due to the increased risk of adverse cardiac events; intervene if IV haloperidol is being considered.
- Educate physicians, pharmacists, and nurses regarding the risk of QT prolongation associated with IV haloperidol.
- Monitor magnesium (<1.5 mg/dL) and potassium (<3.5 mEq/dL), as the risk for TdP is greater in patients with hypomagnesemia and hypokalemia.
- Perform a baseline ECG prior to haloperidol administration.
- Haloperidol should not be administered if the QTc exceeds 500 ms.
- If the initial QTc is elevated (450-499 ms), a follow-up ECG is recommended within 24 hours following administration of IV haloperidol.
- Assess risk if IV haloperidol is being administered.
References
- Information for Healthcare Professionals: Haloperidol (marketed as Haldol, Haldol Decanoate and Haldol Lactate). Information for Healthcare Professionals: Haloperidol (marketed as Haldol, Haldol Decanoate and Haldol Lactate) 2007. Available at: http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/drugsafetyinformationforheathcareprofessionals/ucm085203.htm. Accessed May 9, 2016.
- Society of Critical Care Medicine and American Society of Health-System Pharmacists. Sedation, analgesia, and neuromuscular blockade of the critically ill adult: revised clinical practice guidelines for 2002. Am J Health-Syst Pharm. 2002; 59:147-9.
- Tesar GE, Murray GB, Cassem NH. Use of high-dose intravenous haloperidol in the treatment of agitated cardiac patients. J Clin Psychopharmacol. 1985; 5(6):344-7.
- Wang W, Li HL, Wang DX. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial. Crit Care Med. 2011; 40:731–739.
- Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263-306.
- Risk Categories for Drugs that Prolong QT & induce Torsades de Pointes (TdP). CredibleMeds. Available at: https://www.crediblemeds.org/new-drug-list/. Accessed May 9, 2016.
- Drew BJ, Ackerman MJ, Funk M, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010; 121(8):1047-60.
Board of Pharmacy Update
Highlights from the November 2016 Meeting
by Kathryn Schultz, PharmD, BCPS, BCOP, Director of the Division of Government Affairs
The November 15th Board of Pharmacy Meeting was held at the James R. Thompson Center in downtown Chicago. These are the highlights of that meeting.
New Pharmacy Investigators – Two new pharmacy investigators (inspectors) were introduced at the Board Meeting. Both inspectors will work in the northern half of the State and will help increase the number and frequencies of inspections. Please make sure your self-inspections are up to date!
Department Updates – There is a new online pharmacy technician license application that includes students and certified pharmacy technician initial applications. The system incorporates a faster process than sending in forms via USPS. However, forms must be scanned and downloaded. The Department is planning on rolling out similar processes for pharmacies and pharmacists in the near future. Registrants will be able to go online and check license application status and update profiles including email addresses.
NABP/AACP District IV Meeting – The Illinois Board of Pharmacy and the University of Illinois at Chicago, College of Pharmacy co-hosted the three days of education and policy meetings on November 2-4. The District elected Illinois Board member Al Carter as their representative to the resolutions committee and Phil Burgess was re-elected to a three year term to the NABP Executive Committee. Three resolutions will be brought to the resolutions committee from District IV. They are: 1. NABP should review current language on telepharmacy and use the Illinois Pharmacy Practice Act as a potential model; 2. NABP should define the pharmacist-patient relationship; and 3. AACP requested that foreign pharmacy students who shadow US pharmacists should not have to abide by State licensure requirements but be provided with a separate mechanism for regulation.
Board Elections – Yash Patel was re-elected as Board Chair for the 2017 year, and Ned Milenkovich was re-elected as Vice Chair.
Examination Issues – There was continued discussion on NAPLEX and MPJE failures. The Illinois Pharmacy Practice Act requires remediation after 3 failures of any or all of either tests. The Board is investigating options provided by the Colleges of Pharmacy for approved coursework. Dr. Carrie Sincak, Assistant Dean at Midwestern University Chicago College of Pharmacy offered videotaped therapeutics lectures as an option. Midwestern also offers a 3-day exam review program that may be offered more than once a year. The program is currently open to all pharmacist candidates, not just Midwestern grads. The Board will continue to investigate solutions.
Legislative Update – Garth Reynolds, IPhA Executive Director provided a brief legislative update to the Board. The fall veto session is taking place the 2nd and 3rd weeks of November, and there may be some movement on a bill that could facilitate pharmacist provider status in Illinois. As a result of the election, the Democrats lost their supermajority in the House but retained it in the Senate only by one vote. Republicans will now have to play a role in any budget negotiations.
Practice Act Update Underway – The Department staff has begun work to update the Pharmacy Practice Act which will sunset in 2017. This will open all sections of the Act for possible changes.
Open Session – Clarification by the Board was requested regarding auto-verification of some classes of medications. The Department staff felt that a revision of the Practice Act is necessary but that conveniently, it will be open this coming year for those types of changes.
Next Meeting – The next meeting of the Board of Pharmacy will take place on Tuesday, January 10th at 10:30 AM in the James R. Thompson Center, 100 W. Randolph, Chicago. Members of the profession and public are welcome to attend.
Hi Tech
Introducing Clara Gary
by Clara Gary, CPhT, ICHP Technician Representative
Hi pharmacy technicians!
I am Clara Gary, your new Technician Representative on the ICHP Board! I met some of you at the ICHP 2016 Annual Meeting during the Saturday technician sessions. Wasn’t it wonderful?! We learned about patient safety issues and error prevention measures, how to survive a 340B and Joint Commission Audit and we were introduced to two technicians working with expanded roles as investigational drug and medication reconciliation technicians. And guess where these topics came from? They came from you! When your fellow pharmacy technicians completed their needs assessments and returned them to ICHP, the Educational Affairs and planning committee listened and gave us what we asked for.
I know all of you are some of the best and brightest in your respective pharmacies because you made the decision to come to this meeting and educate yourselves. You understand that our profession is expanding and growing and that we need to be involved in this process. According to Miriam Mobley-Smith’s article, Transforming Technicians: Insights Into the Expanding Roles of Pharmacy Technicians, she states that “a better qualified pharmacy technician workforce will improve patient safety, provide greater consistency to enable the expansion of the technician’s roles and responsibility, [and] give [pharmacists] greater confidence in the delegation of technicians’ tasks”.1 But for this to happen we need to continue to educate ourselves and work together in organizations that appreciate, respect and promote the pharmacy technician profession. In Illinois that organization is ICHP.
I encourage you all to get involved, but here is how I became a member of ICHP:
Our pharmacy student extern, Oksana Kucher, at the University of Illinois observed me at work and after watching me for several days she said, “I think that what you are doing with discharging patients is really interesting and you should present on transitions of care at the Annual ICHP meeting”. I was shocked because I had noticed her watching me but didn’t think much of it. LOL!
At first I was very nervous and apprehensive about speaking in public, but she explained that other technicians would be interested to learn about new roles technicians are fulfilling in the workplace. So I got over my fear, stepped up to the plate and gave a presentation at the ICHP 2014 Annual Meeting on the advanced roles for pharmacy technicians. Then using the awesome “Double Dose Program” (ICHP's Buy One Membership, Get One Free deal) a fellow technician friend and I JOINED ICHP together!
Think about it, ICHP exposes technicians to people that work in all areas of pharmacy. You just have to be willing to come out and network, then: LISTEN, LEARN and GROW. Look for an area within your pharmacy or the organization that you are passionate about and find yourself a mentor then PARTICIPATE. Since I joined ICHP, I have gotten to work with many great people but my time spent with the great teacher Dr. Nicholas Popovich has been especially rewarding. He listened to my suggestions, showed me respect and his humbleness continues to inspire me and the countless future pharmacists that he teaches until this day. This quote that I love is an example of how Dr. Popovich approaches things: “The greatest intention pales next to the smallest deed.” This has become my mantra, and now I try to become the change I wish for.
Pharmacy is not only about counting pills and filling medications. Of course those are the basics, but there are all kinds of OPPORTUNITIES available. There are technicians in research, investigational drugs, nuclear medicine, accredited sterile clean rooms, operating and emergency rooms, procurement, continuous quality improvement and medication assistance programs to name a few. The sky is the limit, so why should you limit yourself? To me, ICHP is a gem! It’s an organization that listens to the technician membership when we communicate our needs, our wants and our concerns. ICHP has several programs to address and promote our continued professional growth. Since joining ICHP, I am learning to move outside of my comfort zone and try things that I fear, like public speaking and now I am attempting to develop a blog! Go figure, I guess old dogs can learn new tricks!
Volunteer to be on a committee at ICHP, become an ICHP Champion (more on that here) and organize the technicians in your area for CE via conference call, an online group or come out to a CE dinner and networking session. Your membership also gives you access to the wonderful Pharmacy Tech Topics™ modules for home-study continuing pharmacy education credits! So invite a fellow technician and ATTEND the ICHP Spring and Annual meetings, like I did. Remember that the only way to improve your situation or make any meaningful change is to GET INVOLVED!
Now I would like to hear from you, email me at cgary1@uic.edu! Tell me: What do you want from ICHP? What questions and concerns do you have? How can I best serve you as the Board Technician Representative? What suggestions do you have for me?
Talk with you soon,
Clara
P.S. I want to thank Oksana, who is doing her residency at Princeton University Hospital, for encouraging me to get involved and I haven’t looked back since!
EDITOR'S NOTE: For more on Clara Gary, ICHP's new Tech Rep, check out her Leadership Profile in the December 2016 issue of KeePosted.
Reference
New Practitioners Network
Grooming Tips: SOAP for New Practitioners
by Sylvia Walsh, PharmD Candidate (2017), Rosalind Franklin University of Medicine and Science College of Pharmacy; Milena McLaughlin, PharmD, MSc, BCPS-AQ ID, AAHIVP, (Mentor) Assistant Professor/HIV/ID Clinical Pharmacist, Midwestern University/Northwestern Memorial Hospital
As a technician with a background in community pharmacy, I have interacted with several new pharmacists. To this day I remember a when a new pharmacy graduate, third day on the job, told me that she had no idea “pharmacy was going to be like this”. In the hope of bringing more transparency to the transition from student to practitioner, I have interviewed current pharmacy residents, residency trained pharmacists, and community pharmacists on what they wish they had known as a student. Hopefully these “SOAP” note tips of the most common themes from my interviews will be helpful for students and new practitioners.
Organization Membership Discounts
S/O: Several organizations offer students discounted or free registration for local or national meetings. By taking advantage of these opportunities at the student level, one can determine which organizations they would like to be involved with after graduation. Attending these meetings provides great networking opportunities not only for residency, but for future employment. At these meetings, several pharmacy organizations also provide workshops to students on residency, CV preparation, and interview skills.
A/P: Organizations for fourth year students and new practitioners include the American College of Clinical Pharmacy (ACCP), the American Pharmacists Association (APhA), the American Society of Health-System Pharmacists (ASHP), and the Illinois Council of Health-System Pharmacists (ICHP). ACCP offers CV tips and on-demand CV review. APhA has a new practitioner mentor program that will connect mentors based on the mentee's needs, a two year discounted membership bundle including a NAPLEX review book, and one year of liability insurance. The ASHP New Practitioners Forum provides practical career development tools, programs, and opportunities for growth that aid in the transition from student to pharmacist. ICHP provides CV review and a New Practitioners Network to help students transition into the real world of pharmacy. Attend as many local and national meetings as your schedule and resources allow to help focus your interests post-graduation.
ASHP Midyear
S/O: The ASHP Midyear can be overwhelming and hectic, so make sure to be prepared. ASHP and ACCP provide residency and fellowship directories that provide brief descriptions of the programs and direct links to the programs. The annual ASHP Midyear Clinical Meeting and Exhibition is intended for current fourth year pharmacy students. However, there will be some P1 - P3 pharmacy students who attend as well.
A/P: If you want to get the real scoop on a residency program, spend more time talking with the current residents. You will be surprised by their honesty and frankness about their program. Narrow your residency list prior to the meeting and research each program. Come with relevant and concise questions (the answers to which should not be readily found on the program’s website!). The ASHP Midyear is a great opportunity for networking. Network with everyone you meet. Introduce yourself as a current fourth year pharmacy student interested in the specific program. It is a good idea to have business cards and CVs available in case you are asked for these. Dress professionally and remember that this is your time to find out to which programs you want to apply!
Interviews
S/O: You are interviewing the program as much as they are interviewing you. The entire day is an interview, so it is crucial to always act professional and be polite to everyone. ACCP and ASHP have interview prep materials with questions available online. And always remember, pharmacy is a small world!
A/P: Practice interviewing with another person to deliver short and concise responses. Research the program beforehand and be knowledgeable about what types of rotations and opportunities that program offers. Be ready to answer questions regarding clinical scenarios and have a list of questions to ask of the program as well. Develop questions that are not easily found online to ask the interviewer. Once the interview is over send a thank you card or email.
The NAPLEX
S/O: The NAPLEX exam was recently changed from an adaptive format to a standardized exam. The amount of questions also increased from 185 to 200. This change increased the amount of time allotted for the exam from 4 hours and 15 minutes to 6 hours. Registration for the NAPLEX begins on November 1, 2016 for 2017 graduates. There are several types of NAPLEX prep materials available (e.g. online courses, textbooks, and mobile apps), so it is important to know your learning style. To begin studying in the month leading up to the exam is not sufficient preparation. Ideally, one should be studying throughout the four years of pharmacy school. To prepare for the NAPLEX it is important to have confidence. Pharmacy experience is helpful in preparation for the NAPLEX.
A/P: Regardless of the amount of pharmacy experience one has, it is still important to take the exam seriously. The NAPLEX is a long exam and test taking practice will help build stamina. It is also a good idea to scope out the test taking facility before the exam and make sure to give yourself adequate time to get there. Start studying early and create a study group with weekly review sessions. Make sure to familiarize yourself with the above mentioned changes prior to taking the exam.
Working as a New Practitioner
S/O: As a student, one cannot grasp the responsibility and the impact an error can have on patient care. Pharmacists have the ability to intervene in order to improve safety and patient outcomes.
A/P: The transition to pharmacy practitioner can be shocking at first. However, it is important to remember that you have the tools to be successful as a practicing pharmacist. In the end, the pharmacist is in charge and is the final quality assurance check. Pharmacy technicians are a great resource and are often well versed in the areas in which they work. Also, there are several resources available for new practitioners that offer guidance and advice. Wherever you end up, it is important to establish a support structure and remember your strengths.
ICHPeople
 Congratulations to Mary Ann Kliethermes for receiving the ASHP Board of Directors Distinguished Leadership award! Read the official press release from ASHP.
Congratulations to Mary Ann Kliethermes for receiving the ASHP Board of Directors Distinguished Leadership award! Read the official press release from ASHP.
Congratulations to SIUE student chapter president, Mallory Belcher, and the SIUE SSHP chapter for receiving the ASHP Outstanding Professional Development Project Award.
Congratulations to Farah Barada, Monica Lach, Bernice Man, Danielle Rahman and Elizabeth Schar for completing the ASHP Foundation Pharmacy Leadership Academy.
College Connections
Chicago State University College of Pharmacy
Pros vs. Cons of Working During Pharmacy School
by Dezaray McDonald, P3
As an eager and naïve pre-pharmacy student I placed importance on having a job prior to applying to pharmacy programs because I was under the impression that not having this experience would make me less competitive. I feared that not having experience as a technician would decrease my chances of getting accepted. If you are a student feeling pressured to land a technician position, my hope is that these pros and cons will help put things into perspective.
I want to begin by explaining the benefits of working during pharmacy school. Firstly, it allows you to work with pharmacists and make personal connections with them. Establishing positive relationships could potentially increase your probability of obtaining a good employment recommendation after graduation. This networking opportunity is invaluable and can be beneficial for other ventures such as participation in professional organizations. All students have heard the following phrase at least once, “pharmacy is a small world”; thus, positive networking is essential. Secondly, the on-the-job experience while still a student is a great way to gain insight into your expectations once you become a pharmacist. Thirdly, having exposure to the drugs as they are dispensed can certainly be useful as you learn about them in the classroom. Next, if you happen to work in the community pharmacy setting, whenever a patient approaches the consultation window, this represents an opportunity for you to apply counseling skills learned in school. This exposure will help better prepare you for APPEs and practice as a pharmacist. Lastly, having a part-time position in addition to school forces one into having better time management and organizational skills.
One major disadvantage of holding a job is of course the time spent away from studying. If you are not able to successfully balance your time both studying and working, then you will have to truthfully evaluate the need for having a job. Since everyone has different financial situations, the decision to work while in school has to be a personalized one. In the community pharmacy setting for instance, in certain districts they have minimum required hours per week, ranging from 8-15 hours per week. Based on my personal community pharmacy experience, I was required to work 12 hours per week. I decided working that many hours, in addition to school, and volunteering with organizations on campus was too much for me. Thus, I made the decision to end my employment. However, as stated, everyone is different; you have to do what is ultimately best for you!
When assessing the benefits and disadvantages of having a job while in school, think about what is best for your education. Your situation may change from year to year, depending on your course load.
Southern Illinois University Edwardsville School of Pharmacy
Residency, or No Residency -- That is the Question
by Jamal Sims, P3, Class / Student Representative Council President
One characteristic that I pride myself on having is being decisive when it comes to making tough choices. I have carried this trait with me throughout my life when it comes to work, school leadership positions. I made the decision to pursue a career in pharmacy when I was 16 years old and have not regretted that decision. After countless, long days filled with classes and many long nights filled with studying, I achieved my goal of being accepted into pharmacy school.
And then there’s now. As a third year pharmacy school student, I am in no way certain of what I want to do after graduating from pharmacy school. Do I want to pursue academia? Take on a position as a clinical pharmacist? Maybe even take on health administration? Although I am facing this tough decision, I noticed a trend in all of the options that I’ve considered; a residency will most likely be required.
A residency is postgraduate education that an individual has the option of pursuing after completing pharmacy school. One could complete a PGY1 (postgraduate year one) followed by a PGY2 (postgraduate year two) residency (if the individual desires to do so). Both involve an application and interview process that is followed up by a matching process through the American Society of Health-System Pharmacists.
It’s no secret that getting a residency is no easy feat. Therefore I have given myself three goals to achieve before the beginning of my fourth and last year of pharmacy school.
1. Attend a Residency Happy Hour.
My SSHP chapter provides us with an innovative method of preparing for the residency process utilizing what we call “Residency Happy Hours”. During this time, faculty walk us through the entire process starting with advice on preparing for Midyear Clinical Meeting (MCM) all the way through how to be successful in the second match process. We also have the opportunity to attend a residency panel discussion held by the chapter to ask any questions we may have regarding their experiences before, during and after being a pharmacy resident.
2. Attend the ASHP MCM in December.
I’ve heard countless stories from older students about their ASHP MCM experience. Considering the importance of this conference with regard to getting placed in a residency, I want to make sure that I am fully prepared for when my time comes. I believe by attending Midyear as a third year student, I will be able to ask questions and become familiar with the entire process as a whole. This will also serve as great practice for talking to programs and planning my time effectively during the conference to talk to as many programs as possible. Overall, I feel that I will be more confident in my ability to take on this conference with full force my fourth year.
3. Be Active!
I have gotten so much more out of an organization when I am highly involved. This year I will be serving as the vice president of my school’s SSHP chapter and I am beyond excited. I have begun to plan blanket drives for dialysis clinics in our area and for the chapter to attend pharmacy legislative day at our state capital. I have the honor of working with an awesome executive board and I am optimistic we will accomplish many, if not all of our goals. This school year, I plan on being even more active in helping out each organization that I’m a part of to the best of my ability. I want to be assured that when I have an interview, whether it be for a residency or a pharmacist position, that I can speak with confidence regarding my participation in organizations and how it has shaped me into the leader I am today.
This journey of becoming a pharmacist has definitely been interesting. I have never worked for something that has been this difficult and trying at times, yet I legitimately still enjoy it. Although I may not know exactly what I want to do as a pharmacist, I do know that I am ready to take on this journey of pursuing a residency with full force.
University of Illinois at Chicago College of Pharmacy
Morning Rounds: Student Learning Opportunities over Coffee and Cases
by Kelsey VandenBerg, P2, Health-Systems Chair
At the University of Illinois at Chicago College of Pharmacy, we are strategically positioned in the heart of the Illinois Medical District and have the distinct opportunity of learning from top rated pharmacists who are just next door at the University of Illinois Hospital. Our professors frequently mention rounding on patients with a team of healthcare providers. This intrigues many students, yet we often do not get the chance to experience this until our fourth year rotations. Recognizing this opportunity for additional student learning, UIC’s student ICHP chapter, in collaboration with the college’s student chapter of ACCP, created Morning Rounds: Cases and Therapeutics, warmly deemed MRCaT.
The brainchild of practicing clinical pharmacists and successful student leaders, MRCaT was developed to be a stress-free learning environment for pharmacy students at all stages of training. The voluntary meetings take place every other Wednesday morning, and prior to the event, attendees receive a patient case with corresponding treatment guidelines for the relevant disease states. Students are also provided with a “P1 cheat sheet” that is tailored to the specific case to help less experienced students with acronyms, normal lab values, and medical jargon used. Sessions begin with a third year pharmacy student introducing the case, allowing these students the opportunity to try their hand at presenting a patient in a setting modeled after grand rounds. The clinical pharmacist in attendance is free to interject his or her thoughts at any point, which may include comments on the format and clarity of the SOAP note or posing directed questions to drive home a principle.
The pharmacist leads the discussion once the patient is presented, guiding the attendees through their evidence-based approach to the case and development of a pharmacotherapeutic plan. During this process, the patient’s pertinent lab values and medical history are discussed, and relevant disease state information is reviewed. The proposed assessment and plan are subsequently evaluated. Students in attendance have the opportunity to learn how the pharmacist would proceed with the case in a patient-centered manner and are exposed to “clinical pearls” shared by the skilled clinicians. Despite the early morning meeting time, case discussions are often lively and peppered with questions and answers from students – with the help of the provided coffee, of course.
Student learning occurs on a myriad of levels during the Morning Rounds sessions. While attendees get the chance to assimilate information learned from multiple courses and apply it to a specific patient, they are also learning how to do so in a simulated grand rounds setting. This is a valuable skill to possess as a future pharmacist. All patient cases discussed in the MRCaT sessions are real, de-identified SOAP notes written by fourth year pharmacy students during their APPE rotations, giving the attendees a small taste of the kinds of patient cases they may encounter in practice. Exposure to these patient cases provides another outlet for students to familiarize themselves with clinical documentation. The meetings also allow attendees to practice applying information from their courses, which encourages students to draw on concepts learned throughout the curriculum. Students are also able to learn how patient cases are presented and gain insight into how experienced clinical pharmacists dissect these cases. This is all accomplished in a relaxed setting free from the looming stresses of grades, making for a comfortable environment conducive to student learning through active participation.
Thus far, we have had the opportunity to host pharmacists from a diverse range of practice settings and specialties, including clinicians who practice in general medicine to those who are board certified specialists in specific fields. The semester was kicked off with a case involving community-acquired pneumonia, heart failure, and hypertension. We then moved on to more specialized areas of practice, discussing cases in HIV and Hepatitis C. In addition, students were introduced to telemedicine by pharmacists who practice in this unique setting. Subsequent cases focused on solid-organ transplants and widespread chronic disease states, including diabetes and atherosclerotic cardiovascular disease.
UIC’s ICHP student chapter is dedicated to contributing to the organization’s mission to advance excellence in pharmacy, and we strive to achieve to do this by providing excellent opportunities for our fellow students, such as MRCaT. We are grateful to all who participated this fall, and look forward to another great semester of coffee and cases!
More
Welcome New Members!

| New Member |
Recruiter |
| Munsal Bashid |
|
| Alyse Battles |
|
| Jeffrey Bell |
|
| Zach Click |
|
| Kevin Cross |
|
| Danielle Davis |
|
| Devin Dinora |
|
| Kelsey Elmore |
|
| Katelyn Fryman |
|
| Noah Harris |
|
| Jacob Huez |
|
| Taylor Kirby |
|
| Jessica Kirk |
Angelia Dreher |
| Greta Kravetskiy |
|
| Deidre Ledbetter |
|
| Kayla Link |
|
| Blake Lutzow |
|
| Kyleigh Maday |
|
| Michael McGee |
|
| Josha Patel |
|
| Dana Rod |
|
| Adam Schulte |
|
| Scott Sexton |
|
| Dylan Smith |
|
| Pavis Smith |
|
| Michael Sparkman |
|
| Rolandes Urbstunaitis |
|
| Madeline Vanbaele |
|
| Leslie Wheeler |
|
| Kimberly Zaleski |
Katarzyna Plis |
Officers and Board of Directors
CHARLENE HOPE
MIKE WEAVER
Treasurer 815-599-6113 mweaver@fhn.org
LARA ELLINGER Director, Educational Affairs laelling@nm.org
CARRIE VOGLER
Director, Marketing Affairs
217-545-5394
KRISTI STICE
Director, Professional Affairs
CAROL HEUNISCH Director, Organizational Affairs 847-933-6811
KATHRYN SCHULTZ
Director, Government Affairs
312-926-6961
Chairman, Committee on Technology 816-885-4649 david.tjhio@bd.com
COLLEEN BOHNENKAMP
Chairman, New Practitioners Network
BRYAN MCCARTHY
Co-Chairman, Ambulatory Care Network
VIRGINIA NASH
Co-Chairman, Ambulatory Care Network
CLARA GARY
Technician Representative
JACOB GETTIG
Editor & Chairman, KeePosted Committee
630-515-7324 fax: 630-515-6958
jgetti@midwestern.edu
Regional Directors
NOELLE CHAPMAN
Regional Director North
312-926-2547
nchapman@nmh.org
LYNN FROMM
Regional Co-Director South
618-391-5539
TARA VICKERY GORDEN
Regional Co-Director South
618-643-2361 x2330
Student Chapter Presidents
FLORENCE PATINO
President, Student Chapter
Chicago State University C.O.P.
SHAZIYA BARKAT
President, Student Chapter
KASIA PLIS
President, Student Chapter
Roosevelt University C.O.P.
MALLORY BELCHER President, Student Chapter Southern Illinois University Edwardsville S.O.Pmabelch@siue.edu
LEVI PILONES President, Chicago Student ChapterUniversity of IL C.O.P. lpilon2@uic.edu
TREVOR LUMAN President, Rockford Student Chapter University of IL C.O.P. tluman2@uic.edu
ICHP Affiliates
ANTOINE JENKINS
President, Northern IL Society (NISHP)
JARED SHELEY
President, Metro East Society (MESHP)
ICHP Pharmacy Action Fund (PAC) Contributors
Names below reflect donations between December 1, 2015 and December 1, 2016. Giving categories reflect each person's cumulative donations since inception.
ADVOCACY ALLIANCE - $2500-$10000Kevin Colgan
Edward Donnelly
James Owen Consulting, Inc.
Frank Kokaisl
Scott Meyers
Michael Novario
Michael Weaver
Thomas Westerkamp
LINCOLN LEAGUE - $1000-$2499
Scott Bergman
Andrew Donnelly
Ginger Ertel
Ann Jankiewicz
Jan Keresztes
Kathy Komperda
William McEvoy
Christina Quillian
Michael Rajski
Michael Short
Carrie Sincak
Avery Spunt
Patricia Wegner
CAPITOL CLUB - $500-$999
Margaret Allen
Sheila Allen
Rauf Dalal
Drury Lane Theatre
Kenneth Foerster
Travis Hunerdosse
Leonard Kosiba
Mary Lee
Janette Mark
Jennifer Phillips
Edward Rainville
Kathryn Schultz
Heidi Sunday
Jill Warszalek
Alan Weinstein
GENERAL ASSEMBLY GUILD - $250-$499
Tom Allen
Jennifer Arnoldi
Peggy Bickham
Jaime Borkowski
Donna Clay
Scott Drabant
Sandra Durley
Michael Fotis
Jo Ann Haley
Joan Hardman
Kim Janicek
Zahra Khudeira
Ann Kuchta
Ronald Miller
Peggy Reed
Tara Vickery Gorden
Carrie Vogler
Marie Williams
SPRINGFIELD SOCIETY - $100-$249
Rebecca Castner
Noelle Chapman
Lara Ellinger
Jennifer Ellison
Nora Flint
Carol Heunisch
Lois Honan
Charlene Hope
Robert Hoy
Kati Kwasiborski
Bella Maningat
Milena McLaughlin
Megan Metzke
Katherine Miller
Kenneth Miller
Danielle Rahman
Jerry Storm
Amanda Wolff
GRASSROOTS GANG - $50-$99
Katrina Althaus
Antoinette Cintron
Jeanne Durley
Linda Grider
Heather Harper
Megan Hartranft
Erika Hellenbart
Ina Henderson
Christina Jacob
Leslie Junkins
Connie Larson
Barbara Limburg-Mancini
Brian Matthews
John McBride
Bill Middleton
Mark Moffett
Kit Moy
Gary Peksa
Daphne Smith-Marsh
Jennifer Splawski
Nadia Tancredi
Thomas Yu
CONTRIBUTOR - $1-$49
Marc Abel
Tamkeen Abreu
Trisha Blassage
Colleen Bohnenkamp
Erick Borkowski
Jeremy Capulong
Josh DeMott
Janina Dionnio
Angelia Dreher
Tim Dunphy
Veronica Flores
Frank Hughes
Lori Huske
Vera Kalin
Levi Karell Pilones
Josie Klink
David Martin
Claudia Muldoon
Jose Ortiz
Lupe Paulino
Amanda Penland
Zach Rosenfeldt
Kevin Rynn
Cheryl Scantlen
Joellyn Schefke
Amanda Seddon
Kushal Shah
Sarah Sheley
Beth Shields
David Silva
Helen Sweiss
Steve Tancredi
Kathryn Wdowiarz
Marcella Wheatley
Tom Wheeler
Junyu (Matt) Zhang
Upcoming Events
Tuesday, December 13, 2016
Accredited for pharmacists and pharmacy technicians | 1.0 contact hour (0.1 CEU)
Tuesday, January 10, 2017
Tuesday, January 10, 2017
Sangamiss LIVE Program
Engrained Brewing Company | Springfield, IL
Accredited for pharmacists and pharmacy technicians | 1.0 contact hour (0.1 CEU)
Wednesday, January 11, 2017
Accredited for pharmacists | 0.5 contact hour (0.05 CEU)
Thursday, January 12, 2017
Students as Pharmacist Extenders
NISHP LIVE Program
UIC College of Pharmacy | Chicago, IL
Save the date! Watch the ICHP Calendar and CPE News Briefs for more information.
Wednesday, February 15, 2017
NISHP Double Feature
NISHP LIVE Program
Location TBA | Oakbrook Terrace, IL
Save the date! Watch the ICHP Calendar and CPE News Briefs for more information.
Friday, March 31, 2017 - Saturday, April 1, 2017
LIVE Joint Statewide Meeting with Missouri Society of Health-System Pharmacists

Print Entire Issue


 President's Message
President's Message Directly Speaking
Directly Speaking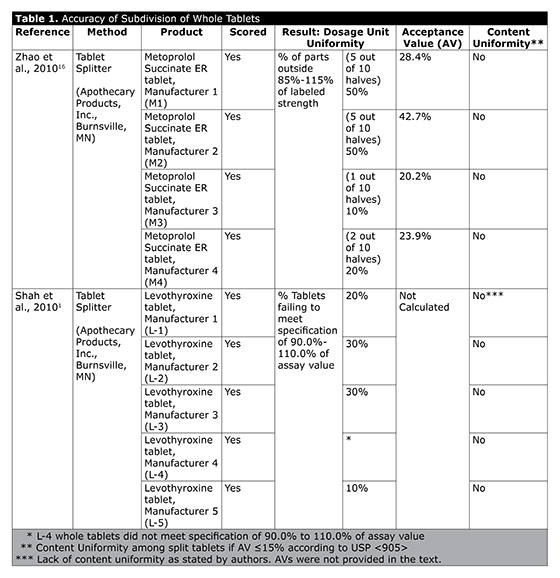
 Where did you grow up and go to school?
Where did you grow up and go to school?  Congratulations to Mary Ann Kliethermes for receiving the ASHP Board of Directors Distinguished Leadership award! Read the official press release from ASHP.
Congratulations to Mary Ann Kliethermes for receiving the ASHP Board of Directors Distinguished Leadership award! Read the official press release from ASHP.


