Official Newsjournal of the Illinois Council of Health-System Pharmacists

November 2021
Volume 47 Issue 4
Feature
Call for Entries: 2016 Best Practice Award
Columns
College Connections
Midwestern University Chicago College of Pharmacy
Roosevelt University College of Pharmacy
More
Officers and Board of Directors
ICHP Pharmacy Action Fund (PAC) Contributors
KeePosted Info

Loves Park, IL 61111-8653
Phone: (815) 227-9292
Fax: (815) 227-9294
www.ichpnet.org
KeePosted
Official Newsjournal of the Illinois Council of Health-System Pharmacists
EDITOR
Jacob Gettig
ASSISTANT EDITOR
Jennifer Phillips
MANAGING EDITOR
Scott Meyers
ASSISTANT MANAGING EDITOR
Trish Wegner
DESIGN EDITOR
Amanda Wolff
EXECUTIVE VICE PRESIDENT
Scott Meyers
VICE PRESIDENT - PROFESSIONAL SERVICES
Trish Wegner
DIRECTOR OF OPERATIONS
Maggie Allen
INFORMATION SPECIALIST
Heidi Sunday
CUSTOMER SERVICE AND
PHARMACY TECH TOPICS™ SPECIALIST
Jo Ann Haley
ACCOUNTANTS
Jan Mark and Trisha Blassage
COMMUNICATIONS MANAGER
Amanda Wolff
ICHP Mission Statement
Advancing Excellence in Pharmacy
ICHP Vision Statement
ICHP dedicates itself to achieving a vision of pharmacy practice where:
- Pharmacists are universally recognized as health care professionals and essential providers of health care services.
- Patients are aware of the training, skills, and abilities of a pharmacist and the fundamental role that pharmacists play in optimizing medication therapy.
- Formally educated, appropriately trained, and PTCB certified pharmacy technicians manage the medication distribution process with appropriate pharmacist oversight.
- Pharmacists improve patient care and medication safety through the development of effective public policies by interacting and collaborating with patients, other health care professionals and their respective professional societies, government agencies, employers and other concerned parties.
- Evidence-based practices are used to achieve safe and effective medication therapies.
- There are an adequate number of qualified pharmacy leaders within the pharmacy profession.
- Pharmacists take primary responsibility for educating pharmacy technicians, pharmacy students, pharmacist peers, other health professionals, and patients about appropriate medication use.
KeePosted Vision
As an integral publication of the Illinois Council of Health-System Pharmacists, the KeePosted newsjournal will reflect its mission and goals. In conjunction with those goals, KeePosted will provide timely information that meets the changing professional and personal needs of Illinois pharmacists and technicians, and maintain high publication standards.
KeePosted is an official publication of, and is copyrighted by, the Illinois Council of Health-System Pharmacists (ICHP). KeePosted is published 10 times a year. ICHP members received KeePosted as a member benefit. All articles published herein represent the opinions of the authors and do not reflect the policy of the ICHP or the authors’ institutions unless specified. Advertising inquiries can be directed to ICHP office at the address listed above. Image disclaimer: The image used in the Pharmacy Tech Topics™ advertisement is the property of © 2016 Thinkstock, a division of Getty Images.
Copyright © 2016, Illinois Council of Health-System Pharmacists. All rights reserved.
Feature
Call for Entries: 2016 Best Practice Award

The objective of the Best Practice Award program is to encourage the development of innovative or creative pharmacy practice programs or innovative approaches to existing pharmacy practice challenges in health systems within the state of Illinois. Applicants will be judged on their descriptions of programs and practices employed in their health system based on the following criteria:
2015 Kuntal Patel, Pharm.D., Pavel Prusakov, and Heather Vaule “Osteopenia of Prematurity (aka Better Bones for Babies)” 2014 Arti Phatak, Pharm.D.; Brooke Ward, Pharm.D., BCPS; Rachael Prusi, Pharm.D.; Elizabeth Vetter, Pharm.D.; Michael Postelnick, BS Pharm, BCPS (AQ Infectious Diseases); and Noelle Chapman, Pharm.D., BCPS “Impact of Pharmacist Involvement in the Transitional Care of High-Risk Patients through Medication Reconciliation, Medication Education, and Post-Discharge Callbacks” 2013 “Development of a Urinary-Specific Antibiogram for Gram Negative Isolates: Impact of Patient Risk Factors on Susceptibility” 2012 |
Online entry form: http://ichpnet.org/pharmacy_practice/professional_practice/ Eligibility Instructions for preparing manuscript The manuscript should be organized as a descriptive report using the following headings:
Format All applicants will be notified of their status within three weeks of the submission deadline. Should your program be chosen as the winner:
Non-winning submissions may also be considered for publication in the ICHP KeePosted, but your permission will be obtained beforehand. Thank you to PharMEDium for providing a grant for the 2016 Best Practice Award! |
Columns
 President's Message
President's Message
Strengthen Your Chances of Success with Soft Skills
by Jen Phillips, PharmD, BCPS, ICHP President; co-written with Sheron Chen, PharmD, Assistant Professor of Clinical Sciences, Roosevelt University College of Pharmacy
 Directly Speaking
Directly Speaking
Letters I Hate and Love to Sign!
by Scott A. Meyers, Executive Vice President
Leadership Profile
Barb Limburg-Mancini, BS Pharm, PharmD
 What is your current leadership position for ICHP?
What is your current leadership position for ICHP?
Board of Pharmacy Update
Highlights from the March 2016 Meeting
by Scott A. Meyers, Executive Vice President
1 minor violation during the same visit $100 fine 2 minor violations during the same visit $250 fine 3 minor violations during the same visit $500 fine
Below is a reference list of potential pharmacy violations cited on the ticket:
- All required current licenses are posted in a conspicuous location in the pharmacy (pocket license or photocopy may be used when registrants are employed at multiple sites).
- Registrant wear proper clean attire and have proper name tags and designations.
- The schedule during which the pharmacy services are provided is conspicuously displayed.
- Security provisions are provided for all drugs and devices within the pharmacy when pharmacist is on staff and during the absence of a pharmacist.
- Refrigerators for the exclusive use of medications are clean, defrosted and in working order maintaining proper temperature.
- Pharmacy is clean and sanitary including but not limited to shelves, workflow area, sink and compounding area.
- Pharmacy must have a sink with hot and cold running water.
- Food and/or beverages are kept in designated areas away from dispensing activities and stored in refrigerators not used for medications.
- Expired medications are stored separately from active medication stock.
- All CII controlled substances are stored securely within the pharmacy.
- Every prescription dispensed shall be documented with the name, initials or other unique identifiers of the pharmacist and pharmacy technician if one is used.
- An offer to counsel shall be made on all prescriptions (new and refill prescriptions).
- Controlled drug prescriptions and records must be properly filed and maintained.
- Annual inventory of controlled substances are properly recorded, dated and signed.
- Controlled substance purchase invoices are signed and kept in a separate file.
- DEA 222 Form properly documented.
- Any prepackaged drug must have a label affixed-name and strength of the drug, name of the manufacturer or distributor, beyond use date, lot number on each container.
- Every licensed pharmacy shall conduct an annual self-inspection using forms provided by the Department.
Government Affairs Report
The Fun Has Begun
by Jim Owen and Scott A. Meyers
SB2515 PBM RegulationHR0944 Study e-prescribing discontinuation/stop ordersHR1018 Urge Congress to ban Direct-to-Consumer AdvertisingHB3627 Immunization expansion for pharmacistsHB5540 Dispensing naloxone without a prescriptionHB5591 PBM RegulationHB5809 Pharmacist prescribed hormonal contraceptives
These bills could be problems for pharmacy:
SB2498 Technical change to pharmacy practice actSB3336 Establishes a pharmacy quality assurance program for error reportingHB4936 Technical change to pharmacy practice actHB6180 Establishes a pharmacy quality assurance program for error reporting
| Bill No. | Sponsor | Summary | Status | Position |
| SB2177 | Noland, D-Elgin | Creates the Illinois Universal Health Care Act. Provides that all individuals residing in the State are covered under the Illinois Health Services Program for health insurance. Sets forth the health coverage benefits that participants are entitled to under the Program. Sets forth the qualification requirements for participating health providers. Sets forth standards for provider reimbursement. Provides that it is unlawful for private health insurers to sell health insurance coverage that duplicates the coverage of the Program. Provides that investor-ownership of health delivery facilities is unlawful. Provides that the State shall establish the Illinois Health Services Trust to provide financing for the Program. Sets forth the requirements for claims billing under the Program. Provides that the Program shall include funding for long-term care services and mental health services. Provides that the Program shall establish a single prescription drug formulary and list of approved durable medical goods and supplies. Creates the Pharmaceutical and Durable Medical Goods Committee to negotiate the prices of pharmaceuticals and durable medical goods with suppliers or manufacturers on an open bid competitive basis. Sets forth provisions concerning patients' rights. Provides that the employees of the Program shall be compensated in accordance with the current pay scale for State employees and as deemed professionally appropriate by the General Assembly. | Executive Comm. | Neutral |
| SB2269 | Bennett, D-Champaign | Makes appropriations to Colleges of Pharmacy at UIC, CSU and SIUe from the General Professions Disciplinary Fund. | Assignments Comm. | Neutral |
| SB2349 | Righter, R-Mattoon | Makes appropriations to Colleges of Pharmacy at UIC, CSU and SIUe from the General Professions Disciplinary Fund. | Assignments Comm. | Neutral |
| SB2403 | Rose, R-Champaign | Hospitals shall ensure that professional staff with direct and indirect patient care responsibilities including pharmacy staff, are periodically trained to implement sepsis protocols. | Public Health Comm | Neutral |
| SB2408 | Rose, R-Champaign | Makes appropriations to Colleges of Pharmacy at UIC, CSU and SIUe from the General Professions Disciplinary Fund. | Assignments Comm. | Neutral |
| SB2461 Same as HB4970 |
Barickman, R-Bloomington | Amends the Pharmacy Practice Act. Removes provisions concerning the position of deputy pharmacy coordinator. Removes limitations on the number of pharmacy investigators that must be employed by the Department of Financial and Professional Regulation (previously no less than 4 pharmacy investigators needed to be employed by the Department). Amends the Private Detective, Private Alarm, Private Security, Fingerprint Vendor, and Locksmith Act of 2004. Provides that the requirement for licensure that an applicant must submit certification issued by the Department of State Police that the applicant's fingerprinting equipment and software meets all specifications required by the Department of State Police applies to fingerprint vendor agencies (rather than fingerprint vendors), and that the requirement is a continuing requirement for licensure. Effective immediately. | Licensed Activities and Pension Comm. | Neutral |
| SB2498 | Bush, D-Grayslake | Amends the Pharmacy Practice Act. Makes a technical change in a Section concerning licensure without examination. | Assignments Comm. | Neutral |
| SB2515 Same as HB5591 |
Munoz, D-Chicago | Amends the Illinois Insurance Code. Provides a process to register with the Department of Insurance as a pharmacy benefits manager and what information must be included. Provides that the Director of Insurance may revoke, suspend, deny, or restrict a certificate of registration for violation of the Code or on other grounds as determined necessary or appropriate by the Director. Provides that the Department shall regulate the drug pricing process used by pharmacy benefits managers, and specifies the appeals process for such pricing. Provides that pharmacy benefits managers shall not mandate that a covered individual use a specific pharmacy or provide incentives to encourage the use of a specific pharmacy under specified circumstances. Provides criteria for entities to use in performing on-site audits of pharmacy records. Provides that health plans must permit their enrollees to receive benefits, which may include a 90-day supply of covered prescription drugs, at any of its network community pharmacies. Contains provisions concerning medication synchronization. Provides that dispensing fees shall be determined exclusively on the total number of prescriptions dispensed. Regulates how pharmacy benefits managers may utilize personally identifiable data. Provides that the Department can regulate other specified activities of pharmacy benefits managers. Makes other changes. Effective January 1, 2017. | Insurance Comm. | Support |
| SB2901 Same as HB5949 |
Martinez, D-Chicago | Amends the Pharmacy Practice Act. Extends the repeal of the medicine locking closure package pilot program from January 1, 2017 to January 1, 2018. Effective immediately. | Assignments Comm. | Neutral |
| SB3158 | McCann, R-Jacksonville | Amends the Home Health and Hospice Drug Dispensation and Administration Act. Provides that the Department of Public Health may by rule provide for the possession and transportation of greater quantities of specified drugs by a home health agency, hospice, or authorized nursing employee. | Assignments Comm. | Neutral |
| SB3326 | Luechtefeld, R-Okawville | Amends the Personnel Code to provide for partial jurisdiction B exemption for certain positions within the Department of Human Services. | Assignments Comm. | Neutral |
| SB3336 Same as HB6180 |
Righter, R-Mattoon | Amends the Pharmacy Practice Act. Requires pharmacies to establish and maintain a quality assurance program designed to prevent dispensing errors as well as a process designed to detect and identify dispensing errors. Requires pharmacies to commence an investigation into any detected dispensing errors within 2 days after the date the dispensing error is discovered. Requires that if an investigation into a dispensing error indicates that the dispensing error is attributable, in whole or in part, to the pharmacy or its personnel, that a quality assurance review be performed. Provides requirements for the quality assurance review and its records. Provides that the records of the quality assurance review shall not be subject to discovery in any arbitration, civil, or other proceeding, except in certain circumstances. Effective 12 months after becoming law. | Assignments Comm. | Oppose |
| HR0944 | Zalewski, D-Riverside | Urges the Department of Financial and Professional Regulation to undertake a study to determine the appropriateness of mandating a mechanism for electronically-prescribed prescription orders to electronically transmit "discontinuation", "cancel", or "stop" orders from health care providers to pharmacies and to examine the effects of auto-refill programs on the unnecessary filling of discontinued medications no longer endorsed by the prescriber. | Health Care Licenses Comm. | Support |
| HR1018 | Mitchell, R-Decatur | Urges Congress to adopt legislation banning direct-to-consumer advertising of prescription drugs. Urges the United States Food and Drug Administration to adopt appropriate rules and regulations banning direct-to-consumer advertising of prescription drugs. | Rules Comm. | Support |
| HB3627 | Evans, D-Chicago | Amends the Pharmacy Practice Act. Makes changes to the definition of "practice of pharmacy", including (ii) allowing for the vaccination of patients ages 10 through 13 pursuant to a valid prescription or standing order (was, limited to Influenza (inactivated influenza vaccine and live attenuated influenza intranasal vaccine) and Tdap (defined as tetanus, diphtheria, acellular pertussis) vaccines). Effective January 1, 2016. | Rules Comm. | Support |
| HB4408 | G. Harris, D-Chicago | Amends the Illinois Public Aid Code. Makes a technical change in a Section regarding Medicaid co-payments. | Rules Comm. | Neutral |
| HB4429 | Nekritz, D-Buffalo Grove | Amends the State Prompt Payment Act. Provides that after the effective date of the amendatory Act, any bill approved for payment under the Act and pursuant to a health benefit plan under the State Employees Group Insurance Act of 1971 or submitted under Article V of the Illinois Public Aid Code, except a bill for pharmacy or nursing facility services or goods, if payment is not issued to the payee in a timely manner under the Section, the following interest penalty shall apply to any amount approved and unpaid until final payment is made: the sum of the prime commercial rate plus 4.0% per year, applied pro rata for the amount of time the bill remains unpaid. Defines "prime commercial rate". Amends the Illinois Insurance Code. In provisions concerning timely payment for health care services, provides that the interest to be charged on late payments of periodic payments, payments by independent practice associations and physician-hospital organizations, and payments by health insurers, health maintenance organizations, managed care plans, health care plans, preferred provider organizations, and third party administrators shall be the sum of the prime commercial rate plus 4.0% per year. Defines "prime commercial rate". Amends the State Employees Group Insurance Act of 1971. Provides that the program of health benefits offered under the Act is subject to certain provisions of the Illinois Insurance Code concerning late payments and assignability except as otherwise provided. | Finance Subcomm. Of Revenue and Finance Comm. | Neutral |
| HB4539 | Brady, R-Normal | Makes appropriations to Colleges of Pharmacy at UIC, CSU and SIUe from the General Professions Disciplinary Fund. | Rules Comm. | Neutral |
| HB4554 | Flowers, D-Chicago | Amends the Illinois Insurance Code. Provides that individual or group policies of accident and health insurance amended, delivered, issued, or renewed in this State after the effective date of the amendatory Act shall provide coverage for all drugs that are approved for marketing by the federal Food and Drug Administration and that are recommended by the federal Public Health Service or the United States Centers for Disease Control and Prevention for pre-exposure prophylaxis and related pre-exposure prophylaxis services, including, but not limited to, HIV and sexually transmitted infection screening, treatment for sexually transmitted infections, medical monitoring, assorted labs, and counseling to reduce the likelihood of HIV infection among individuals who are not infected with HIV but who are at high risk of HIV infection. Provides that the provision does not require a policy of accident and health insurance to provide coverage for clinical trials relating to any drug for pre-exposure prophylaxis for HIV. Amends the Illinois Public Aid Code. Provides that upon federal approval, the Department of Healthcare and Family Services shall provide similar coverage. Effective January 1, 2017. | Insurance Comm. | Neutral |
| HB4936 | Durkin, R- | Amends the Pharmacy Practice Act. Makes a technical change in a Section concerning licensure without examination. | Executive Comm. | Neutral |
| HB4957 | Tryon, R-Crystal Lake | Amends the Medical Assistance Article of the Illinois Public Aid Code. Requires the Department of Healthcare and Family Services to provide medical assistance coverage for diabetes education provided by a certified diabetes education provider for children with Type 1 diabetes who are under the age of 18. Defines "certified diabetes education provider" to mean a professional who has undergone training and certification under conditions approved by the American Association of Diabetes Educators or a successor association of professionals. Defines "Type 1 diabetes" to have the same meaning ascribed to it by the American Diabetes Association or any successor association. Effective immediately. | Rules Comm. | Support |
| HB4970 Same as SB2461 |
Stewart, R-Freeport | Amends the Pharmacy Practice Act. Removes provisions concerning the position of deputy pharmacy coordinator. Removes limitations on the number of pharmacy investigators that must be employed by the Department of Financial and Professional Regulation (previously no less than 4 pharmacy investigators needed to be employed by the Department). Amends the Private Detective, Private Alarm, Private Security, Fingerprint Vendor, and Locksmith Act of 2004. Provides that the requirement for licensure that an applicant must submit certification issued by the Department of State Police that the applicant's fingerprinting equipment and software meets all specifications required by the Department of State Police applies to fingerprint vendor agencies (rather than fingerprint vendors), and that the requirement is a continuing requirement for licensure. Effective immediately. | Rules Comm. | Neutral |
| HB4981 | D. Harris, R-Mt. Prospect | Amends the State Prompt Payment Act. Provides that, for bills paid on or after the effective date, the interest penalty shall be 0.75% per month (currently, 1% per month). Effective immediately. | Rules Comm. | Oppose |
| HB5534 | Feigenholtz, D-Chicago | Amends the Compassionate Use of Medical Cannabis Pilot Program Act. Makes changes to the definition of "designated caregiver". Allows pharmacists to oversee through MTM the use of medical cannabis. Effective immediately. | Rules Comm. | Neutral |
| HB5540 | Flynn-Currie, D-Chicago | Creates Section 225 ILCS 85/19.1 Naloxone dispensing without a prescription. Consistent with the Heroin Crisis Act of 2015. | Rules Comm. | Neutral |
| HB5591 Same as SB2515 |
Lang, D-Chicago | Amends the Illinois Insurance Code. Provides a process to register with the Department of Insurance as a pharmacy benefits manager and what information must be included. Provides that the Director of Insurance may revoke, suspend, deny, or restrict a certificate of registration for violation of the Code or on other grounds as determined necessary or appropriate by the Director. Provides that the Department shall regulate the drug pricing process used by pharmacy benefits managers, and specifies the appeals process for such pricing. Provides that pharmacy benefits managers shall not mandate that a covered individual use a specific pharmacy or provide incentives to encourage the use of a specific pharmacy under specified circumstances. Provides criteria for entities to use in performing on-site audits of pharmacy records. Provides that health plans must permit their enrollees to receive benefits, which may include a 90-day supply of covered prescription drugs, at any of its network community pharmacies. Contains provisions concerning medication synchronization. Provides that dispensing fees shall be determined exclusively on the total number of prescriptions dispensed. Regulates how pharmacy benefits managers may utilize personally identifiable data. Provides that the Department can regulate other specified activities of pharmacy benefits managers. Makes other changes. Effective January 1, 2017. | Insurance Comm. | Support |
| HB5641 | Bellock, R-Westmont | Amends the Illinois Public Aid Code. In a provision concerning orthotic and prosthetic devices and durable medical equipment, provides that the Department of Healthcare and Family Services shall adjust the useful life expectancy of eligible orthotic and prosthetic devices and durable medical equipment to 5 years. Requires the Department to require by rule all vendors of durable medical equipment to be accredited by an accreditation organization approved by the federal Centers for Medicare and Medicaid Services and recognized by the Department. Provides that no later than 90 days after the effective date of the amendatory Act, the Department shall file proposed rules in accordance with the Illinois Administrative Procedure Act to implement this requirement. Provides that no later than 15 months after the effective date of the rule, all vendors must meet the accreditation requirement. Provides that the Department may contract with a third-party vendor to audit eligible durable medical equipment suppliers. | Appropriations-Human Services Comm. | Neutral |
| HB5750 | Harris, D-Chicago | Creates the Health Insurance Claims Assessment Act. Imposes an assessment of 1% on claims paid by a health insurance carrier or third-party administrator. Provides that the moneys received and collected under the Act shall be deposited into the Healthcare Provider Relief Fund and used solely for the purpose of funding Medicaid services provided under the medical assistance programs administered by the Department of Healthcare and Family Services. | Appropriations-Human Services Comm. | Neutral |
| HB5751 | Ives, R-Wheaton | Amends the Workers' Compensation Act. Provides that no medical provider shall be reimbursed for a supply of prescriptions filled outside of a licensed pharmacy except when there exists no licensed pharmacy within 5 miles of the prescribing physician's practice. Provides that, if there exists no licensed pharmacy within 5 miles of the prescribing physician's practice, no medical provider shall be reimbursed for a prescription, the supply of which lasts for longer than 72 hours from the date of injury or 24 hours from the date of first referral to the medical service provider, whichever is greater, filled and dispensed outside of a licensed pharmacy. Provides that the limitations on filling and dispensing prescriptions do not apply if there exists a pre-arranged agreement between the medical provider and a preferred provider program regarding the filling of prescriptions outside a licensed pharmacy. | Rules Comm. | Neutral |
| HB5809 | Mussman, D-Schaumburg | Amends the Pharmacy Practice Act. Provides that "practice of pharmacy" includes the prescribing and dispensing of hormonal contraceptive patches and self-administered oral hormonal contraceptives. Defines "hormonal contraceptive patch" as a transdermal patch applied to the skin of a patient, by the patient or by a practitioner, that releases a drug composed of a combination of hormones that is approved by the United States Food and Drug Administration to prevent pregnancy and "self-administered oral hormonal contraceptive" as a drug composed of a combination of hormones that is approved by the United States Food and Drug Administration to prevent pregnancy and that the patient to whom the drug is prescribed may take orally. Allows pharmacists to prescribe and dispense contraceptives to a person over 18 years of age and a person under 18 years of age only if the person has evidence of a previous prescription from a primary care or a women's health care practitioner. Requires the Department of Financial and Professional Regulation to adopt rules to establish standard procedures for pharmacists to prescribe contraceptives. Provides requirements for the rules to be adopted by the Department. Provides that all State and federal laws governing insurance coverage of contraceptive drugs and products shall apply to this Section. | Rules Comm. | Support |
| HB5949 Same as SB2901 |
Zalewski, D-Riverside | Amends the Pharmacy Practice Act. Extends the repeal of the medicine locking closure package pilot program from January 1, 2017 to January 1, 2018. Effective immediately. | Rules Comm. | Neutral |
| HB6158 | Willis, D-Northlake | Amends the Medical Assistance Article of the Illinois Public Aid Code. Provides that on or after July 1, 2016, drugs which are prescribed to residents of a nursing home shall not be subject to prior approval as a result of the 4-prescription limit. Effective July 1, 2016. | Rules Comm. | Neutral |
| HB6180 Same as SB3336 |
McAuliffe, R-Chicago | Amends the Pharmacy Practice Act. Requires pharmacies to establish and maintain a quality assurance program designed to prevent dispensing errors as well as a process designed to detect and identify dispensing errors. Requires pharmacies to commence an investigation into any detected dispensing errors within 2 days after the date the dispensing error is discovered. Requires that if an investigation into a dispensing error indicates that the dispensing error is attributable, in whole or in part, to the pharmacy or its personnel, that a quality assurance review be performed. Provides requirements for the quality assurance review and its records. Provides that the records of the quality assurance review shall not be subject to discovery in any arbitration, civil, or other proceeding, except in certain circumstances. Effective 12 months after becoming law. | Rules Comm. | Oppose |
Professional Affairs
Strategy for dealing with fomepizole shortage: revisiting the use of alcohol as an antidote
by Katherine V. Zych, PharmD, BCPS, PGY2 Drug Information Resident, UIC College of Pharmacy; Anthony M. Burda, BS.Pharm, DABAT, Illinois Poison Center; Carol DesLauriers, PharmD, DABAT, Illinois Poison Center
Documented ethylene glycol or methanol serum concentration >20 mg/dL (>200 mg/L)
OR
Documented/suspected recent history of ingestion with an osmolal gap > 10 mOsm/kg H2Oa
OR
Documented/suspected history of ingestion plus two or more of the following criteria:
|
| aOsmolal gap calculated after the ethanol contribution is subtracted. Absence of a wide osmolal gap does not exclude toxic alcohol poisoning. |
| Fomepizole | Ethanol | |
| ADH inhibition/ affinity | Highly competitive | Lower affinity and transient inhibition due to self-metabolism |
| Therapeutic drug monitoring | Not necessary | Frequent (every 1 to 2 hours) |
| Availability | Limited due to shortages | Good (especially oral formulation) |
| Cost | Higher acquisition cost; possibly lower cost of monitoring | Inexpensive acquisition cost; possibly higher cost of monitoring |
| Loading Dose | All patients | 10% IV solution
10 mL/kg over 1 hour as tolerated
|
40% oral solution 2 mL/kg over 1 hour as tolerated |
| Maintenance dosing | Alcohol naïve
__________________
Alcohol experienced
|
1 to 1.6 mL/kg/hr 1.9 mL/kg/hr
|
0.3 mL/kg/hr to 0.4 mL/kg/hr
______________________
0.5 mL/kg/hr
|
| Maintenance dosing | During hemodialysis
(Alcohol naïve and alcohol experienced)
|
3 mL/kg/hr to 4.3mL/kg/hr | 0.8 mL/kg/hr to 1.1 mL/kg/hr |
| Intravenous | Oral |
Advantages
Disadvantages
|
Advantages
Disadvantages
|
- Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2014 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clinical Toxicology. 2015;53(10):962-1147.
- McMartin K, Jacobsen D, Hovda KE. Antidotes for poisoning by alcohols that form toxic metabolites. [published online ahead of print November 9, 2015]. Br J Clin Pharmacol. doi:10.1111/bcp.12824.
- Hoffman RS, Howland MA, Lewin NA, Nelson L, Goldfrank LR, Flomenbaum N. Goldfrank's toxicologic emergencies. 10th ed. New York:McGraw-Hill Education; 2015.
- Drug Shortages (Fomepizole Injection). American Society of Heath-System Pharmacists website. http://www.ashp.org/. Updated November 19, 2015. Accessed December 2, 2015.
- Barceloux D. G BGR, Krenzelok E. P, Cooper H, Vale J. A. American Academy of Clinical Toxicology Ad Hoc Committee on the Treatment Guidelines for Methanol Poisoning. American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol. 2002;40(4):415-446.
- Barceloux DG, Krenzelok EP, Olson K, Watson W. American Academy of Clinical Toxicology Practice Guidelines on the Treatment of Ethylene Glycol Poisoning. Ad Hoc Committee. J Toxicol Clin Toxicol. 1999;37(5):537-560.
- Antizole [package insert]. San Diego, CA: Amylin Pharmaceuticals Inc; 2007.
Educational Affairs
2016 Spring Meeting Poster Abstracts
EDITOR’S NOTE: For a detailed list of all posters as presented at the 2016 Spring Meeting, please refer to the Spring Meeting Syllabus, pages 14-16. Poster numbers as presented at the meeting are in parenthesis below. For Platform Presentations, please refer to the Spring Meeting Syllabus, page 10. All research was to have results and conclusions by the time of presentation. This may not be reflected in the posted abstracts below.
PLATFORM PRESENTATIONS
- Reducing adverse drug event risks for geriatric patients by optimizing prescribing for selected medication records
- Economic impact of major adverse drug events using hospital chargemaster data in 2014-2015
ORIGINAL
- Sacubitril; Losartan the next treatment for heart failure?
- The role of tenofovir in preexposure prophylaxis of herpes simplex virus type 2: a systematic review
- Calcium and Vitamin D co-supplementation in Gestational Diabetes Mellitus
- Oral lorazepam for seizure prophylaxis in adult patients treated with high dose intravenous busulfan before hematopoietic stem cell transplantation: A retrospective study
- Evaluation of a Protocol used to Screen and Control Glycemic Levels Following Total Orthopedic Knee and Hip Surgeries
- Analysis of Risk Factors and Antipsychotic Usage Patterns Associated with Terminal Delirium in a Veteran Inpatient Hospice Population
- Redesigning PGY1 Pharmacy Residency Interview Structure
- Impact of pharmacists within a multidisciplinary team on chronic obstructive pulmonary disease (COPD) readmission rates
- Efficacy, nephrotoxicity, and incidence of Clostridium difficile infection with broad spectrum antibiotic regimens in patients with nosocomial pneumonia
- Evaluation of fall risk in dementia patients on an atypical antipsychotic in the VA population
- Digoxin and Time to Cardiac-Related Hospitalizations: A Retrospective Cohort Study
- A Performance Improvement Approach to Implementing a Pharmacist-led Medication Education Program in a Community Hospital
- Evaluation of a Pilot Benzodiazepine Taper Clinic in Veterans with Concurrent Opioid Use
ENCORE
- Implementation of decentralized pharmacy technicians to improve medication delivery and nursing satisfaction
- Global Initiatives to Streamline Pharmacy Education and Workforce Development
- Antifungal prophylaxis consideration in patients being treated with blinatumomab for Philadelphia chromosome-negative relapsed or refractory b-cell acute lymphoblastic leukemia: a case report
- Differences in Clostridium difficile infection outcomes between guideline concordant and discordant therapy
STUDENT
- Assessment of healthcare needs of elderly patients in rural communities of central Illinois
- Effectiveness of Pharmacy Practice Model Initiative Competency
- Desmopressin (DDAVP) Dose Changes Post Discharge in Pediatric Patients with Diabetes Insipidus Receiving Oral DDAVP Compounded from Nasal Spray Inpatient
- Retrospective analysis of osteoporosis risk factors among the Chinese population
- Comparison of oral morphine equivalent doses vs. PHQ9 scores in a family practice setting
- Phytopharmacological evaluation of chamomile (Matricaria recutita L.) for indirect modulation of the endocannabinoid system
- Comparison of Pharmacist and Physician Attitudes and Knowledge of Pain Management
ICHP Poster Presentations – Platform Presentation #1
Category: Original - Research Complete
Title: Reducing adverse drug event risks for geriatric patients by optimizing prescribing for selected medication records
Purpose: To improve the age-appropriate prescribing for selected medications in patients over 65 years old, to decrease the potential for adverse drug reactions (ADRs).
Methods: This trial was conducted at a 600+ bed level 1 trauma center in Peoria, IL, which utilizes an electronic health record (EHR) with pre-selected or default medication doses and frequencies. To reduce potential ADRs associated with medication prescribing, seven medications (amitriptyline, cyclobenzaprine, diphenhydramine (oral and intravenous), glimepiride, glipizide, and glyburide were identified. These medications were selected because, their default doses and/or frequencies in the EHR did not adhere to age-appropriate guidelines as described by BEERs. The BEERs list, published in 1991, described the development of a consensus list of medicines considered to be inappropriate for geriatric patients and is endorsed by The American Geriatrics Society. It includes medications that should be avoided, and medications that should be used with extra caution, either in all elderly or in certain populations.1 Changes in doses and or frequencies were made based on recommendations from the BEERs criteria and the geriatric dosing provided in Lexi-Comp.2 EHR reports were obtained for two six month periods, baseline and follow up. The follow up period began two months after changes were implemented to ensure full integration. The percentage of medication orders within the geriatric appropriate dose and/or frequency targets were measured for both the baseline and follow up periods.
Results: Positive changes in physician prescribing habits were seen in four out of seven medications, including cyclobenzaprine, diphenhydramine (both oral and intravenous), glimepiride and glipizide. The baseline percentage of orders within the target dose range compared to the follow up period were cyclobenzaprine (39.1% vs 61.1%), diphenhydramine oral (39.2% vs 49.4%), diphenhydramine intravenous (55.2% vs 57.4%), glimepiride (19.6% vs 21.9%), and glipizide orders (14.1% vs 21.5%).
References
1. American Geriatrics Society 2015 Beers Criteria Update Expert Panel.
American Geriatrics Society 2015 updated Beers criteria for potentially
inappropriate medication use in older adults. J Am Geriatr Soc 2015 Oct 8. doi: 10.1111/jgs.13702. [Epub ahead of
print].
2. Lexi-Comp. Accessed August 2014.
Conclusion: Improved compliance was achieved with physician ordering of medications (cyclobenzaprine, oral and intravenous diphenhydramine, glimepiride and glipizide) for patients over 65 years old by adjusting the default dose and or frequency, using evidence based criteria. Although not specifically measured in this initiative, it is concluded that the risk of ADEs were reduced by adjusting the EHR default doses and frequencies for these selected medications.
Submitting Author: Amy B. Maxfield, BS Pharm
Submitting Organization: OSF SFMC
Authors: Amy B. Maxfield, BS Pharm; Heather M. Harper, PharmD, BCPS
ICHP Poster Presentations – Platform
Presentation #2
Winner: Best Platform Presentation 2016
Category: Original - Research Complete
Title: Economic impact of major adverse drug events using hospital chargemaster data in 2014-2015
Purpose: Patient-specific adverse drug events (ADEs) have been previously associated with respective increases in hospitalization costs and length of stay. Literature determining the economic impact of ADEs is relatively outdated, driving health system administrators to apply an inflation factor to previously published figures in the processes to evaluate current cost avoidance of ADE prevention. The purpose of this study is to determine the economic impact of major ADEs on patient hospitalization costs and length of stay (LOS), in present time.
Methods: This study has been approved by the University of Chicago Institutional Review Board. ADEs were identified using both voluntary event reporting data and ICD-9 codes for patients admitted to the University of Chicago Medicine during the time period of April 2014 and May 2015. Case patients experienced a major ADE (as classified as “E” or higher on The National Coordination Council for Medication Errors Reporting and Prevention [NCC-MERP] Index for Categorizing Medication Errors). Controls matched by admission during study time period, classification by diagnosis related group, age (±2 years), and sex of each case were included. Using eSimon (Algonquin, IL), a hospital cost accounting system, total cost of hospitalization and length of stay were determined for both cases and controls. All analyses were performed using a two-sample Wilcoxon rank-sum (Mann-Whitney) test in STATA (College Station, TX).
Results: Of a total of 416 patients who experienced major ADEs evaluated for inclusion in the study, 242 were matched with controls for analysis. The drug classes primarily accounting for studied major ADEs include chemotherapy (38%), corticosteroids (14%) and opioids (11%). Mean cost of hospitalization between patients who experienced a major ADE and those who did not differed significantly ($38,239.31 vs. $47,138.04, p=0.0440), as well as in mean LOS (8.03 vs. 9.92 days, p=0.005).
Conclusion: This study determined total cost of hospitalization and LOS remains significantly higher for patients experiencing major ADEs than those who did not.
Submitting Author: Bryan C. McCarthy Jr., PharmD, MS, BCPS
Submitting Organization: University of Chicago Medicine
Authors: Bryan C. McCarthy Jr., PharmD, MS, BCPS; Tara P. Driscoll, PharmD; Kristin A. Tuiskula, PharmD; Andrew M. Davis, MD, MPH
ICHP Poster Presentations – Original
#1
(presented as Poster #14)
Category: Original - Research Complete
Title: Sacubitril; Losartan the next treatment for heart failure?
Purpose: Congestive heart failure (CHF) is a leading cause of morbidity and mortality for which there are few recent improvements in treatment. Over one million US patients on optimized drug therapy are hospitalized each year. Identification of neurohormonal mechanisms that do not overlap with existing therapies are needed. The enzyme Neprilysin impairs endogenous vasoactive compounds, including natriuretic peptide leading to diuresis, natriuresis, and vasodilation. Sacubitril, a neprilysin inhibitor in combination with valsartan is the first of these treatments to show morbidity and mortality benefit compared to enalapril, as reported in the PARADIGM-HF trial. The purpose of this study is to analyze the safety and efficacy data available on sacubitril; valsartan (SV) and to determine if there is a role for the drug in the clinical treatment of CHF.
Methods: A systematic review of the databases PubMed, MedLine, and EMBASE was performed up to December of 2015. The following keywords were used: heart failure, neprilysin, ACE inhibitors, ARB, sacubitril, vasopeptidise inhibitor, PARADIGM-HF. Inclusion criteria included: 1) adult patients with NYHA class II-IV HF with ejection fraction <40% 2) treatment with SV 3) direct comparison to recommended treatment with an ACE-I 4) inclusion of morbidity, mortality, and safety outcomes 5) CEBM level of evidence 2b or greater. Only one randomized control trial met all specified inclusion criteria. It was therefore decided to include retrospective analyses of this trial due to the novelty of this subject. Two secondary analyses were identified as relevant and included in safety and efficacy analysis.
Results: The use of SV compared to enalapril in the treatment of HF was found to significantly reduce the risk of death (17% vs. 19.8% NNT 36) from any cause and (13.3% vs. 16.5% NNT 31) from cardiovascular causes, and time to first hospitalization for CHF (12.8% vs. 15.6% NNT 36). Safety data for SV found patients experiencing significantly less angioedema, renal impairment, or adverse events leading to discontinuation compared to enalapril. However a significant (18% vs. 12%; NNH 17) increase in hypotension was found for patients on SV compared to enalapril. Secondary analysis revealed that the mortality benefit for SV is primarily related to a modification in the risk for sudden death or to worsening heart failure. This benefit was comparable amongst patients of all ages, except for the very oldest in the outcome of CV death and the composite outcome of CV death and heart failure hospitalizations.
Conclusion: More research is needed before clinicians should use SV for the treatment of heart failure, despite the positive outcomes of the PARADIGM-HF trial. The morbidity and mortality benefits found may not generalize to the population at large in the setting of the trial’s limitations. The most concerning of these being that there is only a single RCT comprised majorly of clinically stable white males to support the use of SV over ACE-I. The authors also chose to compare the maximum recommended dose of the ARB component of SV to a low-dose of enalapirl, making it possible that the clinical benefits found were due to greater RAAS inhibition. Additionally, 12% of patients dropped out of the active run-in period due to side effects making it likely that the rates of adverse reactions reported, including angioedema, are lower than would be expected in practice. Moreover, the authors chose to omit findings from pre-clinical trials that demonstrated an increase in CSF beta-amyloid protein for patients receiving SV. For these reasons it is difficult to justify the significant cost associated with SV, which is approximately 100x that of enalapril, until further safety and efficacy analysis can be completed.
Submitting Author: Michael Fotis, RPh
Submitting Organization: Northwestern University Feinberg School of Medicine
Authors: Tara Marcus PA-S2, Master of Medical Sciences Candidate; Michael Fotis, RPh
ICHP Poster Presentations – Original
#2
(presented as Poster #1)
Category: Original - Research Complete
Title: The role of tenofovir in preexposure prophylaxis of herpes simplex virus type 2: a systematic review
Purpose: Herpes simplex virus type 2 (HSV-2) is among the most common sexually transmitted infections, affecting approximately 417 million sexually active adults worldwide [1]. HSV-2 is the leading cause of genital ulcers, and is associated with pain, itching, negative social stigma and increased risk for HIV-1 [2]. Preventative measures include barrier methods, abstinence, and chronic antiviral suppressive therapy for HSV-2 positive patients. There is not a vaccination or medication for preexposure prophylaxis (PrEP) for HSV-2. The purpose of this study is to assess the efficacy of the nucleotide reverse-transcriptase inhibitor, tenofovir, in the preexposure prophylaxis of HSV-2.
Methods: Data sources included PubMed, Cochrane Library and Embase between 1966-2015. Search terms included, “ tenofovir prevention herpes simplex virus type 2”. A total of 222 articles resulted. Inclusion criteria were set as randomized controlled trials with human participants conducted over the last 5 years, which yielded 2 studies. The dominant reason for exclusion was non-human participants. The main outcome measured is HSV-2 seroconversion.
Results: In one study, the incidence rate of HSV-2 was 10.2 cases per 100 person years with pericoital application of tenofovir gel, compared to incidence rate of HSV-2 of 21.0 cases per 100 person-years with placebo gel, NNP = 9.8 [3]. A second study resulted in an incidence rate of HSV-2 of 5.6 cases per 100 person years with oral tenofovir-based PrEP, compared to 7.7 cases per 100 person years with placebo, NNP = 37.1 [4].
References
1. Looker, K.J., et al., Global and Regional Estimates of Prevalent and
Incident Herpes Simplex Virus Type 1 Infections in 2012. PLoS One, 2015. 10(10): p. e0140765.
2. Tan, D., Potential role of tenofovir vaginal gel for reduction of risk of
herpes simplex virus in females. Int J
Womens Health, 2012. 4: p. 341-50.
3. Abdool Karim, S.S., et al., Tenofovir Gel for the Prevention of Herpes
Simplex Virus Type 2 Infection. N Engl J
Med, 2015. 373(6): p. 530-9.
4. Celum, C., et al., Daily oral tenofovir and emtricitabine-tenofovir
preexposure prophylaxis reduces herpes simplex virus type 2 acquisition among
heterosexual HIV-1-uninfected men and women: a subgroup analysis of a
randomized trial. Ann Intern Med,
2014. 161(1): p. 11-9.
Conclusion: Tenofovir-based therapy significantly reduced HSV-2 seroconversion in two double-blinded, randomized controlled trials. Periocoital tenofovir gel resulted in a 51% absolute decrease in HSV-2 seroconversion, while oral tenofovir-based therapy resulted in a 30% absolute decrease in HSV-2 seroconversion, suggesting that topical therapy is more effective in preventing HSV-2 seroconversion compared to oral therapy, although future studies comparing topical and oral tenofovir therapy for PrEP of HSV-2 are needed. Limitations of the studies are: neither study was originally designed to assess the effect of tenofovir on HSV-2 acquisition thus randomization at study enrollment was not stratified by HSV-2 status; the studies do not use the same formulation of tenofovir and neither study assesses the timing of HSV-2 acquisition in relation to plasma tenofovir levels; given the current cost of oral tenofovir, this may be a very costly option; widespread and long-term use of tenofovir may lead to increased viral resistance. This systematic review suggests that there is a potential role of tenofovir to prevent HSV-2 acquisition, which could reduce genital ulcers, pain, social stigma and HIV risk associated with HSV-2.
Submitting Author: Michael Fotis, RPh
Submitting Organization: Northwestern University Feinberg School of Medicine
Authors: Julia Silver PA-S2, Master of Medical Sciences Candidate; Michael Fotis, RPh
ICHP Poster Presentations – Original
#3
(presented as Poster #13)
Category: Original - Research Complete
Title: Calcium and Vitamin D co-supplementation in Gestational Diabetes Mellitus
Explain the strengths and the limitations of the clinical data supporting the use of supplementation of calcium and vitamin D during pregnancy to improve maternal outcomes in patients with gestational diabetes.
Purpose: The purpose of this poster is to examine if vitamin D and calcium co-supplementation is an effective intervention during pregnancy to improve maternal outcomes in patients with gestational diabetes (GDM). Diabetes is a significant cause of morbidity and mortality in the US, and an important economic burden. The CDC estimates up to 9.2% of pregnancies are affected by GDM. Available studies examining the relationship between Vitamin D deficiency and insufficiency in patients with GDM and associated maternal outcomes are inconsistent in their findings. Although the mechanism of effect is unclear there a few studies of Vitamin D and calcium co-supplementation reporting promising results.
Methods: A systematic review was conducted using EMBASE, PubMed, and MedLine databases between October and December 2015. Search terms included: Calcium, Vitamin D, and Gestational Diabetes. Studies written in English were included in this review. Studies that did not examine gestational diabetes or did not examine co-supplementation of calcium and vitamin D were excluded. Under these inclusion and exclusion criteria a total of 2 eligible studies were identified. The studies were CEBM level of evidence 1b.
Results: Karamali in a randomized placebo controlled trial of 60 patients found that Vitamin D and calcium co-supplementation in women with GDM decreased the rates of many maternal and neonatal outcomes. There was a significant reduction in cesarean rates from 63% to 23% the number needed to treat (NNT) estimated as 2.5, and for maternal hospitalization from 13% to 0 (NNT=7). For neonatal hyperbilirubinemia the NNT=2.7, neonatal hospitalization was reduced from 57% to 20% (NNT = 2.7), and macrosomia NNT = 3.
Asemi in a randomized placebo controlled trial of 56 patients found statistically significant improvement in laboratory values for fasting plasma glucose, serum insulin, HOMA-R, LDL cholesterol, total cholesterol: HDL cholesterol, HDL cholesterol, GSH, and MDA. Clinical outcomes were not measured in this trial.
Both studies had the same intervention length of 6 weeks with 1,000mg of calcium carbonate daily over 6 weeks, and 50,000U of Vitamin D3 two times during the intervention, once at baseline and once on day 21 of the intervention.
Conclusion: The two RCTs examined in this systematic review found co-supplementation with calcium and vitamin D improved maternal laboratory results and improved maternal outcomes. There are limitations to note: studies are small, both were conducted in Iran and may lack external validity, only a single small trial measured clinical outcomes where maternal outcomes were secondary outcomes and may not have been appropriately powered to detect differences. Further well-designed, high powered, randomized controlled trials investigating the impact on maternal and fetal outcomes are necessary to determine a clinical effect. If a positive effect is established, future studies can focus on the optimal amount of supplementation and the timing during pregnancy. While the studies did not report adverse events, one separate study has determined that a 300,000 intramuscular dose of Vitamin D is safe and efficacious in pregnant women, and the National Institute of Health recommends 1,000mg of calcium carbonate daily for pregnant and lactating women. Furthermore, with possible similarities in the pathophysiology of GDM and diabetes, and the risk of progression from GDM to Type 2 DM, the effects of co-supplementation in diabetes mellitus could also be explored.
Submitting Author: Michael Fotis, RPh
Submitting Organization: Northwestern University Feinberg School of Medicine
Authors: Christina Hill PA-S2, Master of Medical Sciences Candidate; Michael Fotis, RPh
ICHP Poster Presentations – Original
#4
(presented as Poster #17)
Category: Original - Research in Progress
Title: Oral lorazepam for seizure prophylaxis in adult patients treated with high dose intravenous busulfan before hematopoietic stem cell transplantation: A retrospective study
Purpose: To determine the efficacy of oral lorazepam in preventing seizures in adult patients receiving high dose intravenous busulfan prior to allogeneic hematopoietic stem cell transplant (HSCT).
Methods: This is a single center study conducted at Rush University
Medical Center (RUMC) located in Chicago, Illinois.
• This retrospective study was approved by the Institutional Review Board prior
to data collection.
• A stem cell transplant database was used to identify patients who have
received allogeneic HSCTs from January 1, 2009 to March 31, 2015.
• Patients were included if they were ≥ 18 years old, received intravenous high
dose busulfan, received oral lorazepam for seizure prophylaxis.
· Patients were excluded only if they received concomitant phenytoin.
• RUMC's electronic medical record system and the stem cell transplant database will be used to collect the following: age, sex, race, underlying malignancy, type of transplant, conditioning regimen, dates of busulfan administration, fever during busulfan administration.• Medication charts were reviewed for past medical history of seizures, illegal drug use, AIDS, and CNS malignant disease involvement at or during diagnosis.
• The primary endpoint is the occurrence of seizures from the start of busulfan until 72 hours following the completion of busulfan.
• Per RUMC policy, patients receive oral lorazepam 0.5 mg every 6 hours starting 24 hours prior to busulfan administration and continuing for 48 hours after the completion of busulfan.
• Categorical variables will be analyzed using Chi square or Fischer's Exact test.
Results: Research in progress
Conclusions: Research in progress
Submitting Author: Monica Timmerman, PharmD candidate
Submitting Organization: Midwestern
University Chicago College of Pharmacy and Rush University Medical Center
Authors: Monica Timmerman, PharmD candidate; Lisa M. DiGrazia, PharmD, BCPS, BCOP; Amanda N. Seddon, PharmD, BCPS, BCOP; Annette Gilchrist, PhD
ICHP Poster Presentations – Original
#5
(presented as Poster #4)
Category: Original - Research in Progress
Title: Evaluation of a Protocol used to Screen and Control Glycemic Levels Following Total Orthopedic Knee and Hip Surgeries
Purpose: Perioperative hyperglycemia can affect a patient’s recovery following orthopedic surgery by increasing the risk of complications including infection and by increasing patient length of stay. Currently, our institution does not have a standardized glucose management protocol for this patient population. The objective of this study is to implement a protocol that can effectively manage patient’s glucose levels post-operatively and decrease the rate of post-op infections in patients who have undergone a total orthopedic knee or hip surgery.
Methods: Patients undergoing elective orthopedic knee or hip surgery will first have Hemoglobin A1c labs drawn during preadmission testing. Patients with an A1c <8 will undergo surgery as planned while patient with an A1c >8 will be referred to their primary care physician to help manage their glucose levels. Their surgery will be postponed until the patient can provide documented glucose logs demonstrating glucose control and management over a 4 week period. Once patients undergo surgery their glucose level will be managed by a P&T approved protocol using a sliding scale or basal plus correction method of insulin administration. Both non-diabetic and diabetic patient’s glucose will be managed by this protocol. This study will compare the management of patient glucose levels prior to and after the initiation of the protocol. The primary outcome of the study is the rate of post-operative infection. Secondary outcomes include the average glucose on post-operative days 0, 1, 2, and 3. Other outcomes include nursing satisfaction and number of patients who are found to have new onset diabetes.
Results: Research in Progress
Conclusions: Research in Progress
Submitting Author: Patrick D. Hammond, PharmD
Submitting Organization: Presence St. Joseph Medical Center
Authors: Patrick D. Hammond, PharmD; Rishita Shah, PharmD
ICHP Poster Presentations – Original
#6
(presented as Poster #2)
Category: Original - Research in Progress
Title: Analysis of Risk Factors and Antipsychotic Usage Patterns Associated with Terminal Delirium in a Veteran Inpatient Hospice Population
Purpose: The purpose of this study is to (1) Identify risk factors for terminal delirium in a VA inpatient hospice population (2) Assess usage patterns of antipsychotics in terminal delirium (3) Describe nursing assessment, non-pharmacological and pharmacological interventions, and documentation of terminal delirium
Methods: This is a retrospective case-control study of patients who expired in the Edward Hines, Jr. VA Hospital Community Living Center (CLC) under the treating specialty “NH hospice” during the period of October 1, 2013 to September 30, 2015. Cases are defined as patients who were treated with antipsychotics for terminal delirium within the last two weeks of life. Controls are defined as patients who were not treated with antipsychotics for terminal delirium within the last two weeks of life. All patients enrolled under the treating specialty “NH Hospice” will be evaluated with the exclusion of living hospice patients and patients discharged to receive home hospice care prior to death. Patients’ medical records will be reviewed from two weeks prior to death until the recorded death date during which the following will be assessed from the medical record as available: age, terminal diagnosis, time interval cancer diagnosis and death, war era, comorbid conditions, prescribed antipsychotic medications, other medications potentially contributing to delirium, documentation for antipsychotic use, non-pharmacological interventions, and date of death.
Results: Research in progress
Conclusions: Research in progress
Submitting Author: Emily Ellsworth, PharmD
Submitting Organization: Edward Hines, Jr. VA Hospital
Authors: Emily Ellsworth, PharmD; Kevin Bacigalupo, PharmD, BCPS; Kavita Palla, PharmD, BCPS; Seema Limaye, MD; Margaret Walkosz, ACHPN, GNP-BC; Sandra Szczecinski, BSN; Katie Suda, PharmD, MS
ICHP Poster Presentations – Original
#7
(presented as Poster #8)
Category: Original - Research in Progress
Title: Redesigning PGY1 Pharmacy Residency Interview Structure
Purpose: The structure of our PGY1 residency interview day was redesigned to increase objectivity in candidate evaluations and exposure of candidates to the activities in our department while decreasing the preceptor time commitment.
Methods: In 2015 the PGY1 recruitment team incorporated multiple mini interviews (MMI), interdisciplinary rounds and a departmental activity in the interview days for PGY1 residency candidates for the 2015 recruitment season. Each multiple mini interview assessed specific qualities deemed to be essential in pharmacy residency training and utilized standardized evaluation tools. In 2016, the interview day was again restructured to adjust the time candidates spend rounding, eliminated one of the MMIs and implemented a one-on-one discussion session with the candidates and a current resident. Following the interviews, candidates were sent an electronic survey to evaluate their satisfaction with the interview day and the new structure. Descriptive statistics were used to describe the survey results from 2015 and survey results from 2016 are pending. Preceptor time for interview days in 2015 and 2016 will be compared with the amount of time required of preceptors in previous years.
Results: In 2015 a total of 72 candidates were interviewed and 49 completed the post-interview survey. The activities that left the highest positive impression during the interview day were the introduction section, departmental activity and traditional interview sessions. The majority of candidates (84%) stated that the interview day increased their desire to pursue residency training at University of Chicago and felt that time was adequately appropriated between activities. Preceptor time for candidate interviews decreased by 72% (600 hours vs 168 hours) and from 7.1 hours per candidate to 2.3 hours per candidate. With the new structure, the number of candidates per day was increased allowing us to decrease the number of interview days by 36%. Results from 2016 are in progress.
Conclusion: The restructuring of the interview day in 2015 provided resident a positive impression of our residency program while requiring fewer preceptor hours dedicated to interviewing. These results will be compared and new conclusions drawn off of the research conducted on the 2016 interview cycle.
Submitting Author: Hailey P. Soni PharmD
Submitting Organization: University of Chicago
Authors: Hailey P. Soni PharmD; Shannon Rotolo, PharmD; Mary Kate Miller, PharmD; Jennifer Austin Szwak, PharmD
ICHP Poster Presentations – Original
#8
(presented as Poster #6)
Category: Original - Research in Progress
Title: Impact of pharmacists within a multidisciplinary team on chronic obstructive pulmonary disease (COPD) readmission rates
Purpose: In FY2015, the Centers for Medicare and Medicaid Services (CMS) expanded the existing algorithm accounting for readmission of patients to include those admitted for an acute exacerbation of chronic obstructive pulmonary disease (AECOPD). The Medicare Hospital Readmissions Reduction Program (HRRP) penalizes hospitals for excess early readmissions of patients with AECOPD. Currently, the penalty is in place for all-cause 30 day readmissions. The purpose of this study is to evaluate the impact of pharmacists within a multidisciplinary team on chronic obstructive pulmonary disease (COPD) readmission rates.
Methods: Patients were identified at admission to University of Chicago Medicine using an algorithm that identified documented COPD. On admission, a medication history was performed by a pharmacist or student pharmacist during which five COPD-focused questions were asked to each patient. The patients were then seen by the pulmonary advanced practice nurse (APN). After being seen by the APN, the pharmacy department provided inhaler education utilizing the teach-to-goal (TTG) method. Once the patient was discharged, a follow up appointment was scheduled within approximately seven to ten days with the pulmonary APN. During this follow up appointment, the pharmacy department provided further inhaler education using TTG. The primary endpoint of this study was COPD readmission in 30 days. The secondary endpoints were to show an increase in completed medication histories and an improvement in patients’ inhaler techniques using the TTG method. COPD readmission rates were determined by reporting from the hospital’s quality department. Improvement in patients’ inhaler techniques was evaluated through a systematic scoring system which allowed for the comparison of initial and final inpatient technique scores.
Results: Research in progress. Preliminary data collection comparing scores before TTG session and after TTG session in the inpatient setting shows the average increase in TTG score was 4.9 points for the MDI inhaler (percentage change 20.3%). For the tiotropium inhaler, the average increase in the TTG score was 6 (percentage change of 20%).
Conclusions: Research in progress
Submitting Author: Leigh A. Moffett, PharmD, BCPS
Submitting Organization: University of Chicago Medicine
Authors: Leigh A. Moffett, PharmD, BCPS; Jennifer Szwak, PharmD, BCPS
ICHP Poster Presentations – Original
#9
(presented as Poster #3)
Category: Original - Research in Progress
Title: Efficacy, nephrotoxicity, and incidence of Clostridium difficile infection with broad spectrum antibiotic regimens in patients with nosocomial pneumonia
Purpose: Identify the difference in efficacy, nephrotoxicity, and incidence of Clostridium difficile infection between vancomycin plus piperacillin-tazobactam and vancomycin plus cefepime (with or without metronidazole) in patients with nosocomial pneumonia. Vancomycin plus piperacillin-tazobactam is a broad-spectrum antibiotic regimen chosen as empiric therapy for a multitude of infections. Recent data suggest that this combination may increase the risk of nephrotoxicity when compared to vancomycin alone, or when compared to vancomycin plus an alternative beta-lactam antibiotic, such as cefepime. Recently, as a result of these studies and due to recommendations by pharmacy, prescribing at Edward Hines, Jr. VA Hospital has begun to shift from using vancomycin plus piperacillin-tazobactam to a regimen of vancomycin plus cefepime with or without metronidazole for anaerobic coverage. This regimen has been chosen for many infections, but most commonly for the nosocomial pneumonias: hospital-acquired pneumonia (HAP), healthcare-associated pneumonia (HCAP), and ventilator-associated pneumonia (VAP). This change in prescribing practices raises many important questions. First, in terms of aspiration pneumonia and VAP, what is the difference in efficacy between vancomycin plus piperacillin-tazobactam and vancomycin plus cefepime plus metronidazole? Additionally, in terms of nosocomial pneumonia without mention of aspiration, what is the difference in efficacy between vancomycin plus piperacillin-tazobactam and vancomycin plus cefepime? Finally, what is the difference in the rates of nephrotoxicity and Clostridium difficile infection associated with these regimens?
Methods: This study has been approved by the Institutional Review Board (IRB). This study is a retrospective, electronic chart review of patients with nosocomial pneumonia. Eligible patients for screening will be identified with active orders of piperacillin-tazobactam plus vancomycin, cefepime plus vancomycin, or cefepime plus vancomycin plus metronidazole. Inclusion criteria for the study include male and female patients ≥ 18 years of age with a clinical diagnosis of nosocomial pneumonia, who had a baseline serum creatinine obtained within 24 hours of admission, and who received one of these broad-spectrum antibiotic regimens for at least 48 hours. Patients will be excluded if they are receiving chronic dialysis or have a diagnosis of end stage renal disease. The primary outcome being evaluated is clinical efficacy of antibiotic regimens, which is reflected as improvement in two of the following three clinical symptoms (fever, leukocytosis/leukopenia, purulent secretions) at 48 hours. A secondary endpoint will be the incidence of Clostridium difficile infection, which is reflected as a positive Clostridium difficile toxin B PCR test with diarrhea (three or more unformed stools passed in 24 hours) or histopathological findings of pseudomembranous colitis within 14 days of starting antibiotics. An additional secondary endpoint of acute kidney injury, defined as an increase in serum creatinine ≥50% from baseline, an increase in serum creatinine of ≥0.5 mg/dL, or a urine output <0.5mL/kg per hour for >6 hours, will also be evaluated. Data collection will include demographics, classification/etiology of pneumonia, temperature, WBC count, blood pressure, pulse, sputum production, clinical improvement, use of broad-spectrum antibiotic regimens, number of days on oral or IV antibiotics in the previous 14 days, concomitant use of nephrotoxic drugs, and documented adverse drug reactions to antibiotics.
Results: Research in progress.
Conclusions: Research in progress.
Submitting Author: Kaitlyn B. Kalata, PharmD
Submitting Organization: Edward Hines, Jr. VA Hospital
Authors: Kaitlyn B. Kalata, PharmD; Sue Kim, PharmD, BCPS; Ursula C. Patel, PharmD, BCPS, AQ-ID; Raymond Byrne, PharmD, BCPS
ICHP Poster Presentations – Original
#10
Winner: Best Original Poster Presentation
2016
(presented as
Poster #16)
Category: Original - Research in Progress
Title: Evaluation of fall risk in dementia patients on an atypical antipsychotic in the VA population
Purpose: Antipsychotics are widely used as off-label treatment for behavioral symptoms in dementia patients. It is recognized that antipsychotics can increase the risk for falls in the elderly population. When used in dementia patients, this risk is further increased, since dementia itself is an independent risk factor for falls. A study on the use of antipsychotics in the Veterans Affairs (VA) Community Living Centers (CLC) found that veterans residing in the dementia special care units were more likely to receive an antipsychotic, more commonly atypical antipsychotics. The purpose of this study is to determine whether atypical antipsychotics increase fall risk in dementia patients.
Methods: This study was approved by the Institutional Review Board. This study will be a retrospective cohort study comparing two groups in the VA population: dementia patients receiving atypical antipsychotics versus dementia patients not receiving atypical antipsychotics. The primary endpoint is the difference in the incidence of falls between the two cohort groups. The secondary endpoints are the differences in the incidence of falls between subtypes of dementia, different atypical antipsychotics, and different fall risk as defined by the Morse Scale. Primary endpoint will be analyzed using unpaired t-test, while secondary endpoints will be analyzed through descriptive analysis. The following data will be collected: age, gender, number of other Fall Risk Increasing Drugs (FRIDs), comorbid conditions that can also increase fall risk, subtype of Dementia, type of atypical antipsychotics, fall risk as defined by Morse Scale, and the documented fall. Each patient’s chart will be reviewed from admission and up to 6 months, or patient’s discharge, or patient's death whichever is the earliest to determine if a documented fall has occurred during that time. Determining fall risk in the dementia population receiving atypical antipsychotics can help prevent inappropriate prescribing of these agents for treatment of behavioral symptoms, leading to decreased fall risk.
Results: Research in Progress
Conclusions: Research in Progress
Submitting Author: Lianna Serbas, PharmD, PGY1 Pharmacy Resident
Submitting Organization: Captain James A. Lovell FHCC
Authors: Lianna Serbas, PharmD; Yinka Alaka, PharmD
ICHP Poster Presentations – Original
#11
(presented as Poster #15)
Category: Original - Research in Progress
Title: Digoxin and Time to Cardiac-Related Hospitalizations: A Retrospective Cohort Study
Purpose: The purpose of this study is to evaluate the safety of digoxin therapy in patients with atrial fibrillation with and without heart failure. The time to first cardiac-related hospitalization will be documented comparing patients with atrial fibrillation with and without digoxin therapy. Additionally, the safety of digoxin will be further analyzed by evaluating the length of digoxin therapy prior to first cardiac-related hospitalization and digoxin serum concentrations. Finally, a sub-group analysis of patients with and without heart failure will be conducted to determine if concomitant heart failure has any impact.
Methods: This study is a retrospective cohort study with two groups of patients: patients with atrial fibrillation receiving digoxin therapy and patients with atrial fibrillation not receiving digoxin therapy. Cardiac event is defined as any of the following: cardiac arrhythmia, acute myocardial infarction, unstable angina, cardiac arrest, hypertensive urgency/emergency, and cardioembolic stroke. Patients included in the study are those who are 18 years of age and older, with one or more inpatient admission with a primary discharge diagnosis of atrial fibrillation or two or more outpatient, nonemergency department encounters for atrial fibrillation. Patients must also have at least one primary care or cardiology clinic visit. The following data will be collected for each patient: initial diagnosis of atrial fibrillation, patient age and gender, past medical history, start date of digoxin therapy, concurrent medications, date of initial hospitalization with a cardiac primary admission diagnosis, primary admission diagnosis, length of hospitalization, admission to ICU or general acute medicine floor, serum digoxin level, admission renal function, troponin, potassium, magnesium, and most recent height and weight. The data collected will be used to assess the time to first hospitalization in patients with atrial fibrillation with or without digoxin therapy. The time to initial hospitalization will be reported in number of days since atrial fibrillation diagnosis, and will be analyzed using a Cox proportional hazards regression. The secondary endpoints for continuous variables will be reported as percentages, means, and standard deviations, and assessed using a student t-test.
Results: Research in Progress
Conclusions: Research in Progress
Submitting Author: Stephanie Dwyer, PharmD, PGY1 Pharmacy Resident
Submitting Organization: Captain James A. Lovell Federal Health Care Center
Authors: Stephanie Dwyer, PharmD; Sherri Stoecklein, PharmD, BCPS
ICHP Poster Presentations – Original
#12
(presented as Poster #7)
Category: Original - Research in Progress
Title: A Performance Improvement Approach to Implementing a Pharmacist-led Medication Education Program in a Community Hospital
Purpose: The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey is a standardized questionnaire that has become an important indicator of the patient’s view of perceived care. The study site was underperforming in the medication-related survey questions: “How often did hospital staff tell you what the medication was for?” and “How often did hospital staff describe possible side effects in a way you could understand?”. The Pharmacy Department wanted to implement an intervention to improve patient satisfaction in this domain. The purpose of the study was to determine the impact of a pharmacist-led medication education program on the medication-related HCAHPS scores.
Methods: The study was conducted at a small community hospital from July to December 2015. All pharmacists and student pharmacists received competency and training to ensure uniformity in the medication education sessions. Patients from two medical-surgical units were targeted to receive medication counseling by a pharmacist or student pharmacist with priority given to those with heart failure, on an oral anticoagulant or receiving 6 or more medications. Nursing home patients and patients with altered mental status were excluded from receiving the intervention. At the end of the month, data was reviewed and changes were made to the process to improve to the target goal of five counseling sessions per day. The primary outcome was change from baseline on medication-related HCAHPS scores. A secondary outcome was number of documented counseling sessions performed, tracked on a daily basis on a department quality improvement board and trended monthly.
Results: The 2015 HCAHPS results regarding the question about explaining medication indications improved by 8% and the scores regarding the question about side effects improved by 36% when comparing the pre and post implementation of the medication education service. 392 patients were counseled as part of the pharmacist-led medication education program with an average of 65 sessions performed per month.
Conclusion: As shown in the study, pharmacist medication counseling can make an impact on the medication-related HCAHPS scores. Medication education is an important aspect of patient communication in the inpatient setting and the launching of this service enhanced patient understanding of the indications and side effects of their medications as measured by these scores.
Submitting Author: Stacy Thomas Scaria, PharmD
Submitting Organization: Tenet Healthcare - Westlake Hospital
Authors: Stacy Thomas Scaria, PharmD; Deanna McMahon Horner, PharmD, BCPS; Dusica Jovic Szczybura, PharmD; Charlene Hope, PharmD, MS, BCPS
ICHP Poster Presentations – Original
#13
(presented as Poster #5)
Category: Original - Research in Progress
Title: Evaluation of a Pilot Benzodiazepine Taper Clinic in Veterans with Concurrent Opioid Use
Purpose: Opioid pain relievers are implicated in nearly 17,000 overdose deaths in the United States. This is over a 100% increase in rates over the first decade of this century. Thirty-one percent of these deaths involved the concurrent use of benzodiazepine sedatives. In late 2013, the Department of Veterans Affairs (VA) launched the Opioid Safety Initiative to reduce the use of opioids among veterans. While the initiative drew attention to clinical considerations regarding the risk of co-administration, a recent medication use evaluation concluded that over 700 Veterans had active outpatient prescriptions for both a benzodiazepine and an opioid at a single VA facility. As a result, a pilot benzodiazepine taper clinic will be implemented at Edward Hines, Jr. VA Hospital in January 2016 in collaboration with the Hines Primary Care and Mental Health Providers to reduce the number of veterans on high dose benzodiazepines and concurrent opioid therapy. An order set for the treatment of insomnia will also be created and integrated into the electronic medical record system in February 2016 at Edward Hines, Jr. VA Hospital to promote and facilitate the use of non-benzodiazepine evidence-based treatment of insomnia. The primary purpose of this quality assurance and quality improvement project is to evaluate potential benefits and barriers to implementing a multidisciplinary benzodiazepine taper clinic at Edward Hines, Jr. VA Hospital.
Methods: The project will assess the reduction in high dose benzodiazepines for the pilot clinic patients. The magnitude and time to dose reduction(s) will be evaluated. High dose benzodiazepines will be defined as total daily doses of temazepam >20 mg, diazepam >10 mg, clonazepam >1 mg, lorazepam >2 mg, and alprazolam >1 mg. Patients receiving opioids for cancer pain, patients receiving a benzodiazepine for back spasms in spinal cord patients, hospice patients, and patients with severe mental health disorders (i.e. bipolar disorder, psychosis) will be excluded. Time spent in preparation for clinic visits, patient contact hours, and time spent for follow up will be logged. Self-reported patient compliance with treatment plans and patient clinic cancellations will be recorded. Additionally, the project will track the use of the newly implemented order set for the treatment of insomnia.
Results: Research in Progress
Conclusion: Research in Progress
Submitting Author: Julie Bucek Cabrera, PharmD, PGY1 Pharmacy Practice Resident
Submitting Organization: Edward Hines Jr., VA Hospital
Authors: Julie Bucek Cabrera, PharmD; Julie Stein, PharmD, VHA-CM; Sue Kim, PharmD, BCPS
ICHP Poster Presentations – Encore #1
Winner: Best Encore Poster Presentation
2016
(presented as
Poster #20)
Category: Encore
Title: Implementation of decentralized pharmacy technicians to improve medication delivery and nursing satisfaction
Purpose: To assess the impact decentralized pharmacy technicians (DPTs) can have on the medication delivery process and on nursing satisfaction with the pharmacy service
Methods: A two-week prospective study on one general medicine floor and two intensive care units was conducted between September and October 2015. One decentralized pharmacy technician was assigned to each of these locations Monday through Friday from 9:00 am to 5:30 pm to improve medication availability through timely communication with nursing staff regarding medication procurement issues. Each study floor served as its own control in that data pertinent to the study outcomes was collected in a two-week period preceding the intervention period. The number of medication requests sent to the central pharmacy and the number of medications that required physical pick-up by nurses during the intervention period and the control period were recorded. Nursing satisfaction was surveyed prior to the intervention period and immediately following the intervention period.
Results: Nursing workflow interruptions due to medication retrieval were decreased by 74%. Post-intervention, mean scores for each nursing satisfaction survey question were significantly higher than the pre-intervention period survey (P < 0.01 for all five questions). Electronic medication requests sent to central pharmacy did not decrease significantly, 463 and 453 requests were sent during the pre-intervention and intervention periods respectively.
Conclusion: The decentralized pharmacy technician model significantly reduced nursing workflow interruptions and improved nursing satisfaction.
Submitting Author: Whitnee Caldwell, PharmD
Submitting Organization: Northwestern Memorial Hospital
Authors: Whitnee Caldwell, PharmD; Bryan Shaw, PharmD; Fuwang Xu, PharmD; Noelle Chapman, PharmD; Ana Fernandez, CPhT
ICHP Poster Presentations – Encore #2
(presented as Poster #9)
Category: Encore
Title: Global Initiatives to Streamline Pharmacy Education and Workforce Development
Purpose: The FIP Education Initiatives and Pharmacy Education Taskforce developed the Global Competency Framework and the Global Quality Assurance Framework for pharmacy leadership organizations to provide strategic mapping tools for pharmacy education and workforce development. The main purpose of this study is to share educational tools that impact the pharmacy profession and empower educators, leaders, and practitioners to streamline competencies.
Methods: The educational experts describe national and global initiatives to best streamline Competencies for pharmacy education. Specifically, the experts highlight programs for pharmacy education and workforce development that have been successfully implemented and assessed to assure the quality of pharmacy education on the global level.
Results: A panel of experts of educators, regulators, and practitioners highlight the structure, process, and outcomes of global collaborations to improve the quality of pharmacy education. Specifically, the panel shares the results of a “SWOT” Analysis - Strengths, Weaknesses, Opportunities, and Threats - of streamlining pharmacy educational competencies. The panel also shares examples of pharmacy education and workforce development initiatives that were implemented to continuously improve the quality of pharmacy professional development programs. In addition, the presenters describe collaborations between national and international agencies and opportunities for future scientific contributions.
Conclusions: Global initiatives will enhance the quality of education for pharmacy students and practitioners and ultimately improve pharmacy practice.
Submitting Author: Abby A. Kahaleh, BPharm, MS, PhD, MPH
Submitting Organization: Roosevelt University College of Pharmacy
Authors: Abby A. Kahaleh, BPharm, MS, PhD, MPH; Mike Rouse, BPharm; Ian Bates, PhD-FIP; Andreia Bruno, PhD
ICHP Poster Presentations – Encore #3
(presented as Poster #18)
Category: Encore
Title: Antifungal prophylaxis consideration in patients being treated with blinatumomab for Philadelphia chromosome-negative relapsed or refractory b-cell acute lymphoblastic leukemia: a case report
Purpose: The purpose of this case is to illustrate why antifungal prophylaxis should be considered for patients being treated with blinatumomab for Philadelphia chromosome-negative relapsed or refractory B-cell acute lymphoblastic leukemia (ALL). Based on the National Comprehensive Cancer Network (NCCN) guidelines, consideration of antibacterial, antiviral, and antifungal prophylaxis should be considered for ALL patients being treated with chemotherapy. In this case, AL, a 24-year-old female, upon first diagnosis of B-cell acute lymphoblastic leukemia, was initiated on induction chemotherapy with Cancer and Leukemia Group B (CALGB) 10403 protocol. After four cycles, a bone marrow biopsy was performed and her results were consistent with remission. Two months later, during a routine follow-up visit, AL was noted to have worsening pancytopenia. Her bone marrow biopsy results were consistent with relapsed B-cell ALL involving 80% of the marrow space. The patient was then admitted to the hospital to begin re-induction therapy with newly approved blinatumomab. Blinatumomab is a novel agent that activates T cells by binding to both CD19 expressed on B cells and CD3 expressed on T cells, which results in lysis of the CD19 cells. It is recommended that the first 9 days of the first cycle be administered in the hospital to monitor for cytokine release syndrome (CRS). In addition to CRS, other side effects include neurological toxicities, infections, and elevated liver enzymes. As part of her supportive care regimen, AL continued acyclovir for antiviral prophylaxis and was initiated on levofloxacin for antibacterial prophylaxis. Due to patient’s pancytopenia, antifungal prophylaxis with an azole antifungal was considered, but due to concern for elevated liver enzymes reported with both blinatumomab and azole antifungals, antifungal prophylaxis was held. AL received the first 9 days of blinatumomab induction therapy inpatient as recommended to monitor for CRS. AL tolerated treatment without any issues and was discharged from the hospital to continue the remainder of blinatumomab therapy at home. One month after the initial induction of blinatumomab, AL was admitted to the emergency department with abdominal pain and headache. AL was afebrile upon admission and blood cultures were obtained. Blood culture results revealed growth of budding yeasts, which was later identified as candida krusei. AL began treatment with micafungin and blinatumomab therapy was discontinued. An infectious disease (ID) team was consulted and due to persistently positive cultures for budding yeast, AL’s central line was removed. Cultures of the line were negative. In addition, a transesophageal echocardiogram was obtained, which was negative for valvular vegetation. After five days of failed treatment with micafungin, persistent fever and now newly hypotensive, AL was transitioned to liposomal amphotericin and flucytosine per ID’s recommendations and also transferred to the medical intensive care unit (MICU) for sepsis. The following day, AL went into respiratory distress and was intubated. Two days after, liposomal amphotericin and flucytosine was discontinued and voriconazole was initiated. Cultures remained positive for 13 days with fungemia. Given the progressive decline in her condition and poor prognosis, she expired 21 days from when she was transferred to the MICU. As with any new cancer drug, supportive care treatment is not well defined. Although more experience is needed to draw a definitive conclusion, the purpose of this case report is to share our experience and generate discussion about the need for antifungal prophylaxis, and if so which antifungal agent, in patients receiving blinatumomab therapy.
Methods: N/A
Results: N/A
Conclusion: N/A
Submitting Author: Margaret Lee, PharmD Candidate
Submitting Organization: Midwestern University Chicago College of Pharmacy
Authors: Margaret Lee, PharmD Candidate; Lisa M. DiGrazia, PharmD, BCPS, BCOP; Amanda N. Seddon, PharmD, BCPS, BCOPr
ICHP Poster Presentations – Encore #4
(listed in Syllabus as
Poster #19)
Category: Encore
Title: Differences in Clostridium difficile infection outcomes between guideline concordant and discordant therapy
Poster not presented.
ICHP Poster Presentations – Student #1
(presented as Poster #22)
Category: Student - Research Complete
Title: Assessment of healthcare needs of elderly patients in rural communities of central Illinois
Purpose: To complete an assessment of elderly care to reduce costs, increase quality and access to medical care among patients living in rural Illinois counties.
Methods: A literature review was conducted by the researchers to assess the quality, cost, and access to care among elderly living in rural Illinois. A Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis was conducted to evaluate the feasibility of the project. Search engines, including PubMed and Medline were used for the most currents findings, using relevant subject headings. Comprehensive search strategies were used within the intrinsic limits of each resource. The results were reviewed to select literature for inclusion criteria.
Results: Results of the literature reviews revealed 40 sources from which 17 were utilized. National statistics showed that 20% of the US population lives in rural America, but only 15% of nurses, 12% of pharmacists, and 9% of physicians practice in rural settings. Currently, lack of access to healthcare providers for rural patients has been reported to be the biggest barrier, 31 % were lacking transportation and 37 percent missed their appointments due to transportation issues. Medicare Advantage plan has a high star rating, which is in line for bonus payments from Centers for Medicare and Medicaid Services (CMS). These bonus payments reflect reward for good performance, improved patient outcomes, and health care savings by the plan. In Illinois, Peoria county consists of 187,000 residents, which is the target county in this study. Research indicates that rural elderly residents are more likely to go without needed care. This increases their total out-of-pocket medical costs due to future hospital or specialty care (40% versus 33% of urban patient healthcare costs). This proposal would provide patients with personalized healthcare in the comfort of their own home. The healthcare professional team can provide educational programs at local city centers. These interprofessional teams offer general medical needs, such as blood glucose screenings, medication therapy reviews, and patient counseling.
Conclusions: Interprofessional teams, composed of physicians, pharmacists, nurses and social workers will provide care to elderly patients to reduce costs, increase quality, and improve access to healthcare services. This proposed model will reduce out-of-pocket cost for patients in Peoria by eliminating unnecessary direct and indirect medical costs. This model will optimize individual health care, improve quality of life for patients by providing care at home, and increase patient adherence. Ultimately, providing home care will enhance access to healthcare services amongst elderly patients in Peoria.
Submitting Author: Katarzyna Plis, PharmD Candidate
Submitting Organization: Roosevelt University College of Pharmacy
Authors: Katarzyna Plis, PharmD Candidate; Danielle Cilano, PharmD Candidate; Sarah Bay, PharmD Candidate; Rimple Patel, PharmD Candidate; Abby Kahaleh, BPharm, MS, PhD, MPH
ICHP Poster Presentations – Student #2
(presented as Poster #21)
Category: Student - Research Complete
Title: Effectiveness of Pharmacy Practice Model Initiative Competency
Purpose: The Pharmacy Practice Model Initiative (PPMI) is a national initiative started by the American Society of Health-Systems Pharmacists (ASHP) in 2008 to encourage the most effective use of pharmacists allowing for overall advancement in patient care. PPMI is currently referred to as the Pharmacy Advancement Initiative (PAI) by ASHP; this change was made after the conclusion of the study.
With regards to pharmacy education, there is a lack of literature discussing PPMI/PAI. Such literature would be beneficial for schools of pharmacy in order to assess the best approach to teaching students regarding PPMI. Education of pharmacy students regarding PPMI and the professional goals of advancing patient care can impact healthcare reform and encourage them to advocate for patient care at all stages in their career.
In 2013, Pharmacy Practice Model Initiative (PPMI) components were incorporated into Southern Illinois University Edwardsville School of Pharmacy's curriculum. Students partook in an educational activity to learn more about PPMI during their Advanced Pharmacy Practice Experience (APPE) preparatory course in their 3rd year. Additionally, a competency requirement on PPMI was developed for students to complete during their Hospital APPE. This study’s primary objective is to determine the effect of the PPMI competency on students’ understanding and discussion of PPMI during their Hospital APPE. The expected outcome was that the mean score for the total number of students would be a 6 or above (indicating an average to moderate understanding of PPMI).
Methods: A survey of SIUE preceptors who taught hospital APPE rotations was determined to be the most practical approach to obtaining the necessary information regarding student knowledge base of PPMI. A survey was created consisting of primarily short answer questions and yes/no options. The 20 question survey collected the following information: hospital and preceptor demographics, staffing model, staff training, automation/technology systems, pharmacy involvement in PPMI initiatives, and student understanding and discussion of PPMI during the rotation. For the questions regarding student understanding of PPMI, preceptors were asked to rank student knowledge from 0 to 10 (0 indicating did not meet expectations and 10 indicating exceeded expectations). The scoring of students was based on the discussion of PPMI knowledge and was not based on whether or not changes to the institution were implemented.
Inclusion criteria were: Illinois or Missouri SIUE preceptors, taught ≥ 6 hospital APPE students for the academic school year, and agreed to the interview. Exclusion criteria included: those who did not respond or complete the interview. Only one preceptor was selected from each hospital site. Seven preceptors were selected based on the criteria that were eligible to partake in the survey and were subsequently contacted. Preceptors who taught from May 2013-May 2014 were selected to participate.
Results: Six out of the seven preceptors contacted responded and completed the interview. All preceptors interviewed answered every question on the survey. When asked about the average baseline knowledge of their SIUE Hospital APPE rotation students with regards to PPMI on a numerical scale, the responses ranged from 4 to 8.5 (mean ± S.D., 6.4±1.65).When asked about the impact of PPMI within the hospital after discussion with SIUE APPE hospital students, 5 out of 6 preceptors stated that no changes were made based on these discussions. One preceptor noted that three specific ideas for implementing the goals of PPMI were initiated by SIUE APPE students during their hospital rotation. These ideas included: technicians checking the work of other technicians (tech-check-tech), pharmacists managing insulin titrations until physician champion is set, and medication reconciliation done by pharmacy technicians. Another preceptor stated that since there were no changes implemented after student discussions within the 2013-2014 school year, the site decided to adjust the discussion of PPMI to include students filling out the ASHP hospital PPMI survey which allows hospitals to see how well they are doing in terms of implementing PPMI goals.
Conclusions: Based on the study results, the PPMI competency met the expected outcomes of the study. The study showed that the majority of students had an average to moderate understanding of PPMI according to their preceptors. One significant limitation to the study is the number of preceptors interviewed. Future directions could include performing the study with a larger sample size, studying the long term impact of student discussion on PAI a few years after the rotations, and surveying alumni to see how/if the competency impacted their own practice of pharmacy.
Submitting Author: Saba Mohiuddin, PharmD candidate
Submitting Organization: Southern Illinois University Edwardsville School of Pharmacy
Authors: Saba Mohiuddin, PharmD candidate; Lisa Lubsch, PharmD, AE-C; Jinyang Fan, PharmD, BCPS
ICHP Poster Presentations – Student #3
(presented as Poster #24)
Category: Student - Research in Progress
Title: Desmopressin (DDAVP) Dose Changes Post Discharge in Pediatric Patients with Diabetes Insipidus Receiving Oral DDAVP Compounded from Nasal Spray Inpatient
Purpose: The purpose of this study is to evaluate desmopressin (DDAVP) dose changes among diabetes insipidus (DI) pediatric patients receiving oral DDAVP solution formulated using DDAVP nasal spray. DDAVP is not commercially available as an oral liquid in the United States.1 This is problematic for pediatric patients unable to swallow whole tablets. Consequently, many caregivers must resort to extemporaneously compounding a DDAVP solution prior to immediate use. Comparing the effect of both formulations, oral tablets and solution compounded from tablets, on decreasing urine volume and increasing urine osmolality have produced equivalent results.2 However, many institutions utilize a compounding recipe that uses desmopressin nasal spray to produce an oral solution that has a 30 day shelf life.3 Following the inpatient administration of this formulation, however, the Pediatric Endocrinology service at the University of Chicago observed that preadmission desmopressin doses were no longer adequate post discharge.
Methods: This single center retrospective study evaluated the medical records of pediatric patients who received DDAVP oral solution compounded from DDAVP nasal spray. The observation period took place between January 1, 2013 and August 7, 2015. Only patients who received oral desmopressin before admission and after discharge were included in the study. Additionally, a two-month refill history of oral desmopressin tablets with instructions for extemporaneous compounding before and after discharge was required. Patients undergoing neurosurgical procedures and displaying acute renal impairment were excluded. Doses were then tabulated and analyzed using descriptive statistics.
Results: Research in Progress
References
1. Desmopressin. Micromedex 2.0. Truven Health Analytics, Inc. Greenwood Village, CO. Available at:
http://www.micromedexsolutions.com.
Accessed December 20, 2015.
2. Argenti D, Ireland D, & Heald DL. A pharmacokinetic and pharmacodynamics
comparison of desmopressin administered as whole, chewed, and crushed tablets,
and as an oral solution. J Urol. 2001;165(5):1446-51.
3. Michigan Pediatric Safety Collaboration to Standardize Compounded Oral
Liquids. University of Michigan College of Pharmacy. Available at:
http://www.mipedscompounds.org. Accessed
December 21, 2015.
Conclusions: Research in Progress
Submitting Author: Gennaro Anthony Paolella, BS Pharmacy Student
Submitting Organization: University of Chicago
Authors: Gennaro Anthony Paolella, BS Pharmacy Student; Shannon Rotolo, PharmD, BCPS
ICHP Poster Presentations – Student #4
Winner: Best Student Poster Presentation
2016
(presented as
Poster #12)
Category: Student - Research in Progress
Title: Retrospective analysis of osteoporosis risk factors among the Chinese population
Purpose: Assess effects of weight, cigarette smoking, and alcohol intake, on bone mineral density, measured as T-score, among the Chinese population in Chicago’s Chinatown neighborhood. -Determine if length of stay in the US has any impact on BMD.
Methods: A retrospective analysis will be conducted using data collected at Midwest Asian Health Association (MAHA) in Chicago’s Chinatown neighborhood from August 2013 to August 2015. Data from 200 participants will be reviewed. MAHA, located in Chicago, is a community-based, non-profit 501 (c)(3) organization that provides community outreach education, screenings, immunizations and linkage to care in collaboration with community-based organizations, health care providers and academic institutions to reduce health disparities for the Asian population. The majority of the health fair attendees lack or have limited health insurance. For the last two years, pharmacy school students from Chicago State University College of Pharmacy have partnered with MAHA to offer free bone mineral density screening during MAHA’s monthly health fair. During these events, MAHA collected demographic information of each participant as part of their record keeping in order to properly assess the participants’ risk of osteoporosis. These demographic information include age, sex, height weight, social and family history. Bone health-bone density screenings were offered to men and women aged 20 years and older using the Lunar AchilllesTMQuantitative Ultrasound System provided by the College of Pharmacy at Chicago State University. All participants signed a consent form to be part of the health screenings. Descriptive analysis will be used to report demographic and fracture risk factors. A correlation analysis will be used to describe the relationship between length of stay in the US, weight, smoking status, and alcohol consumption and BMD.
Results: Research in Progress
Conclusion: Research in Progress
Submitting Author: Anna Aidonis, PharmD candidate
Submitting Organization: Chicago State University College of Pharmacy
Authors: Anna Aidonis, PharmD candidate; Cindy Leslie A. Roberson, PharmD, BCACP; Hemangini Shah, PharmD Candidate
ICHP Poster Presentations – Student #5
(presented as Poster #23)
Category: Student - Research in Progress
Title: Comparison of oral morphine equivalent doses vs. PHQ9 scores in a family practice setting
Purpose: Determine if a pharmacist is able to decrease opioid use without worsening PHQ9 scores.
Methods: This retrospective chart review evaluates a sample size of 271 patients receiving pain management by a pharmacist in a family practice setting in southern Illinois. The primary outcome is to determine if decreasing oral morphine equivalent doses increases PHQ9 scores. Opioid use (measured by the oral morphine dose) and depression (measured by PHQ9 scores) were calculated for each patient visit and compared over a two year time frame.
Results: Research in Progress
Conclusions: Research in Progress
Submitting Author: Lauren Ashley Kirkpatrick, PharmD candidate
Submitting Organization: Southern Illinois University Edwardsville
Authors: Lauren Ashley Kirkpatrick, PharmD candidate; Chris Herndon, PharmD, BCPS, CPE, FASHP
ICHP Poster Presentations – Student #6
(presented as Poster #11)
Category: Student - Research in Progress
Title: Phytopharmacological evaluation of chamomile (Matricaria recutita L.) for indirect modulation of the endocannabinoid system
Purpose: German chamomile (Matricaria recutita L.) has been known to be a useful antidepressant and anxiolytic in humans. Clinical trials demonstrate the role of the endocannabinoid system in modulating emotional homeostasis. The objective of our research was to identify compounds in chamomile that indirectly modulate the endocannabinoid system through inhibition of the endocannabinoid catabolizing enzymes, fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL). The identification of compound(s) interacting with the endocannabinoid system will provide lead compounds with therapeutic potential against various mood disorders.
Methods: A bioassay-guided fractionation approach was adopted. Whereas chamomile powder was initially extracted with methanol followed by fractionation with hexane, chloroform, ethyl acetate, and methanol. All fractions were fingerprinted using high performance liquid chromatography. The fractions were evaluated for FAAH inhibition using an in vitro microplate assay. In the initial screening, the hexane showed the highest activity. The fraction was further subjected to bioassay-guided chromatography until a pure active compound was isolated and identified. All fractions were also evaluated for inhibition of the MAGL enzyme.
Results: Research in progress. Throughout our experiments, we were able to identify one active compound, linoleic acid. Our current and future research aim at identifying the remainder of compounds and their evaluation in animal models.
Conclusions: Though our research is still in progress, our experiments demonstrate a procedure that can be replicated for any other herbs of interest. We are still in an early phase of our chamomile project, and many active compounds are yet to be isolated and identified. However, we were able to reliably demonstrate FAAH and MAGL inhibition activity, which show that chamomile has a role in modulating the endocannabinoid system and supports its use as an herbal dietary supplement for depression and anxiety.
Submitting Author: Kristine Manlimos, PharmD Candidate
Organization: Chicago State University College of Pharmacy
Authors: Kristine Manlimos, PharmD Candidate; Nidhi Patel, PharmD Candidate; Ehab Abourashed, MS, PhD; Abir El-Alfy, MS, PhD, PharmD Candidate
ICHP Poster Presentations – Student #7
(listed in Syllabus as
Poster #10)
Category: Student - Research in Progress
Title: Comparison of Pharmacist and Physician Attitudes and Knowledge of Pain Management
Poster not presented.
ICHPeople
 Congratulations to Sister Mary Louise Degenhart, who received ASHP's 2016 Harvey A.K. Whitney Lecture Award.
Congratulations to Sister Mary Louise Degenhart, who received ASHP's 2016 Harvey A.K. Whitney Lecture Award.College Connections
Midwestern University Chicago College of Pharmacy
IFN Interprofessional Event
by Aisha Alsliman, PS2, ICHP Philanthropy Chair, Midwestern University Chicago College of Pharmacy



Roosevelt University College of Pharmacy
Providing Tools for Success of First-Year Pharmacy Students in a Three-Year Program
by Cony Hartnett, PS3, SSHP Webmaster/Historian; Camille Andrews, PS3, SSHP Treasurer; Jordan Faison, PS3, SSHP President
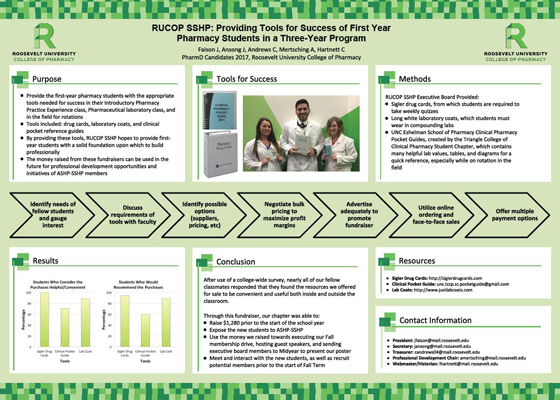
More
Welcome New Members!

| New Member | Recruiter |
| Sara Abdulrasoul | |
| Mona Adhami | |
| Josephine Adutwumwaa | |
| Gabriel Ahiamadi | |
| Fahad Ahmed | |
| Benish Alam | |
| Shazia Alavi | |
| Saniya Ali | |
| Reem Alsultan | |
| Elnaz Arabian | |
| Megan Asher | |
| Asma Awad | |
| Elizabeth Awoyemi | |
| Mark Badria | |
| Mohammed Baig | |
| Jori Bailey | |
| Sarah Banday | |
| Ellecia Bernard | Jordan Faison |
| Sharril Boda | |
| Ryan Bonomo | Oliver Smith |
| Olivia Brandner | |
| Rob Braylock | |
| Sarah Brockhouse | Garry Moreland |
| Francisco Castaneda | |
| Elena Cheptene | Florence Patino |
| Jessi Cramer | Linda Fred |
| Joseph Desantis | |
| Krystal Earle | |
| April Estes | Linda Fred |
| Meta Jo Floyd | |
| Juliet Franklin | |
| Britrice Goins | |
| Anna Gracheva | |
| Andrew Grigus | |
| Jatin Gumpella | |
| Alexander Heinz | |
| Cynthia Hidden | Tobi Sondag |
| Shirley Huang | |
| Soheileh Hwang | |
| Jiji Isaac | |
| Christina Jacob | |
| Brent Jamison | |
| Carlos Jara-Garate | |
| Simon Lam | |
| Vanessa Leon | |
| Angelique Lintz | Trevor Luman |
| Sarah Lynch | |
| Dezaray McDonald | |
| Ariel McDuffie | |
| Dana Mdanat | |
| Anna Michalec | |
| Lauren Nail | |
| Hannah Nelson | Linda Fred |
| Jennifer Oetgen | |
| Bintu Ogundimu | |
| Ozren Orlovic | |
| Duaa Oshaik | |
| Kevin Park | |
| Ravi Patel | |
| Hetal Patel | |
| Nidhi Patel | |
| Priyanka Patel | |
| Robert Pecho | |
| Kimberly Peterson | Ina Henderson |
| Suzanne Pihlstrom | |
| Sree Prathipati | |
| Damaris Quagrainie | |
| Therese Quijano | |
| Farheen Quraishi | Tamkeen Quraishi Abreu |
| Courtney Reed | Linda Fred |
| Kylie Reikowski | |
| Nichole Reiten | |
| Quratulain Sabir | |
| Ayesha Saleem | |
| Steven Sessions | David Silva |
| Mohammed Sikder | |
| Nichelle Simpkins | |
| Jennifer Sotto | |
| Mark Spitzer | |
| Malia Stark | Linda Fred |
| Steve Tancredi | Nadia Tancredi |
| Jamie Thomas | |
| Aaric Thompson | |
| Rita Tonino | |
| My Trang | |
| Tanya Uddin | |
| Jami Weiland | Trevor Luman |
| Nikki Wilson | |
| Ryan Wilson | |
| Jeremy Wilson | |
| Jasmine Woods | |
| Anne Yeglic |
Officers and Board of Directors
linda.fred@carle.com
Treasurer
815-599-6113
mweaver@fhn.org
TRAVIS HUNERDOSSE
Director, Educational Affairs
thunerdo@nmh.org
DESI KOTIS
Director, Professional Affairs
dkotis@nmh.org
ANN JANKIEWICZ
Chairman, House of Delegates
DAVID TJHIO
Chairman, Committee on Technology
816-885-4649
david.tjhio@cerner.com
JACOB GETTIG
Editor & Chairman, KeePosted Committee
630-515-7324 fax: 630-515-6958
jgetti@midwestern.edu
Assistant Editor, KeePosted
630-515-7167
jphillips@midwestern.edu
Executive Vice President, ICHP Office
815-227-9292
scottm@ichpnet.org
Regional Director North
Co-Regional Director South
Co-Regional Director South
President, Student Chapter
University of IL C.O.P.
ksenci2@uic.edu
President, Rockford Student Chapter
University of IL C.O.P.
cha17@uic.edu
JESSICA PENG
President, Student Chapter
jpeng54@midwestern.edu
BRITTANY HUFF
President, Student Chapter
Chicago State University C.O.P.
WHITNEY MAHER
President, Student Chapter
Southern Illinois University Edwardsville S.O.P
whitney.maher@gmail.com
JORDAN FAISON
President, Student Chapter
Roosevelt University C.O.P.
VALENTIN PACURARU
President, Student Chapter
Rosalind Franklin University C.O.P.
valentin.pacararu@my.rfums.org
ICHP Affiliates
KATHRYN SCHULTZ
President, Northern IL Society (NISHP)
JARED SHELEY
President, Metro East Society (MESHP)
AMY BOBLITT
President, Sangamiss Society
ED RAINVILLE
President, West Central Society (WSHP)
ed.c.rainville@osfhealthcare.org
Vacant Roles at Affiliates —
President, Rock Valley Society; Southern IL Society; Sugar Creek Society
ICHP Pharmacy Action Fund (PAC) Contributors
Ronald Miller