Official Newsjournal of the Illinois Council of Health-System Pharmacists

November 2021
Volume 47 Issue 4
Features
Change is an Opportunity, not an Enemy: Highlights of the Alliance Conference
History of Organized Hospital Pharmacy in Illinois: The Early Years
Do You Like to Run? How About Out in Front?
Do You Know a Great Pharmacist?
ICHP Best Practice Award Program
Columns
College Connections
Celebrating Poison Prevention Month
The Importance of Quality in Saving the Lives of Crickets Everywhere
Brown Bag Medication Review – An Overview and Planning Guide
Lung Health Booth at St. Bridget’s Food Pantry
More
Officers and Board of Directors
ICHP PHARMACY ACTION FUND (PAC) Contributors
KeePosted Info

Illinois Council of Health-System Pharmacists
4055 North Perryville Road
Loves Park, IL 61111-8653
Phone: (815) 227-9292
Fax: (815) 227-9294
www.ichpnet.org
KeePosted
Official Newsjournal of the Illinois Council of Health-System Pharmacists
EDITOR
Jacob Gettig
ASSISTANT EDITOR
Jennifer Phillips
MANAGING EDITOR
Scott Meyers
ASSISTANT MANAGING EDITOR
Trish Wegner
DESIGN EDITOR
Amanda Wolff
ICHP Staff
EXECUTIVE VICE PRESIDENT
Scott Meyers
VICE PRESIDENT - PROFESSIONAL SERVICES
Trish Wegner
DIRECTOR OF OPERATIONS
Maggie Allen
INFORMATION SPECIALIST
Heidi Sunday
CUSTOMER SERVICE AND
PHARMACY TECH TOPICS™ SPECIALIST
Jo Ann Haley
ACCOUNTANT
Jan Mark
COMMUNICATIONS MANAGER
Amanda Wolff
LEGISLATIVE CONSULTANT
Jim Owen
ICHP Mission Statement
Advancing Excellence in the Practice of Pharmacy
ICHP Vision Statement
ICHP dedicates itself to achieving a vision of pharmacy practice where:
• Pharmacists are universally recognized as health care professionals and essential providers of health care services.
• Patients are aware of the training, skills, and abilities of a pharmacist and the fundamental role that pharmacists play in optimizing medication therapy.
• Formally educated, appropriately trained, and PTCB certified pharmacy technicians manage the medication distribution process with appropriate pharmacist oversight.
• Pharmacists improve patient care and medication safety through the development of effective public policies by interacting and collaborating with patients, other health care professionals and their respective professional societies, government agencies, employers and other concerned parties.
• Evidence-based practices are used to achieve safe and effective medication therapies.
• There are an adequate number of qualified pharmacy leaders within the pharmacy profession.
• Pharmacists take primary responsibility for educating pharmacy technicians, pharmacy students, pharmacist peers, other health professionals, and patients about appropriate medication use.
KeePosted Vision
As an integral publication of the Illinois Council of Health-System Pharmacists, the KeePosted newsjournal will reflect its mission and goals. In conjunction with those goals, KeePosted will provide timely information that meets the changing professional and personal needs of Illinois pharmacists and technicians, and maintain high publication standards.
KeePosted is an official publication of, and is copyrighted by, the Illinois Council of Health-System Pharmacists (ICHP). KeePosted is published 10 times a year. ICHP members received KeePosted as a member benefit. All articles published herein represent the opinions of the authors and do not reflect the policy of the ICHP or the authors’ institutions unless specified. Advertising inquiries can be directed to ICHP office at the address listed above. Image disclaimer: The image used in the Pharmacy Tech Topics advertisement is the property of © 2013 Thinkstock, a division of Getty Images.
Copyright © 2013, Illinois Council of Health-System Pharmacists. All rights reserved.
Features
Change is an Opportunity, not an Enemy: Highlights of the Alliance Conference
by Maggie DiMarco Allen, PhD, ICHP Director of Operations
Collaboration and partnering are becoming essential in the world of continuing education – for all the health professions. The shrinking pool of education grants and sponsorships affects all the healthcare continuing education providers, while the need for excellent programming grows as a means of countering medication errors and improving patient safety outcomes. In response, the national Alliance for Continuing Medical Education (ACME) changed its focus and vision, and opened its membership to include all healthcare disciplines. Re-branded as the Alliance for Continuing Education in the Health Professions, this re-defined focus attracted CE professionals from the medical, nursing and pharmacy communities this past January 30-February 2, 2013 to the 38th Annual Conference of the Alliance in San Francisco.
I was fortunate to attend this meeting as ICHP’s representative and a new member of the Alliance. ICHP takes great pride in the quality of our continuing pharmacy education programs. We view this member benefit as a key component in fulfilling our vision of advancing excellence in the practice of pharmacy.
The conference’s opening keynote by Ed O’Neil, PhD, MPA, FAAN, set an important tone with a very straightforward message – change is going to happen whether we like it or not, so “get over it!” The health professions and we, as CE providers, need to position ourselves for strategic success – this means NOT resisting change – rather, understanding it and positioning oneself and one’s organization for change.
O’Neil outlined three main drivers of this inevitable change:
- US healthcare costs too much
- The quality of US healthcare is dropping
- Consumer satisfaction is extremely low
In a humorous, yet very pointed comparison, O’Neil likened the US Healthcare system to the Hummer vehicle – a vehicle described as expensive, overbuilt and underperforming. He said we have four options:
- Drive less – ration use, since can’t afford it, so limit access to it (e.g. insurance).
- Shift the cost – from hospital to insurance to patient.
- Pay less for it through use of controls – everyone takes a 40% pay cut – but that will NOT happen.
- Build a NEW CHASSIS – requires the willingness and ability to think differently about the problem!
Being open to a new way of seeing and thinking about our problems is essential. The challenge for CE providers during the next 15 years, which is how long O’Neil believes it will take our country and our systems to adapt to and modify the Affordable Care Act so it is a fully operational part of the healthcare system, is to disrupt the beloved patterns of how it has been done, and show that a shifting healthcare paradigm is not the end of the world. This conference opener left us all with a lot to think about as we proceeded to split up and attend the various sessions of interest.
We reviewed the old lecture / memorization / recitation and Flexnerian1 model of education and the growing movement toward team-based education, the United States’ standing in comparison to global healthcare, and the need for deep empathy among healthcare professionals when interacting with patients. We explored the impact of technology, marketing, and education design on our CE programs, as well as the need for continuing professional development, for both healthcare and CE providers.
Mixing it up with the corporate grant providers in attendance, we also explored the precarious state of commercial grants for CE funding. Grant making departments are likewise feeling the economic pinch as the funding previously provided by their respective companies is being diverted to other areas. Our CE programming needs to include interactive components as well as outcomes reflecting follow-up, to verify the impact of the CE on patient safety and work site quality improvements. We reviewed ways and means to develop CE formats and follow-up reports that reflect clear needs and gap analysis, and a clear indication that our CPE programming affects and changes the process – improving pharmacist / technician / patient communication and outcomes. Without these needs assessments and outcome reports, grant providers are finding it more difficult to justify the continuation of CE funding.
Members who attend our annual and spring meetings may have noticed how ICHP has been working with our speakers to create programming that includes interactive components with our Audience Response System, more Q and A, pre-test, post-test, etc. We will be developing select follow-up surveys as well to help us document the value of our CPE to ourselves, our members, and potential grant providers. You also will receive an ICHP Needs Assessment email within the next month – something we do every two years – asking for your feedback on what are the most important CPE topics for you.
Overall, the Alliance conference was both inspiring and educational, providing new perspectives on the value of continuing education in healthcare, new ideas for improving our educational formats and grant requests, and some thoughtful encouragement on personal growth.
I would like to end with an interesting closing excerpt which Dr. O’Neil used as a reminder to us all to never stop questioning the underlying reasons for why we do what we do.
THE MYTH OF SISYPHUS
We tend to think of Sisyphus as a tragic hero, condemned by the gods to shoulder his rock sweatily up the mountain, and again up the mountain, forever.
The truth is that Sisyphus is in love with the rock. He cherishes every roughness and every ounce of it. He talks to it, sings to it. It has become the mysterious Other. He even dreams of it as he sleepwalks upward. Life is unimaginable without it, looming always above him like a huge gray moon.
He doesn’t realize that at any moment he is permitted to step aside, let the rock hurtle to the bottom, and go home.
Tragedy is the inertial force of the mind.
- Stephen Mitchell in Parables and Portraits
1 Abraham Flexner, author of the Flexner Report published in 1910, used to reform medical education.
History of Organized Hospital Pharmacy in Illinois: The Early Years
In this month’s issue, the early history of hospital pharmacy organizations is summarized. The first part of the article was written by Elvera H. Dressler, the first president of ICHP’s earliest predecessor – the Hospital Pharmacists of Chicagoland, but the part of the history from 1947 on was prepared by an unknown writer.
History of Illinois Society of Hospital Pharmacists
For many months during the year 1940, the pharmacists at St. Francis Hospital, Evanston, Illinois, namely Sr. M. Alphonsa, Florence Baker Carmody, and Elvera H. Dressler discussed the merits of having an organization composed of hospital pharmacists in the Chicago area. Finally in April 1941 they decided to make their idea known to others in their field, and they sent out invitations to about 90 hospital pharmacies within a 50-mile radius of Chicago to attend an “Open House” and meeting to be held on a Sunday afternoon at St. Francis Hospital. About 70 of those invited responded and attended. After a general tour of the hospital, a meeting was held and Mrs. Dressler presented the idea of organization to the group. The purposes of such an organization were presented as follows:
- To promote the science and art of hospital pharmacy
- To promote the betterment of the working conditions and remuneration of the hospital pharmacists
- To promote a better professional relationship between the physician and the pharmacist
- To cooperate with national and state organizations should there be any having the same ideals, purposes and problems
- To discuss mutual problems
The group organized then and there and chose the name of “Hospital Pharmacists of Chicagoland.” Mrs. Elvera H. Dressler was elected the President of the group.
Meetings were held each month at the different hospitals during the first year. This proved successful in that comparisons, exchange of ideas, and discussions of mutual problems between the members was natural on these visits. Many good scientific speakers and/or films were also obtained, which added to the interests of the group. After the rounds of the hospitals had been made, it was decided to hold our meetings at the University of Illinois College of Pharmacy on the same evening that the American Pharmaceutical Association held their meetings so that members could attend both meetings on one evening. This arrangement was not too satisfactory as it would often be necessary to cut our meeting short so as not to delay the APhA meeting.
Our next move was to the Hospital Council Meeting Rooms in the Bankers Building in Chicago. This place soon became too small for the group and there were no accommodations for refreshments to be served there, so it was necessary to move again. We then met in the St. Clair Hotel in Chicago. The membership had grown considerably and changed somewhat. Hospital pharmacists or clinic pharmacists are active members, but we also had quite a large associate membership composed of drug manufacturers’ representatives and a few community pharmacists.
In 1947 the Chicago group affiliated with the national group and became known as the Illinois Chapter of the American Society of Hospital Pharmacists or the Illinois Society of Hospital Pharmacists.
ISHP carried on a rather comprehensive and extensive program with several types of activities involved. The principal project during the 1950s was a continuous and sustained effort to inform hospital pharmacists of new advances in science and new ideas in hospital pharmacy procedures. Most of the meetings made this project their main objective.
The Society, of course, carried on a regular program of meetings since its beginning. Usually eight meetings a year were held in hospitals, and the people who attended benefited by seeing other hospital facilities and learning something about how things were done there. Some meetings were held in hotels, sponsored by pharmaceutical companies.
In addition, the Society held or helped with several special types of meetings. One type had been annual one-day seminars for hospital pharmacists, beginning in 1958. They were conducted by the Society in cooperation with the Midwest Association of Sister Pharmacists. They were sponsored by the Chicago Hospital Association, and the University of Illinois College of Pharmacy.
The seminars were held at hotels or at the College of Pharmacy. They were well attended with 70-90 registrants. These included hospital pharmacists from such distant locations as Rockford, Joliet, Peoria, Decatur, and Springfield.
Another type of special meeting was participation of the Society in the hospital pharmacy programs of the Tri-State Hospital Assembly. Held over a period of two or three days annually in the spring, such programs were held for several decades. Members of this Society attended and participated actively. Beginning in 1959, the Society was invited to appear on the program as a “Participation Organization.”
The Society also helped with the Institutes on Hospital Pharmacy held by the American Hospital Association. When the Institutes were held in Chicago, usually once a year, the Society was given suitable publicity and held a reception for those attending. Many of the members of the Society served as instructors at the Institutes.
Another principal activity of the Society was helping hospital pharmacists to know each other better so that they could more readily get specialized advice on their problems. This was aided by the publication of the Society’s This publication was begun in the spring of 1956. While it began as the Bulletin, it was later called the Newsletter, and then received a new title, Keep Posted. For several years, beginning in the fall of 1956, this publication was printed and distributed for the Society by the Chicago Division of McKesson and Robbins and later by the AHA. While the bulletin’s principal purpose was to inform hospital pharmacists of this area of Society affairs, it carried some scientific notes, information on immunization for international travel, and other items of definite educational value.
Another project that helped hospital pharmacists know each other were meetings held outside Chicago or its immediate suburbs. The first such meeting was held November 10, 1959, at the Tinley Park State Hospital. The second meeting was an all afternoon program held at the Springfield Memorial Hospital in Springfield, Illinois, on November 19, 1960.
In addition to the above activities, which dealt particularly with hospital pharmacies and hospital pharmacists, the Society for many years cooperated with other pharmaceutical organizations in holding joint meetings. A long-standing event of this type was the annual May meetings of the Society held jointly with the Chicago Branch of the APhA and the University of Illinois Student Branch of the APhA.
A particular effort was made to hold special meetings especially designed for students in the College of Pharmacy. The Society, in cooperation with the University of Illinois College of Pharmacy, and with the approval of the Illinois Hospital Association and the Chicago Hospital Council, conducted an annual “Student Visitation Program” since 1958. The aim of this program was to introduce the junior pharmacy students to hospitals and, hopefully, to induce them to think of hospital pharmacy as a career. One must emphasize, though, that the primary goal of this program was to introduce this neophyte member of the health profession to a typical hospital and all of its complexities. As part of this program, the students, who were excused from classes for one afternoon for this visitation, were invited to attend the monthly meeting of the Society in the evening. The typical visitation program for the student was as follows:
- The students were greeted by the administrator of the hospital (or one of his assistants) who described, in 20 minutes or so, the philosophy of hospitals, some aspects on problems of administration, and some statistics about hospitals.
- The students met briefly with a member of the medical staff who discussed the physician-pharmacist relationship in the hospital and the role and responsibility of the physician in the hospital.
- The director of nursing service described the scope of the nursing department and the many divisions falling under the directorship of this department (student nurses, nurse aides, orderlies).
- During a coffee break, the director of the dietary department described the responsibilities of this department in feeding both the patient and the employee and the many types of diets required for the patients with different illnesses.
- At the end of the tour the students inspected the pharmacy department and the various aspects different from the practice of pharmacy in community stores.
In addition to the above wide variety of programs directed toward hospital pharmacists, other pharmacists, and pharmacy students, the Society sponsored activities to bring hospital pharmacists into contact with other individuals in the health sciences. This has been done in part through the Tri-State meetings and the hospital visitations referred to above.
Another great project that gave direct contact with other individuals in the health sciences was the manning of booths by members of the Society in the annual conventions of the AHA held in Chicago in 1957 and 1958. This project was specifically meant to show some aspects of the hospital pharmacy to hospital administrators. One feature was a model of a model pharmacy prepared by the U.S. Public Health Service. This was sponsored by the AHA and the ASHP.
To illustrate another function of the Society in this category, the Illinois Hospital Association asked the Society to appoint one of its members to represent the pharmacy department on the joint committee on paramedical services. This activity began in 1957. In addition to activities involving others in the medical sciences, a meeting was held in December 1959 in conjunction with the annual meeting of the American Association for the Advancement of Science in Chicago.
The Society also had a community service project beginning in 1956. Material was assembled and talks were presented on poison control and accidental poisoning in children. These talks were directed principally to the layman and given to such groups as the PTA, women’s groups, and radio audiences. A presentation of this topic was made at the Museum of Science and Industry in 1959 as a part of a Junior Chamber of Commerce Health Fair.
Do You Like to Run? How About Out in Front?
How Would You Like To Run For An ICHP Office?
by Scott A. Meyers, Executive Vice President
Every year, ICHP elects new members to its Board of Directors. As existing officers complete their terms, they often move up to higher offices or move on for a variety of reasons, not the least being that they’ve completed the highest offices of President-elect, President and Immediate Past President. So every year the ICHP Committee on Nominations searches for new leaders who are dedicated to “Advancing Excellence in the Practice of Pharmacy!” That’s ICHP’s mission by the way.
This year is no exception. With Chris Rivers completing her term as Immediate Past President and Ann Jankiewicz, and Jennifer Arnoldi completing their terms as Chair of the House of Delegates and Chair of the New Practitioners Network respectively, there are at least three offices that will need two candidates each to run. In addition, Board Members Carol Heunisch, Travis Hunerdosse, Jennifer Ellison, and Liz Engebretson can run for another term for their respective offices and may or may not have yet committed. And even if they do decide to run again, the Committee on Nominations will be seeking a second candidate to fill the ballot completely.
Below is a list of the offices open for election in the fall of 2013. All the elected candidates will take office at the 2014 Annual Meeting with the exception of the President-elect, who assumes office immediately. So each new leader will have almost a year to train for their new jobs and be coached by our current Board members. You don’t have to run that race unprepared!
- President-elect
- Secretary-elect
- Chair of the House
- Director-elect of Division of Educational Affairs
- Director-elect of the Division of Marketing Affairs
- Technician Representative-elect
- NPN Chair-elect
If you are interested in running for an office or you would like to know more about an office before committing to run, you may contact Committee on Nominations Chair, Chris Rivers at criversrx@gmail.com or Scott Meyers at scottm@ichpnet.org. We hope you are ready to run to the lead of ICHP and Pharmacy!
Do You Know a Great Pharmacist?
ICHP Pharmacist of the Year Nominees Sought
by Scott A. Meyers, Executive Director
ICHP is looking for the best of the best for this year’s Pharmacist of the Year Award Recipient! You should recognize some of the previous years’ winners as they have been pharmacy leaders in Illinois and nationally: Stan Kent, Kevin Colgan, Andy Donnelly, Miriam Mobley-Smith, Mary Lee and so many more! One of the earliest recipients of Illinois health-system pharmacy’s highest award, Herb Carlin, served as President of both ASHP and APhA. This is a feat that has been done by only a select few!
The ICHP Pharmacist of the Year recognizes a pharmacist who has worked in or around health-system pharmacy making substantial and sustained contributions to health-system practice or the profession in general. Below are the criteria for selection. Nominators should send a letter outlining the nominee’s accomplishments in detail to Trish Wegner (2013 Selection Committee Chair) at trishw@ichpnet.org or Scott Meyers at scottm@ichpnet.org.
Selection Criteria
The Illinois Health-System Pharmacist of the Year Award is given annually, if a recipient is chosen, to an individual of high moral character, good citizenship and high professional ideals, who has made significant contributions affecting the practice of health-system pharmacy throughout the state. These contributions shall have been in the form of sustained exemplary service in health-system pharmacy, or, a single outstanding achievement, or, a combination of accomplishments benefiting health-system pharmacy, and through it, humanity and the public health. They may include accomplishments, achievements or outstanding performance in:
- health-system pharmacy practice,
- health-system pharmacy education,
- health-system pharmacy administration,
- pharmaceutical research or development related to health-system pharmacy,
- pharmacy organizational activity with a definite relationship to health-system pharmacy,
- scientific or professional pharmaceutical writing, e.g., noteworthy articles on pharmaceutical subjects with applicability to health-system pharmacy,
- pharmaceutical journalism related to health-system pharmacy,
- public and/or interprofessional relations activities benefiting health-system pharmacy,
- pharmaceutical law or legislation, professional regulations, standards of professional conduct or pharmacy law enforcement as related to health-system pharmacy practice.
Past Recipients of ICHP’s Pharmacist of the Year Award
1966 F. Regis Kenna *
1967 Louis Gdalman *
1968 C. Charles Lev *
1969 Edward Hartshorn
1970 Herbert Carlin *
1971 Sr. Mary Louise (Matthew) Degenhart
1972 Harland E. Lee
1973 Roger Klotz
1974 Ronald Turnbull
1976 John Lewis
1977 Raphael Jacobson *
1978 Terry Trudeau *
1979 Merrikay Oleen
1980 Sr. Mary Margaret Wright
Ernie Steinbaugh **
1981 Karen Nordstrom
1982 Mary Maranti *
1983 E. Clyde Buchanan
1984 David Vogel *
1985 William Wuller
1986 LeRoy Hayes *
1987 Max L. (Mick) Hunt
1988 Marcia Palmer
1989 Lee S. Simon
1990 Edna Dooley
1991 Scott A. Meyers
1992 Kenneth Witte
1993 Kevin Colgan
1994 Alan Weinstein
1995 Edward Donnelly
1996 Bruce Dickerhofe
1997 Steven E. Marx
1998 Janet L. Teeters
1999 James Dorociak
2000 Robert Hoy
2001 Jacqueline Kessler
2002 Andrew Donnelly
2003 Mary Ann Kliethermes
2004 Michael Novario
2005 Miriam Mobley-Smith
2006 Jan Keresztes
2007 Avery Spunt
2008 Stan Kent
2009 Michael Fotis
2010 Mary Lee
2011 Michael Weaver
2012 Patricia Wegner
* deceased
** awarded posthumously
NPN Night at the Ballpark

CHICAGO CUBS vs. COLORADO ROCKIES
Wednesday, May 15
7:05 PM – 10:00 PM
Wrigley Field
Tickets are $6 (Yes, that’s the real price – for a Cubs game!)
Infield Terrace reserved seats
Now available on www.ichpnet.org!
All ICHP new practitioners, pharmacy residents, residency directors, and preceptors are welcome. Only ICHP members may attend and only one ticket per person may be purchased. Your credit card will be charged when you order.
Ticket sales are open through Wednesday, May 8 – after that date, all remaining tickets may be sold to an outside party.
ICHP Best Practice Award Program

|
The objective of the Best Practice Award program is to encourage the development of innovative or creative pharmacy practice programs or innovative approaches to existing pharmacy practice challenges in health systems within the state of Illinois. Applicants will be judged on their descriptions of programs and practices employed in their health system based on the following criteria:
Past winners include: 2012 2011 2010 |
Online entry form: http://www.ichpnet.org/professional_practice/best_practices/
Eligibility Instructions for preparing manuscript The manuscript should be organized as a descriptive report using the following headings:
Format All applicants will be notified of their status within three weeks of the submission deadline. Should your program be chosen as the winner:
Non-winning submissions may also be considered for publication in the ICHP KeePosted, but your permission will be obtained beforehand. |
Columns
 President’s Message
President’s Message
Our Role in Healthcare: a Personal Reflection
by Tom Westerkamp, ICHP President
My older brother, Jack, was diagnosed with metastatic pancreatic cancer in November 2011. We know the devastation of this disease, and as cancers go, this is typically an aggressive, relentless disease with a grim prognosis – not a good one to get if you have any choice in these matters. As a pharmacist, my family members came to me for advice on information that they had Googled. They had gleaned information from cyberspace on possible “cures” and promising treatment regimens. All I had were depressing facts, sobering statistics and weak answers.
He had a radical surgical procedure in January 2012, and endured twelve months of chemotherapy, side effects, pain, nausea and vomiting. The family arranged multiple visits out to see him where he lived in rural Iowa. He was treated at a large teaching hospital in Omaha and was referred to a regional cancer specialty hospital in Illinois. While in the Chicago area for chemo, we had more frequent opportunities to get together and had simple meals together on days when his GI tract cooperated and his nausea and vomiting were under control.
I do not have a lot of clinical experience in oncology; most of my training was in critical care. During this past year, I relied on the input of a couple of oncology pharmacy specialist friends that I know who were very helpful in providing information to me. George (in Evanston) and Tom (in Omaha) provided input on the various chemo regimens that they have experience with and always had helpful hints on treating the side effects my brother experienced. Their expertise with various treatment modalities they have used with success was helpful, and I eagerly shared their suggestions with my brother and his immediate family.
An important message to all of us that practice in pharmacy: no matter what our role is, no matter what our title is, no matter where we practice, never forget how important providing solid drug information can be to the patients and families and friends with which we interact. Never forget that there are many people looking for drug information, and that many people rely on our input and suggestions. Never forget how important it is to speak to patients and their families with a smile and caring attitude. Our knowledge is essential for many patients (and their families) to get through what frequently are extremely difficult times. In our busy day-to-day activities, when we get so caught up with phones ringing and dozens of orders to review and process, IVs and chemotherapy orders to prepare, and meetings to attend, it’s easy to lose sight of what we are each called to do. It’s easy to forget how important our role is with all that is going on in our busy lives.
All it takes is a family member or friend with a serious illness or severe side effects to jolt us out of our day-to-day routine with questions about their drug therapy to stop us in our tracks, and remind us how important our role in healthcare is.
I was reminded of this many times this past year while my brother was being treated. After Jack died in January, the absence of drug therapy questions from the family, and the void it created, served as a reminder to me of the role my oncology pharmacy specialist friends played in easing his burden, especially at the end.
So as we look forward to the arrival of Spring, and plow through another day at work or at school, with all the hectic activities that get jammed into it, I would ask you to once in a while take a deep breath and remind yourself why you went into pharmacy and what an important role you play on the healthcare team. We are important. We do touch the lives of our patients. We may not see it frequently, but our contributions do have an impact on the lives of our patients and their families. Whether our primary responsibilities are in drug purchasing, drug distribution, clinical, administrative, teaching or full-time learning, remember how important our professional role is, and that we are all trying to help patients.
Thanks for caring.
 Directly Speaking
Directly Speaking
Building Alliances and Accepting Compromise
by Scott A. Meyers, Executive Vice President
Last time I checked, Illinois was still part of the United States of America, and the USA was still a democracy. And while hospitals and health-systems don’t always function as democracies, there are some lessons to be learned for a properly operating democracy. Having made that last statement, I am by no means endorsing the current political arena in the US as a properly operating democracy. The US and Illinois Legislative and Executive branches have lost the ability to compromise almost completely. Our elected officials need to reread their history books to see how the early leaders of this country envisioned our existence.
Unfortunately, the current political climates in Washington, DC and Springfield are out of my and our control, at least until the next elections when hopefully enough US and Illinois citizens will band together to demonstrate their dissatisfaction and disappointment at the voting booth! In the meantime, pharmacy and all of health care continue to face struggles as a result of factors. Cost-containment efforts, new challenging resistant infections, more government and accrediting body regulation and expanding technology and treatment options all pose unique challenges and opportunities for health care in general and for us, pharmacy specifically.
Just like the at the State and Federal level there is an important political environment, the hospital has its own political climate, albeit without the elections. But elections may be the only difference. In the politics of government there are alliances that often produce change at a faster pace than most observers would expect. Frequently these alliances are made of members of different parties making the effort bi-partisan. Sometimes it can be a struggle to build an alliance within a single party. But most times, it takes some alliance building to get bills passed or defeated.
In the hospital, it has been known to be difficult for pharmacy and nursing to see eye-to-eye. However, when they do and work for the common good, amazing accomplishments can be achieved! The same is true with pharmacy and IT or pharmacy and administration or even pharmacy and their suppliers. But whenever a win-win can be identified, the change usually moves quicker and the results are often magnified. This shouldn’t be a new concept.
But just like the Executive and Legislative branches of government in Illinois and the US, we forget that a decision to find a win-win rather than a winner-takes-all result can make accomplishing the goal possible and will often amplify the positive gains down the road. So building alliances should be an important function in every pharmacy director, manager and supervisor’s job description.
However, alliances with other departments may not be initially possible, so then what do you do? First, look for a champion or two within the department you seek to partner with to help you get the rest on board. Individual champions can facilitate the alliance building process, so tap into the relationships your staff members have built with individual members of the other department. Use all your resources, but remember what the Knight Templar warned Indiana Jones when he sought to select the cup he thought was the Holy Grail, “You must choose wisely!”
Selecting just anyone from another department to champion your cause could cost you any gains you may already have achieved. To put it simply, think of who in your own department would carry the least amount of influence with you and make sure you have done enough background work to make sure you haven’t selected that same type of person in the department you are trying to court. It makes the most sense to go after the most respected member of the department, but sometimes the hardest worker may be of equal value. This is why professional working relationships outside your department by all your staff are critical and should be encouraged whenever possible. As a matter of fact, feedback from other departments about positive relationships between their staff and the department staff could and should be used during annual performance evaluations! And for those of you who think, “I just need to do my job and I don’t have time to schmooze people outside of pharmacy!”, don’t say I didn’t give you a heads up.
As pharmacists we always talk about being a member of the patient care team, but as pharmacists and pharmacy technicians we also need to think more globally about being a member of the health-system team. Each member of the pharmacy department needs to build relationships with members of any department they interface with daily, weekly or even monthly. Each positive relationship will prove to be helpful sooner or later.
Once the relationships are identified, you will find it is difficult to go for the winner-takes-all objective because the relationship will be damaged or destroyed. Accepting compromise to get closer to your goal is better than losing an all out fight and landing further from it. Working with each other always produces more than working against each other.
Maybe instead of letting political leaders from opposing parties play golf together, we should encourage them to build a Habitat Home, serve a meal in a soup kitchen together or better yet, clean the litter off a section of interstate highway together! Then they would actually experience the benefit of working together, feel the satisfaction of accomplishing a goal and develop a relationship that is not based on competition but rather cooperation. Then building alliances and accepting compromise might come a little easier!
The GAS from Springfield
Are “Biosimilars” Really that Dangerous?
by Jim Owen and Scott Meyers
Are “Biosimilars” really that dangerous? You sure would think so if you listened to the lobbyists from Genentech and Amgen in Springfield. These two biologic agent manufacturers have asked Senator Antonio Munoz to sponsor SB1934 that if passed would require pharmacists to notify the prescribing physician of an FDA-approved interchange within 5 days of making a switch.
First, there are some questions we think you might have right off the bat. One, are there any biosimilar agents available and approved for interchange currently in the US? The answer would be NO! Two, what is the definition of a biosimilar currently in the US? The answer would be…it’s not officially defined yet! Three, why all the excitement and concern around biologic agents, anyway? The answer would be biologic agents are for the most part much safer (less toxicity or side effects and adverse reactions than many other classes of medications (i.e., anti-coagulants, or anti-epileptic agents). Finally, most biologics are currently administered by injection or infusion in an infusion center, hospital or physicians office so wouldn’t the prescriber see what the patient is receiving or at least wouldn’t the product name appear in the medical record? The answer right now would be YES!
So if all the above is true, why are these manufacturers pressing forward with a bill that will inhibit interchange of eventually FDA-approved interchangeable biologic agents or biosimilars? MONEY! Of course, that’s usually the answer when the General Assembly gets involved! Patient safety is their excuse but money is the real reason. Prescribers in Illinois have worked with generic substitution for a couple of decades with few if any problems. When warfarin first became available generically, there was concern, but with pharmacist oversight, the substitutions proved to be safe. Several years ago, the manufacturers of anti-epileptic medications waged a similar fight to the one we’re battling now and eventually were turned back with the only concession from pharmacy being that the patient receive a written notice at the time of substitution when dispensing occurred.
Earlier in March, every ICHP member with an e-mail address was sent two e-mail blasts urging them to contact their Illinois Senator and urge them to vote “No” on SB1934. Whether you did or didn’t probably made an impact on where this bill goes this session. We will be sending out more e-mails of “Legislative Alerts” this spring and urge each of you to act whenever you receive one. We’ll make sure you have talking points and we’ll direct you who to call. But your help is critical as we fight to maintain the practice of pharmacy at a level that is appropriate for our education, training and professionalism.
Here are some of the important pharmacy-related bills ICHP is watching and working on, on your behalf!
SB0073/HB1052 – Sen. Steans, D-Chicago; Rep. Bradley, D-Marion – Amends the Nurse Practice Act and other Acts to remove references to a written collaborative agreement.
SB1610 – Sen. Silverstein, D-Chicago – Amends the Department of Public Health Powers and Duties Law of the Civil Administrative Code to require facilities licensed by the Department to mandate influenza vaccinations of affiliated health care workers or the health care worker must wear a surgical mask while performing duties during the influenza season.
SB1696/HB2534 – Sen. Althoff, R-McHenry; Rep. Fine, D-Glenview – Creates the Prescription Drug Repository Program Act to establish a voluntary repository for donated medications and supplies from health care facilities to be used for indigent patients.
SB1741 – Sen. Koehler, D-Peoria – Amends the State Finance Act to sweep funds from multiple dedicated funds into the General Revenue Fund including $2.054M from the Pharmacy Disciplinary Fund, making it almost insolvent.
SB1934 – Sen. Munoz, D-Chicago – Amends the Pharmacy Practice Act to restrict the interchange of “Biosimilar Agents”.
SB2248/HB3074 – Sen. Don Harmon, D-Oak Park; Rep. Bradley, D-Marion – Amends the Clinical Psychologist Licensing Act to provide specially trained and certified clinical psychologists the ability to prescribe medications.
HB0001 – Rep. Lang, D-Skokie – Creates the Compassionate Use of Medical Cannabis Pilot Program Act, allowing registered qualifying patient to possess up to 2.5 oz of medical cannabis.
HB0011 – Rep. Flowers, D-Chicago – Amends the Pharmacy Practice Act and other Acts and would require pharmacies that receive State or Federal funds to provide services to the unemployed without reimbursement.
HB0072/HB1343 – Rep. Mussman, R-Schaumburg; Rep. Sosnowski, R-Rockford – Amends the Safe Pharmaceutical Disposal Act and the Pharmacy Practice Act to allow pharmacies to voluntarily take back unused, unwanted or expired pharmaceuticals.
HB0084 - Rep. Franks, D-Woodstock – Amends the Wholesale Drug Distribution Licensing Act to prohibit the sale of “drugs in shortage” by any entity other than licensed manufacturers and wholesalers.
HB2823 – Rep. Mitchell, R-Decatur – Amends the Controlled Substances Act to remove the 30-day supply limit on prescriptions for CII controlled substances.
Please watch your e-mails and future issues of KeePosted so that you can stay informed and be proactive on behalf of your profession! The legislative session will continue until the end of May, so the fight is nowhere near over!
New Practitioners Network
Antimicrobial Stewardship
by Jason Morrell, PharmD
If you are a new practitioner and are starting an antimicrobial stewardship program or simply wish to gain confidence, I strongly advise you to consider the Society of Infectious Diseases Pharmacists (SIDP) certification program or the Making a Difference in Infectious Diseases (MAD-ID) certification program.
My story with stewardship began one day at work. The clinical coordinator announced that the department would undertake antimicrobial stewardship. This decision made several pharmacists nervous. Personally, I was excited. I was eager to learn more about infectious diseases pharmacotherapy and apply this knowledge to improve patient outcomes. I remember how stimulating and rewarding it was a few years ago, during my infectious disease rotation, to de-escalate therapy and recommend different antimicrobials. One week of that rotation was devoted solely to conducting antimicrobial stewardship. So I had a lot to learn. However, the great thing was that compared to some of my colleagues, I already knew what a difference interventions make on institution-specific outcomes.
To help implement antimicrobial stewardship, our institution applied for and was subsequently awarded a grant which would pay for everyone to become certified in stewardship through SIDP. I would highly recommend this self-study program to any practitioner, new or seasoned. This substantially improved my comfort level. The first phase of the program is listening to lectures on microbiology, pharmacology and pharmacotherapeutics and taking an examination after each lecture. Once these are complete, the participant completes four webinars that include a live question and answer period. Topics include antibiograms, optimizing outcomes, and a few others. Finally, the last phase involves completing a project at the institution using the information learned. I worked with a colleague to perform a DUE on antifungals, to understand how many patients are affected by invasive Candidiasis at our institution and if the antifungals were being prescribed appropriately. To my surprise, we found many instances of C. glabrata and kruseii, as well as under-dosing of intravenous fluconazole, failure to de-escalate therapy, and inappropriate duration of therapy. At this time, my colleague and I are looking into possible use of the Peptide Nucleic Acid (PNA) Fluorescence in situ Hybridization (FISH) technology to increase our identification of a specific Candida species and recommend to the prescriber appropriate therapy in a timely fashion.
Another program offered annually through the Infectious Diseases Society of America is the Making a Difference in Infectious Diseases (MAD-ID) conference. This consists of preparatory work, a two-day live event and a project at one’s institution. While I have not attended the MAD-ID program, I have spoken with an ID resident who did, and had positive feedback about the program. My institution utilizes Sentri 7, a clinical surveillance program, to help devote antimicrobial stewardship resources appropriately. One rule created by a colleague is to flag all patients with a vancomycin MIC of two, as there are poorer outcomes reported with these patients if they are on vancomycin. Another rule is for any patient who has two anaerobic drugs. The drawback to this rule is that the rule will include patients receiving treatment for Clostridium difficile-Associated Diarrhea (CDAD) and another anaerobic infection. An additional rule is for patients on tigecycline, voriconazole, daptomycin, linezolid or aztreonam to see if this is the most appropriate pharmacotherapy. The possibilities are endless with clinical decision support technology.
Call for NPN Volunteers
NPN Helps Ronald McDonald House
 Calling all students and recent graduates (< 10 years), join the New Practitioners Network for a networking and volunteer event at the Lurie Ronald McDonald House (211 East Grand Avenue, Chicago, IL) on Friday, May 3rd from 6:00-8:00pm. We will be preparing a taco bar to serve to the 70+ people staying at the house and want your help*!
Calling all students and recent graduates (< 10 years), join the New Practitioners Network for a networking and volunteer event at the Lurie Ronald McDonald House (211 East Grand Avenue, Chicago, IL) on Friday, May 3rd from 6:00-8:00pm. We will be preparing a taco bar to serve to the 70+ people staying at the house and want your help*!
Students contact your SSHP Chapter President for registration information.
Pharmacists can register online at http://www.ichpnet.org/calendar/event.php?ce_id=318
For general information: http://rmhccni.org/meals-lurie/
For event specific information contact Colleen Czerniak at coczerni@nmh.org
Volunteers will be responsible for bringing and/or preparing food at the event, meal set-up and clean-up. Additionally, volunteers are invited to join the guests for the meal that we prepare. A sign-up sheet of food items will be sent out closer to the date of the event.
*Due to a limited amount of space, we will be accepting the first 20 volunteers.
If you wish to help with the event but cannot attend, we will be accepting monetary donations to help cover the cost of food. Please contact Jan Mark at janm@ichpnet.org or 815-227-9292.
Leadership Profile
Leadership Profile: Fatima Ali

Where did you go to pharmacy school?
Midwestern University Chicago College of Pharmacy, Downers Grove, IL
Trace your professional history since graduation: where have you trained / worked, any special accomplishments? (Include a description of your current area of practice and practice setting.)
I have a Bachelors of Science in Chemistry from Roosevelt University. I graduated with a Doctorate in Pharmacy from Midwestern University Chicago College of Pharmacy and pursued a first year post-graduate Pharmacy Practice Residency at Advocate Lutheran General Hospital. My residency project was on procalcitonin-guided antimicrobial therapy for which ICHP awarded my residency project the Best Practice award in 2011. After completion of my post-graduate training, I accepted my current appointment as an Assistant Professor. I am also the Director of the Resident Teaching Certificate Program. As part of this program, I mentor post-graduate pharmacy practice residents as well. This residency year of 2012 to 2013, I am coordinating and managing seventeen residents from four affiliated clinical institutions in the Chicagoland area.
Describe your current area of practice and practice setting.
My clinical practice includes being on the internal medicine team as a clinical pharmacist to ensure appropriate medication therapy management. At Rush Medical Center, I round with one of eight internal medicine teams. Our medical team consists of an attending, one senior resident, two medical residents, a pharmacist, and medical and pharmacy students. On a daily basis, I review patient medication therapy for appropriateness, perform order verification, educate healthcare providers about medication therapy, counsel patients about risk and benefits of their medications upon discharge, and precept pharmacy students.
How long have you been an advisor?
Since July 2011 - present
What do you like about being a chapter advisor?
I have the opportunity to mentor students from their first year in the program and it gives me satisfaction to observe the students emerge as leaders and grow professionally through the program.
What benefits are there?
One of the benefits is being able to mentor students and participating in their events as the faculty advisor. Also, coordinating and participating in the Clinical Skills Competition was a good experience.
What made you decide to become a chapter advisor?
Roosevelt University College of Pharmacy is a new college of pharmacy. At the start of the program, I was one of the faculty with a health-system background and involvement with ICHP and ASHP and had an interest in starting up the SSHP chapter at RUCOP.
What responsibilities do you have?
The SSHP student chapter aims to deliver the following services to the student members each term: fundraising event, health-system speaker, patient education service project, and writing a student column in ICHP’s KeePostedI advise and mentor the SSHP executive board by meeting with them on a weekly basis to keep them on track with their projects, provide feedback on the student reflection column and patient-related projects. As a faculty advisor and practitioner, I emphasize on giving back to the community through service and public health education.
What advice do you give others who are considering becoming an advisor at their institution or active in ICHP?
It is a good opportunity to network with other advisors and leaders within ICHP. Also, being an advisor allows you to be a mentor for students and watch them grow professionally. It also allows you to participate in Clinical Skills Competition and patient-related health projects.
Do you have any special interests or hobbies outside of pharmacy/work/school? Any special accomplishments?
I love to travel and have been to four of seven continents thus far!
Educational Affairs
Illinois Council of Health-System Pharmacists 2013 Spring Meeting Poster Abstracts
This issue of KeePosted contains the abstracts of the posters that will be presented at the ICHP 2013 Spring Meeting April 12th-13th. Posters will be presented Friday, April 12th from 5:30-6:30pm and Saturday, April 13th from 8:00-9:00am.
Original Poster Abstracts
- Management of Clostridium difficile infections and the effects of protocol regulated treatment on patient outcomes
- Impact of a Community-Based Outpatient Heart Failure Clinic on 30-day Readmission Rates
- Analyses of interventions at discharge made by a pharmacist care transition team in a community based hospital
- Assessing the clinical benefits of implementing a urinary tract infection treatment guideline in the emergency department
- Evaluation of Glucose Management and Coordination of Various Service Lines to Optimize Glycemic Control Within an Acute Hospital Setting
*ICHP Member
**Submitting Author
ICHP Poster Presentations – Original #1
TITLE: Management of Clostridium difficile infections and the effects of protocol regulated treatment on patient outcomes
AUTHORS: **Craig R. Grzendzielewski, PharmD; *Kimberly A. Janicek, PharmD; *Nicole Costa, PharmD; Frederick S. Alexander, MD
Presence Saint Joseph Medical Center
PURPOSE: Guidelines published in 2010 by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA) provide recommendations for the treatment of Clostridium difficile infections. However, these guidelines do not address treatment with fidaxomicin, which was approved in May 2011 to treat Clostridium difficile infections. At our institution, the treatment of Clostridium difficile infections is not standardized and varies between physician groups. The objective of this study is to determine the effect on patient outcomes after implementation of a protocol regulated Clostridium difficile algorithm which incorporates fidaxomicin.
METHODS: Prior to study implementation, the protocol was approved by the Institutional Review Board. A data surveillance system was used to identify patients who had positive Clostridium difficile tests between April 1, 2012 and September 30, 2012 for retrospective analysis. This analysis evaluated current treatment patterns and identified predictive factors that may correlate with outcomes. Predictive factors included: age, renal function, white blood cell count, concomitant antibiotic usage, and immunologic status. The primary outcomes of this study include length of stay and treatment duration. Secondary outcomes include 30 day re-admittance rates and appropriateness of therapy. Working with the infectious disease physician group, a Pharmacy and Therapeutics Committee approved treatment algorithm for Clostridium difficile infections was implemented for use in all patients with Clostridium difficile infections. A prospective analysis will be conducted between December 1, 2012 and March 31, 2013 focusing on outcomes listed above. Adherence to the treatment algorithm will be monitored by the clinical pharmacy staff.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Original #2
TITLE: Impact of a Community-Based Outpatient Heart Failure Clinic on 30-day Readmission Rates
AUTHORS: **Chelsea A. Williams, PharmD; *Dina L. Porro, PharmD; *Se H. Choi, PharmD
Presence Saint Joseph Medical Center
PURPOSE: With the enactment of the Patient Protection and Affordable Care Act, hospitals are now being penalized for excess heart failure readmissions. In an effort to streamline the number of patients who are being readmitted and maximize reimbursement rates, Provena Saint Joseph Medical Center (PSJMC) established a heart failure clinic to care for and treat these patients in an outpatient setting. The purpose of this study is to evaluate the outcomes of a community-based heart failure clinic on 30-day hospital readmission rates.
METHODS: The PSJMC outpatient heart failure clinic opened on November 15, 2012, taking patients on a referral basis. A retrospective review was completed using Midas™ software to compile patients and trend the pattern of heart failure admissions during the third quarter of 2012 at PSJMC. This baseline data will be used to compare changes in readmission rates following the opening of the heart failure clinic through March 2013. The patients who visit the clinic will be followed to determine if they have a reduction in the amount of heart failure readmissions to PSJMC. This data will also be used to calculate a cost savings for the hospital based on the reduced number of patients being readmitted for their heart failure treatment. The role of the pharmacist in the clinic will include performing medication reconciliation, medication management, and patient education. Additionally, a drug utilization and cost differentiation will be conducted to compare differences in treatment for the nurse practitioner and pharmacist in the clinic verses the nurse practitioner alone.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Original #3
TITLE: Analyses of interventions at discharge made by a pharmacist care transition team in a community based hospital
AUTHORS: **Amy Christine Boblitt, BS, PharmD; Megan Theresa Fines, BS, PharmD; *Ann Groesch, BS, PharmD; *Megan Elizabeth Metzke, PharmD, BCPS
Memorial Medical Center
PURPOSE: Medication reconciliation and education are essential elements in the transition of care from hospital to home. Circumstances that often surround the discharge process can make patients vulnerable to medication errors, including inadequate communication among disciplines. Additional barriers include low health literacy and lack of medication instruction. The goal of this project is to quantify and categorize the interventions made by care transition pharmacists during discharge.
METHODS: The position of the care transition pharmacist was created to offer assistance in medication counseling for patients at high risk for discharge medication errors or non-compliance after discharge. The pharmacy team may be consulted by patient care facilitators (nurses on the floors who facilitate safe discharge processes), physicians, diagnosis-driven lists, order entry pharmacists, or the care transition pharmacists. Patient selection is based on criteria including poly-pharmacy, low health literacy, high risk medications, multiple medication changes during admission, and primary diagnosis. At discharge, a care transition pharmacist reviews the discharge orders for accuracy, while assuring the medications are appropriate for the patient’s disease states and meet the hospital core measures. The pharmacist compiles a typed discharge medication list, which is provided to the patient and saved into the hospital system. Patient education was performed using teach-back methodology. Data was collected prospectively and intervention characteristics were reported. Comparisons of intervention and discharge attributes were made to evaluate pharmacist transitional care and program utility.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Original #4
TITLE: Assessing the clinical benefits of implementing a urinary tract infection treatment guideline in the emergency department
AUTHORS: **Katherine Rita Allen, PharmD PGY-1; *Dina L. Porro, PharmD
Presence Saint Joseph Medical Center
PURPOSE: Fluoroquinolone resistance among common urinary tract infection (UTI) pathogens has been increasing on a global level. In the literature, academic health care facilities have documented increased resistance rates with fluoroquinolones, which is now presenting in community hospitals nationwide. The objective of this study is to assess the effect of implementing empiric UTI antimicrobial guidelines in the emergency department (ED) on treatment outcomes.
METHODS: A data surveillance system utilized at Saint Joseph Medical Center was used to identify patients admitted to the ED who had positive urine cultures showing resistance to fluoroquinolones from July 2012 through September 2012. In addition to culture and sensitivity data, the following patient specific information has been collected: age, gender, drug allergies, white blood cell count, occurrence of fever, urinalysis results, renal function markers, empiric antimicrobial agent initiated prior to culture results, and antimicrobial agent selected after the final sensitivity results. ED treatment guidelines were then developed to promote appropriate empiric UTI antimicrobial therapy. Prior to guideline implementation, the ED physician staff received instruction on the proper use of the guideline and education regarding fluoroquinolone resistance at our institution. Following guideline implementation, initial choice of antibiotic, culture and sensitivity reports, antibiotic changes made based on sensitivity results, and length of antibiotic therapy will be collected for analysis over a three-month period. The primary objectives of this study will be to determine if the initiation of an empiric UTI treatment guideline results in more accurate initial use of antimicrobial therapy and a shortened duration of treatment.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Original #5
TITLE: Evaluation of Glucose Management and Coordination of Various Service Lines to Optimize Glycemic Control within an Acute Hospital Setting
AUTHORS: **Rebecca A. Adorable, PharmD, PGY-1; *Se H. Choi, PharmD; Rachel M. Crumb, RN, BSN, CDE; William Farrell, MD
Presence Saint Joseph Medical Center
PURPOSE: Hyperglycemia in non-critically ill patients (with or without diabetes), irrespective of its cause, is associated with poor outcomes and is often overlooked and inadequately treated. Glucose management at Presence Saint Joseph Medical Center (PSJMC) has become more complicated due to the implementation of patient meals on demand. The use of sliding scale insulin only regimens is common for glycemic management in non-critically ill patients, and the current standard of care for glycemic management is inconsistent throughout PSJMC. The purpose of this study is to develop a multidisciplinary glucose management service to optimize glycemic control by means of a blood glucose order set.
METHODS: A retrospective chart review was conducted from September and December 2012 in non-critically ill, post-operative patients located on the orthopedic unit (7W). Current management of glycemic control was evaluated by examining the sequence and difference in time between insulin administration, point-of-care glucose monitoring, and meal delivery. Patients =18 years of age who are diabetic requiring meal time insulin therapy or non-diabetic experiencing hyperglycemic episodes were eligible for inclusion. Following implementation of the blood glucose management protocol, eligible patients on 7W will be monitored to assess overall glycemic control for a one month period. Various in-services regarding insulin education and an overview of the protocol will be provided to all staff affected by the initiative. Data variables collected for analysis include: patient demographics, indication for hospital admission, insulin types, mean fasting and pre-prandial blood glucose levels, hypoglycemic episodes, and length of stay.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
PLATFORM PRESENTATIONS
The following two original research poster submissions were accepted as platform presentations. The presentations will take place on April 13th starting at 1:00pm.
ICHP Poster Presentations – Platform Presentation #1
TITLE: Effects of an outpatient generic medication voucher program on the generic dispensing ratio (GDR) in a 4,100 physician-hospital organization (PHO) - 4 years experience
AUTHORS: **Mark Edward Greg, PharmD, RPh
Advocate Physician Partners
PURPOSE: To describe the effects of an outpatient generic medication voucher program on the GDR in a 4,100-plus physician member PHO as part of a comprehensive academic detailing program over a four year period of time.
METHODS: The APP generic medication voucher program was in place from September 1, 2008 through December 31, 2012. Vouchers provided patients up to $10 off of their copay or cash price paid for the first fill of up to a 30-day supply of a select number of generic medications at any Walgreens Pharmacy in Illinois. Availability of the voucher program was communicated to APP prescribers by email, on-line ordering through an intranet portal, a table display at meetings, and during 1:1 meetings at prescriber practices. Covered generic medications were reviewed and modified yearly based upon redeemed voucher data, prescriber feedback, and generic medication category goals. Redeemed voucher data was included in prescriber GDR calculation.
RESULTS: Over 11,200 vouchers were redeemed. Non-employed, independent Pediatricians, OB/GYNs, and Gastroenterologists were the top medical specialties using the program. Oral antibiotics, fluticasone nasal spray, and PEG-3350 bowel prep were among the top three classes of medications that were redeemed. Participating physicians easily exceeded yearly PHO goals for generic prescribing for their given medical specialty.
CONCLUSIONS: The addition of an outpatient generic medication voucher program is an effective tool as part of a comprehensive pharmacist-conducted academic detailing program to promote outpatient generic prescribing and increase GDR in a PHO.
ICHP Poster Presentations – Platform Presentation #2
TITLE: Efficacy of Antiretroviral Therapy in a Large Urban Clinic: Does a Diverse Patient Population Require a Diversity of Treatment Options?
AUTHORS: **Andrew Merker, PharmD, Pharmacy Resident; John H. Stroger, Jr. Hospital; *Blake Max, PharmD, AAHIVE
Ruth M. Rothstein CORE Center
PURPOSE: There are numerous highly active antiretroviral therapy (HAART) combinations to treat human immunodeficiency virus (HIV). The high cost of preferred regimens, and possible availability of less expensive generics, may significantly impact formularies. The purpose of this study is to determine the proportion of patients engaged in care with undetectable viral load (VL) and document the diversity of regimens in order to evaluate the necessity of having a large complement of antiretrovirals for optimal HIV treatment.
METHODS: Data was obtained through electronic medical record. Patients must be: ≥ 18 years, HIV diagnosis ≥ 30 days, attend clinic as a walk in or scheduled appointment, engaged in care (≥ 2 clinic appointments in previous 12 months), and have a CD4 and VL within the previous 6 months. For patients receiving treatment, it must be for ≥ 3 months.
RESULTS: A total of 600 patients were observed, 90.5% male, and 105 different regimens were recorded with 65 unique to a single patient. Atripla® was most common (34.5%) followed by Truvada® and Norvir® boosted Reyataz® (10.5%). Salvage regimens accounted for 65.2% of therapies. Overall, 82% had undetectable VL and a mean CD4 count of 449.
CONCLUSIONS: Of the patients followed in clinic, over 80% have an undetectable VL. In addition, 10.8% were prescribed a unique regimen no one else is on. The future of antiretroviral formulary management will need to proceed cautiously; fiscal responsibility and availability of all antiretrovirals will need to be further evaluated to ensure optimal HIV treatment.
Encore Poster Abstracts
- Impact on pharmacist interventions by implementing pharmacy practice model changes
- Comparing change in hemoglobin A1C of patients in pharmacist managed telehealth clinic versus in-person clinic
- Stepwise implementation of total pharmacy medication reconciliation
- Analysis of the Completeness and Accuracy of Dietary Supplement Information in Wikipedia
- Impact of antibiotic stewardship program on the treatment of asymptomatic bacteriuria at an inpatient rehabilitation hospital
*ICHP Member
**Submitting Author
ICHP Poster Presentations – Encore #1
TITLE: Impact on pharmacist interventions by implementing pharmacy practice model changes
AUTHORS: **Ed C. Rainville, MS Pharm; *Jerry A. Storm, BS Pharm; *Vern L. Johnson, BS Pharm; *Mike R. Hawley, BS Pharm
OSF Saint Francis Medical Center
PURPOSE: The purpose of this study is to show the impact of pharmacy practice model changes on the number of pharmacists' interventions.
METHODS: Two practice model changes were implemented in February 2011. The process of pharmacist verification of drug orders was transferred from two centralized locations to decentralized pharmacists on the patient care units. The other change was to expand the decentralized staffing on weekdays, second shift by reassigning pharmacists from the central and satellite pharmacies. Utilizing available staff, a satellite pharmacy was closed and the number of pharmacists staffing in the main pharmacy was reduced. Four positions on second shift (1500-2300) were introduced. Pharmacist intervention data from July to December 2010 was utilized as the baseline measure; July to December 2011 data was chosen as the comparison after changes.
RESULTS: Overall, there was a 21.6% increase in interventions. The greatest change in pharmacist activity was during the second shift with increases of 31.2% in documented interventions and 32.2% in estimated cost avoidance. Types of interventions included order clarification, dosing consults, antibiotic stewardship, duplicate therapy, non-formulary to formulary changes, parenteral nutrition recommendations, dose changes, initiate new drug therapy and medication reconciliation. The additional estimated cost avoidance after the practice model change was $291,047.
CONCLUSIONS: Utilizing existing staff to provide unit-based pharmacy order verification and extending the hours of decentralized pharmacy services resulted in significant increase in documented clinical interventions, increased estimated cost avoidance and greater participation by unit-based pharmacists in processing of drug orders.
ICHP Poster Presentations – Encore #2
TITLE: Comparing change in hemoglobin A1C of patients in pharmacist managed telehealth clinic versus in-person clinic
AUTHORS: **Khyati Patel, PharmD, BCPS; Danielle Alsip, PharmD; Roshani Raval, PharmD; Todd Lee, PharmD, PhD
Rosalind Franklin University of Medicine and Science- College of Pharmacy, Edward Hines, Jr. VA Hospital, University of Illinois at Chicago-College of Pharmacy
PURPOSE: The primary objective of the study was to assess the effectiveness of a telehealth program by comparing changes in HgbA1c over 6 ± 3 months of patients in a telehealth clinic, where care was provided using telecommunication technology, versus in-person clinic. Secondary endpoints included change in HgbA1c over 12 ± 3 months, change in weight, enrollment into the MOVE! Program-a weight loss program provided by Hines, diabetes medication changes, compliance to clinic appointments, and adverse events related to diabetes medications.
METHODS: This was a retrospective chart review of 118 patients receiving diabetes care by a clinical pharmacist via in-person and telehealth modalities from January 2010 to December 2011 at an outpatient clinic affiliated with the Edward Hines, Jr. VA Hospital. Data collected include clinic location, age, gender, co-morbid diseases, diabetes management via other healthcare professionals, HgbA1c, weight, diabetes medications, status of enrollment into MOVE! Program, and adverse events of diabetes medications at baseline ± 2 months, 6 ± 3 months, and 12 ± 3 months. An ease of telehealth use survey consisting of 10 multiple choice questions was conducted to assess perceived barriers to the telehealth use.
RESULTS: The in-person group had an average HgbA1c reduction of 1.1% at 6 months versus 0.88% reduction in the telehealth group, p=0.46. Secondary outcomes revealed no statistically significant difference between the two groups. Outcomes of the ease of telehealth use survey were in favor of the telehealth technology use.
CONCLUSIONS: The study found no difference when two modalities of health care delivery, telehealth vs. in-person, used in a clinical pharmacist run diabetes clinic were compared with each other.
ICHP Poster Presentations – Encore #3
TITLE: Stepwise implementation of total pharmacy medication reconciliation
AUTHORS: **Jenan Eileen Dailey, PharmD Candidate 2013; Christina Sun Hwa Choi, PharmD Candidate 2013; *Yen Hoang Yvonne Duong, PharmD Candidate 2013
Midwestern University Chicago College of Pharmacy
PURPOSE: This study evaluated if a pharmacy student led pilot program would significantly improve the medication reconciliation process at Copley Memorial Hospital. This study aimed to increase continuity of care, interdisciplinary teamwork and the pharmacy’s role in direct patient care.
METHODS: Fourth year pharmacy students performed a stepwise medication reconciliation pilot based in the emergency department (ED). Phase I compared medication lists generated by pharmacy students to those of ED nursing staff. Phase II added a discharge counseling program. Phase III combined phases I and II into one role. Surveys measured patient and staff satisfaction with the program. Outcome measures were: completeness of patients' home medication lists, accuracy of medications upon discharge and satisfaction of staff and patients.
RESULTS: Student pharmacists recorded 57.45% more medications per patient list when compared to nurses (7.4 vs. 4.7, p<0.0001). Medication lists completed by students included more over-the-counter (OTC) medication usage (average OTC medications per list 2.47 vs. 1.36, p=0.04). ED and inpatient nurses reported time savings of 35 and 42 minutes respectively when pharmacy students completed initial medication histories. Physicians and nurses surveyed agreed that pharmacists are the most qualified to complete home medication lists and to perform medication discharge counseling (77.5% and 82.5% respectively, n=40). Patient satisfaction scores for medication discharge counseling by pharmacy were 4.54 out of 5.0.
CONCLUSIONS: This pilot program improved patient transition through the hospital and at discharge. The program created a pharmacy driven role to provide optimal patient care through complete medication reconciliation.
ICHP Poster Presentations – Encore #4
TITLE: Analysis of the Completeness and Accuracy of Dietary Supplement Information in Wikipedia
AUTHORS: **Jennifer Ann Phillips, PharmD, BCPS; Connie Lam, PharmD Candidate; *Lisa Marie Mackowski, PharmD, PGY-1
Midwestern University Chicago College of Pharmacy
PURPOSE: Wikipedia is a popular collaborative web-based encyclopedia. Published studies suggest that health information in Wikipedia is not as complete and accurate as information found in other on-line health websites. Since many consumers and pharmacists use on-line resources to find information on dietary supplements, it is important that reliable information on these agents is available. Evaluating the quality of information contained in this database may help guide healthcare practitioners and patients to appropriate resources.
METHODS: Wikipedia entries for the top 19 dietary supplements were evaluated on a single day. To determine completeness, the contents of each entry were evaluated to determine if information on therapeutic uses, adverse effects, dosing, drug interactions, pregnancy and contraindications was present. To determine accuracy, information within each entry was compared to information in Natural Medicines Comprehensive Database (NMCD) and Natural Standard. Accuracy was assessed for therapeutic uses, adverse effects, dosing, and pregnancy. To account for subjectivity, 3 reviewers performed the analysis.
RESULTS: Most entries contained information on therapeutic uses and adverse effects; information on drug interactions, pregnancy and contraindications was missing for most entries. Most entries had between 26-75% of the therapeutic uses validated by NMCD or Natural Standard; most had between 76-100% of adverse effects validated. Most of the dosing and pregnancy information was inconsistent with NMCD or Natural Standard. Inter-rater reliability was established for all categories.
CONCLUSIONS: Wikipedia should not be used as the sole source of information for dietary supplements since information is incomplete and partially inconsistent with reputable dietary supplement references.
ICHP Poster Presentations – Encore #5
TITLE: Impact of antibiotic stewardship program on the treatment of asymptomatic bacteriuria at an inpatient rehabilitation hospital
AUTHORS: **Nitika Agarwal, PharmD; *Mary Mekheil, PharmD; Steven Lewis, MD; Susan Isenberg, RN; *Xiao Yuan, Clinical Staff Pharmacist
Marianjoy Rehabilitation Hospital
PURPOSE: To evaluate the effectiveness of antibiotics stewardship program (ASP) lead by multi-professional team supported by physicians, nurses and pharmacists in reducing the treatment of asymptomatic bacteriuria (ASB).
METHODS: The antibiotics identified for treatment of UTI at our facility were ciprofloxacin, trimethoprim/sulfamethoxazole and nitrofurantoin. The retrospective review was conducted before the development of guidelines and education (Period 1) and after the ASP was fully implemented (Period 2). Period 1 used a stewardship model of pharmacist performing concurrent review and feedback. Between period 1 and 2 ASP team got created in Nov 2011 and concise guidelines defining UTI and asymptomatic bacteriuria (ASB) as well as unnecessary antibiotics treatment were developed and approved by Pharmacy and Therapeutics committee. Education on guidelines and definitions was provided to all physicians and pharmacists. New nursing documentation screen “UTI surveillance” was created in Meditech; nursing staff was educated on the use of this documentation tool. Physicians were encouraged to document rationale for starting antibiotics in progress notes. Period 2 used the guidelines and the tools that got created by the ASP team. Data collection included review of all patients (within a specific time frame) that received the above mentioned enteral antibiotics. Patients receiving antibiotics upon admission or receiving it for reasons other than UTI were excluded. The goal of the institution is to reduce over-prescribing of antibiotics, thus reducing adverse effects, resistance and cost.
RESULTS: About 19.8 percent of total number of patients admitted within study time frame prior to ASP in place were prescribed antibiotics compared to 7.7 percent patients after the ASP was implemented, resulting in a 61% decline in overall prescriptions of antibiotics .The antibiotics days of therapy per 1000 patient days declined by 43%. Further review of pharmacists’ interventions revealed that treatment of ASB declined by 59% after the ASP was fully implemented.
CONCLUSIONS: Setting a specific institutional goal, developing clear guidelines, and engaging nurses and physicians in an ongoing ASP dramatically improved performance by reducing the treatment of ASB thus leading to reduced antibiotic use.
Student Poster Abstracts
- Evaluation of Dronedarone Use
- A State-by-State Analysis of Medicaid Payment Programs for Clinical Pharmacy Services
- Fluoroquinolone cross-resistance of Pseudomonas aeruginosa
- Assessment of Sedation in Mechanically Ventilated Patients in a Medical Intensive Care Unit
- Platelet recovery in hospitalized patients with thrombocytopenia after changing beta-lactam therapy
*ICHP Member
**Submitting Author
ICHP Poster Presentations – Student #1
TITLE: Evaluation of Dronedarone Use
AUTHORS: **Deborah Christine Helmink, PharmD Candidate; *Jingyang Fan, PharmD, BCPS
Southern Illinois University Edwardsville School of Pharmacy, Mercy Hospital
PURPOSE: Dronedarone is a Class III antiarrhythmic agent that is approved for atrial fibrillation. It has been under scrutiny recently due to some literature suggesting its harm in certain patient populations. This study was a retrospective chart review that evaluated dronedarone use at a 1000-bed community teaching hospital and to determine the prevalence of contraindications in those patients receiving dronedarone.
METHODS: Patients were eligible for evaluation if they received dronedarone during their hospitalization between January and December 2011. Information was collected for 50 patients randomly selected from the list of eligible patients. Data collected from the electronic medical charts included demographic information, medical history, indications for dronedarone, contraindications if applicable, and other antiarrhythmic usage.
RESULTS: Among the 50 randomly selected patients, the average age was 72.34, 56% of the population was female, and 92% were Caucasian. Seventy four percent of patients were on dronedarone prior to hospital admission. Of the patients with prior medications on record, 60% had previously tried another antiarrhythmic medication. Twelve patients (24%) had at least one contraindication to dronedarone (two patients had two contraindications for a total of fourteen contraindications). Of these patients, six of the contraindications were new for this hospitalization. All of the new to hospitalization contraindications were acute heart failure decompensation requiring hospitalization.
CONCLUSIONS: Our study suggested that the prevalence of contraindications is high in patients currently receiving dronedarone. Half of these contraindications were newly developed, suggesting that the appropriateness of dronedarone use should be reevaluated at every hospitalization.
ICHP Poster Presentations – Student #2
TITLE: A State-by-State Analysis of Medicaid Payment Programs for Clinical Pharmacy Services
AUTHORS: **Maria C. Tangonan, PharmD Candidate 2014; *Ciby Chacko, PharmD Candidate 2014; *Asha Kalichira, PharmD Candidate 2015; *Shivali Shah, PharmD Candidate 2014; *Alice Lee, PharmD Candidate 2014; *Shally Alendry, PharmD Candidate 2014; *Tszyee Tsui, PharmD Candidate 2014; Sandra Durley, PharmD, RPh1; JoAnn Stubbings, MHCA; Christine Rash, PharmD
University of Illinois College of Pharmacy, University of Illinois Hospital & Health Sciences System
PURPOSE: To establish a comprehensive list of clinical pharmacy programs in the United States for which pharmacy services are paid by state Medicaid agencies.
METHODS: The 50 states and Washington D.C. were divided into seven groups and assigned to the students who authored this study. Each student conducted primary literature searches, visited state Medicaid websites, consulted previous publications, and contacted state pharmacy associations. Program descriptions, goals, outcomes, and implementation methods as well as, pharmacist requirements and reimbursement information were documented if available.
RESULTS: Current findings demonstrate that pharmacists are being paid for services, such as medication therapy management (MTM), mass vaccination, academic detailing, compounding, as well as other disease management programs in various states including Florida, Minnesota, New York, Mississippi, Oregon, and more. Additionally, several states are currently implementing pilot programs including Texas, Minnesota, Missouri, and others.
CONCLUSIONS: Our research offers evidence that programs elevating the pharmacist’s role as part of the healthcare team with the potential of providing improved health outcomes and cost savings exist and can be utilized on a national level. The implications of this study justify payment for clinical pharmacy services and may be applied to other insurance providers and patient populations.
ICHP Poster Presentations – Student #3
TITLE: Fluoroquinolone cross-resistance of Pseudomonas aeruginosa
AUTHORS: **Britany Nicole Walls, PharmD Candidate 2013; *Katie Ronald, PharmD, BCPS
Southern Illinois University Edwardsville School of Pharmacy
PURPOSE: Resistance to antibiotics is an increasing problem for many hospitals. To optimize drug therapy, resistance patterns must be taken into account when prescribing antibiotics. Adding to the complexity of combating antibiotic resistance is the occurrence of cross-resistance between antibiotics. Pseudomonas aeruginosa in particular can acquire resistance to multiple antibiotics. The purpose of this study is to determine cross-resistance of fluoroquinolone-resistant Pseudomonas aeruginosa to other antibiotics.
METHODS: Pseudomonas aeruginosa isolates with susceptibility results to fluoroquinolones of “resistant” or “intermediate” will be analyzed. The isolates include all Pseudomonas aeruginosa isolates that were obtained from Memorial Medical Center between January 1, 2011 and June 1, 2012. Duplicate specimens from the same site on the same patient will be excluded. Susceptibilities of fluoroquinolone resistant Pseudomonas aeruginosa isolates to other antibiotics will be used to determine the rate of cross-resistance. The percentage of isolates that are considered multi-drug resistant (MDR) will be examined. Resistance to both agents of commonly used combinations including a fluoroquinolone for double coverage will be noted.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Student #4
TITLE: Assessment of Sedation in Mechanically Ventilated Patients in a Medical Intensive Care Unit
AUTHORS: **Kristin Anne Courtright, PharmD Candidate; *Katie Elizabeth Ronald, PharmD, BCPS
Southern Illinois University Edwardsville School of Medicine
PURPOSE: To determine baseline hospital and medical intensive care unit length of stay, time to extubation, and amount of sedation medication used at Memorial Medical Center’s medical intensive care unit prior to implementation of a sedation protocol. Baseline characteristics will be compared to follow-up data after sedation protocol is implemented to determine areas for improvement.
METHODS: This was a single-center, retrospective study of patients ages 18-89 admitted to the ICU, sedated, and on a ventilator at Memorial Medical Center between October 1, 2011 and June 30, 2012. Exclusion criteria include ages <18 and >90 as well as DNR or expired status. Data collected included patient’s age range, DNR/hospice status, ICU and hospital length of stay, time to extubation, and amount of each agent received while the patient was ventilated. Medications evaluated included midazolam, lorazepam, propofol, morphine, hydromorphone, fentanyl, and dexmedetomidine.
RESULTS: Research In Progress
CONCLUSIONS: Research In Progress
ICHP Poster Presentations – Student #5
TITLE: Platelet recovery in hospitalized patients with thrombocytopenia after changing beta-lactam therapy
AUTHORS: **Katelyn Mae Daniels, PharmD Candidate; *Scott Bergman, PharmD, BCPS
Southern Illinois University Edwardsville School of Pharmacy and Southern Illinois University School of Medicine
PURPOSE: This study aims to determine if platelet recovery differs after changing beta-lactam therapy in hospitalized patients with thrombocytopenia. We will compare patients that were switched to an alternative class of antibiotics to those that were changed to a different beta-lactam therapy.
METHODS: Using the health system's electronic database, medical records were retrospectively reviewed to identify all hospitalized patients discharged with ICD-9 code 287.49 for “other secondary thrombocytopenia” over the past 5 years (July 1, 2007 – June 30, 2012). This list was further narrowed down by identifying those patients who were taking a beta-lactam antibiotic at the time of diagnosis. . Finally, patients were only included in the study if the diagnosis of thrombocytopenia could not definitely be attributed to any other cause, (such as heparin or chemotherapy). The information collected included the following: original beta-lactam at time of diagnosis, other medications the patient took that are known to increase or decrease platelets, concurrent disease states, the length of time receiving the beta-lactam until development of thrombocytopenia, the lowest platelet count, the agent the patient was switched to once the offending agent was discontinued, whether the platelets recovered to greater than 100,000 cells/mL during hospitalization, and the length of time until recovery from thrombocytopenia. Data regarding antibiotic switch and platelet recovery will then be analyzed using the chi-square or Fisher's exact test depending on the number of patients in each category.
PRELIMINARY RESULTS: P 419 patients were diagnosed with secondary thrombocytopenia during this timeframe. Of those, 229 patients were on a beta-lactam during their stay. 18 patients met inclusion criteria due to no other known cause of thrombocytopenia. Half of these 18 patients were switched to an alternative beta-lactam to complete their course of therapy, 7 patients were switched to alternative classes of antibiotics, and 2 patients discontinued antibiotic therapy completely. Overall, platelet counts for 17 of the 18 patient’s platelet counts fully recovered once the likely offending beta-lactam agent was discontinued. The one patient whose platelet counts did not recover was switched from their beta-lactam to an alternative class of antibiotics.
CONCLUSIONS: In patients that developed thrombocytopenia while on a beta-lactam antibiotic, platelet recovery was not more apparent in those switched to an alternative class of antibiotic compared to those continuing therapy with a different beta-lactam. Prospective trials with a larger sample size are warranted to avoid the selection bias and confounding variables which may have impacted these retrospective results.
ICHPeople
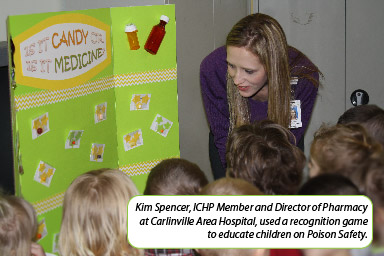
Ask First
Kim Spencer, an ICHP Member Pharmacy Director at Carlinville Area Hospital in Carlinville, IL, organized a volunteer effort to help educate area children in Poison Safety for March Illinois Poison Prevention Month. Carlinville Area Hospital is a critical access hospital in a town with one non-home based daycare and two preschools. Kim took three other individuals from the hospital with her, including the ED nurse manager, the quality improvement manager, and an IT specialist. Kim presented the poison prevention information and the two nurses helped with the games while the IT specialist provided technical support. Volunteers showed the Ember 911 Poison Safety video or the Quills Up for safety video with four preschool-age classes – three at the daycare and one at a preschool (about 75 kids total). They also played two games, one with picture recognition of poisons versus safe items and one with differentiating medications from candy (pictured). Kits were sent home for parents that included information about the Illinois Poison Prevention Center as well as flashlights and magnets with the IPC number. A letter also went home emphasizing the volunteers’ education theme of “ask first.”
In the evening, the volunteers educated the daycare center providers about the incidence of child poisonings, common poisons, ways to prevent accidental poisoning, actions to take if a poisoning is suspected, and ways to get more information or education about poison prevention.
Way to go!
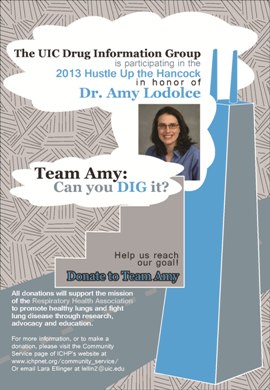 Team Amy
Team Amy
ICHP Members Lara Ellinger, Michelle Bryson, Shadi Ghaibi, and Milena McLaughlin participated in the annual Hustle Up the Hancock on Sunday, February 24 to raise money for the Respiratory Health Association in honor and memory of Dr. Amy Lodolce. Everyone on their team successfully reached the top of the Hancock Building in Chicago and their donations raised a total of $6420!
Great job, Team Amy, and thanks to everyone who supported them!
If you would like more information about 2013 Hustle Up the Hancock, please click on the link below.
https://secure.imisfriendraising.com/registrant/startup.aspx?eid=10172&langpref=en-CA
Baby News
 ICHP Member Jaime Borkowski and her husband, Erick, welcomed baby girl Cecilia Lynn Borkowski into the world on Monday, February 25th at 0554. She weighed 7 lb 7 oz and was 20 1/4 in long. “We are all doing well and her big brothers are very excited,” Jaime said.
ICHP Member Jaime Borkowski and her husband, Erick, welcomed baby girl Cecilia Lynn Borkowski into the world on Monday, February 25th at 0554. She weighed 7 lb 7 oz and was 20 1/4 in long. “We are all doing well and her big brothers are very excited,” Jaime said.
What should we feature in the next ICHPeople? Send suggestions, pictures and info to Amanda Wolff at AmandaW@ichpnet.org.
Medication Safety Pearl
IL-ADAP and decreasing ARV Resistance in a vulnerable population at the UIC HIV Outreach Clinics
By Ream Qato, PharmD, Clinical Staff Pharmacist, University of Illinois at Chicago College of Pharmacy and Renata Smith, PharmD, Clinical Assistant Professor, Department of Infectious Disease, University of Illinois at Chicago College of Pharmacy
Non-adherence to medication regimens is an important patient safety issue. Adherence to antiretrovirals (ARVs), in particular, is essential to minimizing the risk of developing resistance.1-2 If a patient is non-adherent, they have a proven risk of developing resistance as well as a decreased quality of life and long term survival. This can result in the need for more complicated and expensive regimens and likely increase the cost of medical care for these individuals. Having medications refilled on time is critical for maintaining adherence; therefore it is imperative that patients receive their ARVs on time every month.
The University of Illinois at Chicago (UIC) – HIV Clinics care for ~1300 patients with 20-30% of patients being uninsured and from low-income households. Many are homeless. With this unique population, the pharmacists at UIC work diligently to ensure that the patient is able to receive their necessary ARVs on time. Therefore, before initiating ARVs, the uninsured patient is first enrolled in a reliable program that will ensure uninterrupted coverage. Typically this requires patients to enroll in the Illinois AIDS Drug Assistance Program (IL-ADAP) and/or Patient Assistance Programs funded by a pharmaceutical company.3
IL-ADAP serves over 4,000 patients monthly.3 The process for applying can be quite cumbersome and is a barrier to treatment. The program has multiple requirements, including an online application to be completed every six months, proof of income, proof of residency, HIV laboratory results, and other demographic and health information. Most patients do not have internet access, and due to their unstable living situation may not have the documents required for proof of residency or proof of income. Therefore, the pharmacist often assists in completing the online application and faxing all the appropriate documentation.
For patients recently released from the Illinois prison system, the process to apply for IL-ADAP may take even longer due to the time needed to establish residency and obtain a state ID. Illinois prisoners who were on ARVs while incarcerated are typically released with one month of ARVs but it usually takes about three months for these patients to have all the necessary documents required to complete the IL-ADAP application. As a result, they are likely to be without medications for at least two months. Nonetheless, as soon as a patient’s IL-ADAP application is approved, the pharmacist will call in their prescriptions to CVS Caremark in Pittsburgh and arrange for deliveries. The pharmacist also confirms and coordinates monthly deliveries thereafter.
Another barrier to implementation is that IL-ADAP informs patients that they are due for renewing their application by mail to the address listed on their most recent IL-ADAP application. This assumes that IL-ADAP has the patient’s most updated address. For a low-income population this is rarely the case, and many patients only find out that they need to re-apply when their prescriptions are no longer being filled. If the IL-ADAP benefits expire, the patient may be without medications for two months. Again, this increases the likelihood of resistance and the need to initiate a new and more expensive and complicated regimen.4
In order to limit the interruptions in their ARVs, the UIC-HIV Clinic pharmacists make a concerted effort to ensure the patients are aware of their IL-ADAP status by discussing it at their clinic visits. Patients meet with the pharmacists on a weekly, bi-weekly, or monthly basis to assess adherence and tolerance to ARVs and to pick up their pillboxes or the monthly ARV delivery from CVS Caremark. Since many of the patients do not have internet access, the pharmacist assists in completing the online application and faxing all of the appropriate documentation. If a patient is unaware of their IL-ADAP status, the pharmacist investigates if they are due for approval and completes their application. In order to minimize the risk of ARV interruptions when there is a lapse in IL-ADAP, the pharmacists will complete patient assistance applications and coordinate the delivery of ARVs to clinic within days of the application.
Of note, the patient’s individual ability to be adherent to their medication is of utmost importance. Therefore, if the patient’s adherence ability is questionable, the time between IL-ADAP submission and approval is spent assisting the patient in developing ritualistic adherence to a placebo using pillboxes, alarms, and other adherence improving techniques. This practice ensures that by the time the patient has IL-ADAP approval they have either increased their adherence potential tremendously, or have shown an inability to be adherent and continue to require adherence training prior to beginning their regimen.
Ultimately, it is with the assistance of the UIC pharmacists in the HIV clinics that many of the patients are able to complete and renew their IL-ADAP applications on-time every six months. In doing so, patients are assured that they will be able to safely continue on the same regimen with an increased adherence potential and decreased likelihood of resistance.
References
- Chesney MA. The elusive gold standard. Future perspectives for HIV adherence assessment and intervention. J Acquir Immune Defic Syndr. 2006;43 149-155
- World Health Organization (WHO). Adherence to long term therapies – evidence for action. 2003.
- Illinois Department of Public Health: AIDS Drug Assistance Program. http://www.idph.state.il.us/health/aids/adap.htm [Accessed September 23, 2011]
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. January 10, 2011; 1-166.
Board of Pharmacy Update
Highlights from the March Meeting
by Scott A. Meyers, Executive Vice President
The March 12th Board of Pharmacy Meeting was held at the James R. Thompson Center in Chicago. These are the highlights of that meeting.
Pharmacy Prosecutor – Scott Golden, the Department’s lead pharmacy prosecutor, will be leaving sometime near the end of March or early April to take a new position elsewhere in the Department. Scott has been the lead pharmacy prosecutor for several years and has developed a solid relationship with the Board of Pharmacy and a strong knowledge of pharmacy practice. He will be missed, and the Board thanked him for his service.
One Point Patient Care – Representatives of One Point Patient Care requested permission to use remote order processing and automated dispensing and storage systems to service Illinois hospices. One Point Patient Care is a licensed pharmacy currently providing pharmacy services to over 12,000 hospice patients a day around the US from five locations including one located in Illinois. They use an Amerisource Bergen automated system for patients located in hospice facilities. The Department General Counsel responded that rules have not yet been written for this type of patient care but that they are working on them just as they are expanding the use of automated dispensing and storage systems for use in long-term care.
FDA Inspections – The Department staff informed the Board that the FDA is now inspecting any pharmacy that has indicated it provides sterile compounding services to other pharmacies in Illinois. IDFPR investigators have been invited to participate in these inspections which have been extremely thorough, taking up to four days on site of each pharmacy. The FDA has offered to provide lab testing services to IDFPR staff when needed and will assist in any manner requested.
Pharmacy Student/Technician License Renewal – All of the Colleges of Pharmacy have identified a variety of issues with student pharmacist license renewals again this year. After their initial year in pharmacy school, students are directed by their respective schools to obtain Student Pharmacist registrations so that they may experience a wider variety of tasks and responsibilities as part of their experiential training. However, many students requesting student pharmacist designation for the first time have been denied with no apparent reason and some renewing their student pharmacist registration have been sent pharmacy technician or certified pharmacy technician registrations instead. There was a high level of frustration expressed from representatives of the colleges and the Department staff will fully investigate. In the meantime, all pharmacy directors are urged to verify that their pharmacy technicians have obtained the appropriate registration and that all certified pharmacy technicians can provide proof of certification from the certifying agency (PTCB, etc.). Reports of pharmacy technicians receiving certified pharmacy technician registrations without proof of certification have been received and investigators will be checking these credentials during any visits to pharmacies in the future.
Impaired Pharmacist Program – A question was raised at the January meeting of the Board as to what services are paid for by the State when a pharmacist or pharmacy technician enters the Illinois Professionals Health Program for a substance abuse issue. The State contract with IPHP pays for the initial assessment/intervention, case management services, and one drug screen per month. It does not cover psychological treatment or drug screen costs if more than one per month is ordered. These additional costs place a hardship on the effected pharmacist or technician but taking responsibility for the costs is part of the process of taking responsibility for the situation. In addition, the State would have to raise license and registration fees if more services were to be picked up by the State.
Commencement Date vs. Meeting Graduation Requirements – A concern was raised that Continental Testing (the company the State outsources its testing registration process to) is not allowing some graduates to register for the NAPLEX exam until after their graduation date has passed. The statute allows students to register for the examination up to six months prior to graduation as long as the College of Pharmacy certifies that graduation is expected. IDFPR staff will communicate with Continental Testing to clarify this issue.
Legislative Update – Scott Meyers of ICHP provided the Board of Pharmacy with an update of pharmacy-related legislation being considered by the Illinois General Assembly this spring. A list of the most important bills is provided in this month’s issue of “The GAS From Springfield”.
Next Board of Pharmacy Meeting – Is scheduled for Tuesday, May 14th at 9:30AM on the 9th floor of the James R. Thompson Center in downtown Chicago. Pharmacists, pharmacy students and pharmacy technicians are welcome to attend the open portion of the meeting.
Hi-Tech
Important Info from PTCB
PTCB Extends March 2013 Recertification Deadline until April 30
by: PTCB Staff | Mar 14, 2013
Certified Pharmacy Technicians (CPhTs) due to recertify by March 31, 2013 will remain in “active” status during April, and automatically receive an additional 30 days, until April 30, to submit their recertification applications. Higher than anticipated traffic has caused response times to be inconsistent. PTCB is working continually across multiple fronts to improve system performance. While many CPhTs with the March 2013 recertification deadline have successfully submitted their applications, some users need extra time.
Please note that in the subsequent two-year recertification cycle, recertificants in this group will be expected to recertify by March 31, 2015, rather than April 30, 2015.
PTCB assures our CPhTs, and those applying for certification for the first time, that we are here to support you. This one-month deadline extension is automatic, and there is no need to apply for it.
Letter to employers explaining the deadline extension.
Important Notice About Reinstatement
Reinstatement candidates in this cycle (those who did not recertify before their expiration date in March of 2012) are still subject to their March 31, 2013 deadline to apply for reinstatement.
Taken directly from http://ptcb.org/about-ptcb/news-room/news-landing/2013/03/14/ptcb-extends-march-2013-recertification-deadline-until-april-30#.UUODdFciHd4
PTCB Announces Certification Program Changes
by PTCB Staff | Feb 27, 2013
WASHINGTON, DC — The Pharmacy Technician Certification Board (PTCB) announces future changes to the PTCB Certification Program. The new changes will advance pharmacy technician qualifications by elevating PTCB’s standards for national certification and recertification. During the next seven years, PTCB will phase in the changes, including mandatory background checks, accredited education requirements, and changes in acceptable continuing education (CE) programs for recertification.
“PTCB is elevating our certification requirements in order to meet the demands of the evolving healthcare system,” said PTCB Executive Director and CEO Everett B. McAllister, MPA, RPh. “We have made bold decisions on what will be required for candidates to become certified pharmacy technicians (CPhTs). Our Board of Governors is sharply focused on ensuring that the PTCB Program prepares CPhTs for the integral roles they play in supporting pharmacists in all practice settings.” PTCB’s requirements have remained largely unchanged since the organization’s founding in 1995.
The PTCB Board of Governors decided that new candidates for PTCB certification will be required to complete criminal background checks, beginning in, or around, 2014. Many employers already require background checks as a condition of employment, and PTCB plans to collaborate with stakeholders to synchronize with the existing systems.
As part of the 20 hours of CE required for recertification, individual CPhTs will need to complete one hour of medication safety CE, effective in 2014, in addition to the one hour of law CE already required. By 2015, PTCB will require all 20 recertification CE hours to be pharmacy technician-specific. Many existing CE offerings already fit this definition. The allowable CE hours from college courses will be reduced from 15 to 10 by 2016, and allowable in-service hours will be phased out by 2018.
By 2020, PTCB will require candidates for initial PTCB certification to successfully complete an American Society of Health-System Pharmacists (ASHP)-accredited education program. ASHP-accredited programs include didactic course work and practical experience, thereby providing well-rounded training for technicians.
Beginning today, PTCB is conducting a 90-day open, online comment period at www.ptcb.org to allow members of the pharmacy community to share best practices for implementing the new requirements. PTCB intends to begin releasing the policies and procedures regarding the implementation of these decisions later this year.
These program changes are the result of a PTCB initiative which began with a 2011 summit focused on five areas related to pharmacy technicians: Consumer Awareness, Resources, Education, State Policy and Testing (C.R.E.S.T.). Summit attendees included pharmacists, certified pharmacy technicians (CPhTs), educators, major employers, state boards of pharmacy, and others. Summit findings, combined with results from two profession-wide surveys, called for PTCB and the pharmacy profession to make decisive changes in certification standards.
Visit www.ptcb.org for more information on the certification program changes.
Taken directly from http://www.ptcb.org/about-ptcb/news-room/news-landing/2013/02/27/ptcb-announces-certification-program-changes#.UT4duFciHYg
College Connections
Celebrating Poison Prevention Month
by Joanna Kasper, P-2, SSHP Student President, and Vy Tran, P-2, SSHP Philanthropy Chair, Rosalind Franklin University of Medicine and Science College of Pharmacy
 March is Illinois Poison Prevention Month and Rosalind Franklin University SSHP chapter is honoring this event by hosting a variety of educational initiatives. In the United States, more than 2 million poisonings are reported each year with more than 90 percent of these occurring in the home.1 For children between the ages of 18-36 months, poisoning is the number one cause of injury-related hospitalization and death.2 Specifically in Illinois there are more people hospitalized for poisonings than for injuries from firearms and motor vehicle collisions combined, and 9 out of 10 deaths due to poisoning are caused by drugs and medications.2 To celebrate Poison Prevention Month, Rosalind Franklin University SSHP chapter is implementing poison prevention education in the community and at the university.
March is Illinois Poison Prevention Month and Rosalind Franklin University SSHP chapter is honoring this event by hosting a variety of educational initiatives. In the United States, more than 2 million poisonings are reported each year with more than 90 percent of these occurring in the home.1 For children between the ages of 18-36 months, poisoning is the number one cause of injury-related hospitalization and death.2 Specifically in Illinois there are more people hospitalized for poisonings than for injuries from firearms and motor vehicle collisions combined, and 9 out of 10 deaths due to poisoning are caused by drugs and medications.2 To celebrate Poison Prevention Month, Rosalind Franklin University SSHP chapter is implementing poison prevention education in the community and at the university.

The inaugural class in the college of pharmacy, along with the first year students, reached out to the Neal Math and Science Academy in North Chicago to participate in their health fair. Our pharmacy students focused on educating children and their parents about poison prevention in fun, interactive ways. Games were played including “pill vs. candy” where participants attempted to identify which look-alikes were medications and which were candy. Many parents and children could not believe how difficult it was to distinguish between the two. One mother shared her personal story about a trip to the grocery store; while shopping she saw her daughter eating something that had fallen on the floor. Upon investigating it turned out to be an over the counter medication that her daughter mistook for candy. She was taken to an emergency department where she was examined and treated and is fine today. Additional poison prevention lessons were presented including information to help identify potentially hazardous items around the home. Information on emergency care for babysitters, poison control center pamphlets, telephone stickers, and magnets were distributed. The day was fun, interactive and a great success with very positive feedback. All of these activities will be repeated at Rosalind Franklin University for faculty, staff, and students during National Poison Prevention Week, March 17th – 23rd.
It is important to preserve the services provided by poison control centers with government funding. The Illinois Poison Center is a non-profit center serving one of the largest populations in the nation; there are an estimated 12.9 million Illinois residents and the IPC annual call volume exceeds 80,000.2 It is estimated that for every $1 that is invested in the center there is $13 saved in reduced health care costs. With these facts in mind please consider contacting your local, state, and national representative to support funding for poison control centers in the United States. Visit the poison centers website, www.illinoispoisoncenter.org to see how you can help.
References:
- Poison Prevention Week Council. Poison Prevention.org. Available at:
http://www.poisonprevention.org/index.htm Accessed: March 1st 2013. - Illinois Poison Center. Illinois Poison Prevention Month. Available at:
http://illinoispoisoncenter.org/IPPMAccessed: March 2nd 2013.
The Importance of Quality in Saving the Lives of Crickets Everywhere
by Jacob Sicinski, ICHP Student Chapter Treasurer, University of Illinois at Chicago
It is that time of year again, the time of year where consumers flock to the pharmacy to stock up on cough medicine and nasal decongestants. It is the dreaded flu season. A cold had been going around my extended family during Christmas, so I was unfortunate enough to catch it a few days later. I ventured over to my local pharmacy to purchase some cold relief medication, and then I went home to take some of the medication and try to sleep off the worst of the cold. I am not one to check the medication for quality control and uniformity, especially in the state I was in, but I wish that I had checked the packaging. It was not until I reached for my third dose a day later that I found every pharmacist’s, company’s, and consumer’s worst nightmare. I found a dead, smashed cricket in the blister packaging of my medication.
Luckily I had not taken any of the medication that was nestled next to the remains of my dear cricket friend, but the damage was done. I contacted the FDA with the appropriate information about the product with pictures, and I decided it was time to just let my cold run its course without any other type of intervention.
This incident is a prime example of what problems and errors pharmacists can experience in community, hospital, and industry settings. There seemed to be a lapse in Good Manufacturing Practice (GMP) in the company’s packaging facility and a product recall will most likely cause them a huge loss of revenue, consumer confidence, and possibly licensing problems.
Company GMP errors can be compared to a pharmacist’s errors, but they are more detrimental in scale. For a pharmacist, an unfortunate mistyping of PRN to PR can change “as needed” to “by rectum” and possibly cause one patient harm or discomfort. However, for a company, a GMP error can affect the lives of thousands. Take the New England Compounding Center, for example, whose epidural steroid injections were responsible for fungal infections and deaths of 44 patients. This case seemed to be an eye-opener for consumers across the country, and Massachusetts responded by performing surprise inspections of compounding pharmacies, which resulted in closing of a few of them for sterility issues.
The fact is, we’re all human. Everyone makes mistakes. However, a pharmacist’s mistakes can cause harm or distress to patients. Sometimes a pharmacist just needs to take a step back, take a deep breath, and focus on the task at hand. It can not only save the company possible legal trouble and the pharmacist his or her license, but it can also save a patient from possible harm. If only the person in charge of the company’s packaging facility had been more aware of the manufacturing process (not to mention GMP), then the life of that poor cricket might have been saved.
Brown Bag Medication Review – An Overview and Planning Guide
by Vincent Tam, PS-3, ICHP Philanthropy Chair, and Josephine Aranda, PS-3, Midwestern University Chicago College of Pharmacy
 On Feb 7, 2013, the Midwestern University Chicago College of Pharmacy ICHP Philanthropy Committee hosted a brown bag medication review event at Mayslake Village, an assisted living center in Oakbrook, IL. Members from the American Society of Consultant Pharmacists (ASCP) were also present to discuss Fall Prevention Initiatives. Ten student pharmacists volunteered for this event and worked under the supervision of three mentor pharmacists. Over the course of 2 hours, the student pharmacists were able to provide thorough medication reviews for seven patients. In addition, an informational booth was also set-up to check patients in, answer questions, and provide education regarding medication safety and the role of pharmacists as medication experts. This event was also used for Script Your Future – a campus wide event promoting the importance of medication adherence.
On Feb 7, 2013, the Midwestern University Chicago College of Pharmacy ICHP Philanthropy Committee hosted a brown bag medication review event at Mayslake Village, an assisted living center in Oakbrook, IL. Members from the American Society of Consultant Pharmacists (ASCP) were also present to discuss Fall Prevention Initiatives. Ten student pharmacists volunteered for this event and worked under the supervision of three mentor pharmacists. Over the course of 2 hours, the student pharmacists were able to provide thorough medication reviews for seven patients. In addition, an informational booth was also set-up to check patients in, answer questions, and provide education regarding medication safety and the role of pharmacists as medication experts. This event was also used for Script Your Future – a campus wide event promoting the importance of medication adherence.
Patients brought in their medication bottles and lists to our brown bag event. For each medication, patients were interviewed on how they take it, when they take it, missed doses, and side effects. Medication bottles were also checked for last refilled dates, expiration dates and storage conditions. We attentively addressed concerns, and counseled patients on their medication indications, potential drug interactions and how to manage side effects. After performing medication reconciliation, we were able to create updated medication lists that scheduled the medications by time of day and allowed for additional timing, food, drink and storage instructions. Throughout the sessions, we stressed the importance of medication adherence, keeping updated medication lists, and reaching out to pharmacists to manage their medications.
 Through this successful event we were able to have educational and meaningful interactions with an elderly population in our community. We were able to enhance communication about medications with patients and enhance their relationships with pharmacists. About one week later, we followed up on our patients by sending thank you cards and satisfaction surveys. We look forward to hosting future brown bag events, reaching more patients, and involving greater participation from other school organizations. Based upon our experience, we created a brown bag event planning guide to share with our future members and other student chapters.
Through this successful event we were able to have educational and meaningful interactions with an elderly population in our community. We were able to enhance communication about medications with patients and enhance their relationships with pharmacists. About one week later, we followed up on our patients by sending thank you cards and satisfaction surveys. We look forward to hosting future brown bag events, reaching more patients, and involving greater participation from other school organizations. Based upon our experience, we created a brown bag event planning guide to share with our future members and other student chapters.
Brown Bag Objectives
- Patients bring in all their prescription and OTC medications for review.
- Identify possible drug interactions and adherence problems.
- Look out for expired, duplicate, and poorly stored medications.
- Promote better communication between patients and their health care providers.
Before the Brown Bag
- Find pharmacist mentors to support and guide you in planning and implementing the event.
- Find a venue, date and time for the event. Identify needs in the community.
- Collaborate with other student organizations.
- Recruit student pharmacist volunteers and provide appropriate training session(s)
beforehand. - Create materials specific to your event and make photocopies.
- Collect drug information resources and tools, such as books and software, to use during the event.
Brown Bag Materials
- Patient Consent Form: Inform patient about the purpose of the review, confidentiality, and that the session should be followed up with their pharmacist and physician(s). Collect signature, date, printed name, and contact information.
- Medication List: Blank templates are available from the ASHP website (link also listed below).
- Interview Checklist: Use a checklist as a guide for the interviewer to collect thorough information.
- Informational Pamphlets: Provide pamphlets with medication safety tips and education regarding the roles of a pharmacist.
- Script Your Future Wallet Sized Medication Lists: Card-sized medication lists that promote medication adherence that patients can carry with them at all times.
During the Brown Bag
- Check patients in at an outside booth. Utilize an organized waiting list or number system.
- Provide patients with an anticipated wait time.
- Upon starting a review session, introduce yourself, explain the purpose of the brown bag, and have the patient sign the consent form.
- Collect a brief patient history, allergies, and address any immediate concerns.
- Thoroughly go through each medication. Be sure to use open-ended questions.
- Keep the interaction conversational and flowing. Use the checklist as a guide and to assess for thoroughness of the interview.
- Create an updated mediation list with the patient. Counsel them on their medications, directions, indications, and side effect prevention and management. Assess their understanding and concerns.
- Promote our profession and the importance of compliance and medication safety.
- Refer to pharmacist and drug information.
After the Brown Bag
- Follow up with thank you to patients – phone call, letter or card. Use the contact information provided on the consent form.
- Provide survey with stamped and addressed envelope to solicit feedback.
ASHP Foundation Medication List Template
http://www.ashpfoundation.org/MainMenuCategories/PracticeTools/MyMedicineList
Lung Health Booth at St. Bridget’s Food Pantry
by Nadiyah Chaudhary, P2, President-Elect, UIC College of Pharmacy-Rockford Campus
 As pharmacy students, we continuously hear about interventions pharmacists make that significantly influence patient care. One of the main ways pharmacists are able to influence patient care is through patient education. However, as students, we sometimes lack the confidence to make this type of contribution. The Lung Health Information event at St. Bridget’s Food Pantry provided a unique opportunity for students to interact with patients and promote the profession of pharmacy as future healthcare providers. The Rockford ICHP student chapter, in conjunction with the Christian Pharmacists Fellowship International (CPFI), held a volunteer event at St. Bridget’s Church on December 5th to provide Lung Health education. We chose this location because the St. Bridget’s food pantry provides for underserved members of this community. The purpose of the Lung Health Information clinic was to promote smoking cessation.
As pharmacy students, we continuously hear about interventions pharmacists make that significantly influence patient care. One of the main ways pharmacists are able to influence patient care is through patient education. However, as students, we sometimes lack the confidence to make this type of contribution. The Lung Health Information event at St. Bridget’s Food Pantry provided a unique opportunity for students to interact with patients and promote the profession of pharmacy as future healthcare providers. The Rockford ICHP student chapter, in conjunction with the Christian Pharmacists Fellowship International (CPFI), held a volunteer event at St. Bridget’s Church on December 5th to provide Lung Health education. We chose this location because the St. Bridget’s food pantry provides for underserved members of this community. The purpose of the Lung Health Information clinic was to promote smoking cessation.
Although many students had participated in lung health clinics in the past, this event provided new challenges. Initially, the patrons at the food pantry (our potential patients) seemed reluctant to discuss these issues. Their reluctance may have been due to embarrassment, intimidation, concern for privacy of their health issues, or, possibly the stigma sometimes associated with using a food pantry. Because of these issues, we felt we needed to be more proactive in engaging our potential patients. We decided to roam the pantry and informally introduced ourselves. We explained who we were, and attempted to engage the patrons in short conversations. It was obvious that this was most effective way we could ‘break the ice’ and create an open dialogue regarding lung health.
I quickly realized that many people had concerns other than what medications were available to them. The most common questions asked were the cost of specific medications and how to attain affordable healthcare. I was able to provide information about low-cost clinic options, such as Crusader Community Health, whom many did not know existed.
The main purpose of the event to was to provide Lung Health Information to this underserved community. However, this event provided us, as students, with confidence in our abilities and the opportunity to interact with patients. We are planning to continue working with CPFI and St. Bridget’s Church to provide healthcare to this underserved community in Rockford. We have already begun planning another Lung Health Information clinic at the church in the coming months. This event proved to be beneficial to both the community and the pharmacy students and I hope it becomes an ICHP Rockford tradition.
Although I did not get to make an ‘earth-shattering’ clinical intervention, I did feel this was the first time I made a difference and I can’t wait to do this every day as a pharmacist!
Script Your Future Presentations and Interprofessional Health Fair at Roosevelt University College of Pharmacy
by Diane Cluxton, PS-3, Nathan Fowler, PS-2, Stephen Jankovic, PS-2, Aesha Shah, PS-3, and Tyler Davis, PS-3, Roosevelt University College of Pharmacy
Roosevelt University College of Pharmacy (RUCOP) professional student organizations participated in the Script Your Future (SYF) initiative in February 2013. Planning Script Your Future as a collaborative effort between Student Society of Health-System Pharmacy (SSHP), Academy of Managed Care Pharmacy (AMCP), and American Pharmacist Association Academy of Student Pharmacists (APhA-ASP) was a challenging and rewarding process. The event took approximately four months to plan from conception to completion. Between the three professional organizations, the SYF team consisted of approximately twenty-five student members working closely with faculty advisors, community leaders, and facility management to secure space, funding, materials, supplies, and educational pamphlets. There were schedule conflicts, space availability, and funding challenges that inspired creative and resourceful solutions by the student members and advisors. The end result was worth the numerous planning sessions it took to brainstorm, research, and create seminars that would educate and motivate the community members to sign the medication adherence pledge.
 The SYF team at Roosevelt University delivered two educational seminars. The topics were divided across the organizations to deliver information about heart health, diabetes mellitus, and chronic obstructive pulmonary disease (COPD). The purpose of the seminars was to educate the Institute of Continued Learning (ICL), student population over the age of 55 years at the Schaumburg campus, about some of the chronic disease states and medication adherence. The main purpose of the RUCOP SYF initiative was to educate about medication adherence as it relates to patients with hypertension and cholesterol, diabetes mellitus, and COPD. APhA-ASP student chapter worked on the cardiovascular disease state presentation, SSHP focused on diabetes mellitus, and AMCP on COPD. Each topic was then subdivided and the projects were completed in smaller groups with the overseeing editors tying all the individual pieces of the presentation together. The seminars discussed risk factors, symptoms, management, and medication adherence as related to each of the three disease topics.
The SYF team at Roosevelt University delivered two educational seminars. The topics were divided across the organizations to deliver information about heart health, diabetes mellitus, and chronic obstructive pulmonary disease (COPD). The purpose of the seminars was to educate the Institute of Continued Learning (ICL), student population over the age of 55 years at the Schaumburg campus, about some of the chronic disease states and medication adherence. The main purpose of the RUCOP SYF initiative was to educate about medication adherence as it relates to patients with hypertension and cholesterol, diabetes mellitus, and COPD. APhA-ASP student chapter worked on the cardiovascular disease state presentation, SSHP focused on diabetes mellitus, and AMCP on COPD. Each topic was then subdivided and the projects were completed in smaller groups with the overseeing editors tying all the individual pieces of the presentation together. The seminars discussed risk factors, symptoms, management, and medication adherence as related to each of the three disease topics.The presentation portion of the RUCOP SYF initiative was a challenging and rewarding experience. Due to time and schedule constraints the APhA-ASP students presented on cardiovascular health earlier in February and the SSHP and AMCP student members delivered a combined presentations on the day of the interprofessional health fair. We wanted to make sure that we presented the information in lay language and in a way that the ICL students would remember the importance of medication adherence. One of the ways we were able to achieve this was by encouraging active audience participation. We presented problems and asked the ICL students to participate by sharing some solutions to the problem. We concluded our presentation by having the ICL students share challenges they face when trying to adhere to their medication regimen and came up with solutions to address these challenges. For example, we suggested setting an alarm or placing medications next to the coffee maker to help improve adherence. The ICL students were engaged throughout the presentation and were excited to sign the pledges and implement the many ways we came up with to help them adhere to their medications.
 We also collaborated with students from Harper
College School of Nursing, Dentistry, and Massage Therapy and the Dietetic
Technician program to organize an interprofessional health fair. The health
fair was scheduled in the afternoon following the diabetes mellitus and COPD
seminar. At the health fair, student pharmacists, under the supervision of
faculty members, provided blood pressure screenings, counseled on inhaler technique
and blood glucose monitoring, and medication adherence. The other healthcare
professional students provided counseling on nutrition and dental care, blood
pressure screenings as well as neck and shoulder massages. The SYF initiative allowed
students in the healthcare field to come together interprofessionally to
educate the Roosevelt community about blood pressure, nutrition, dental
hygiene, and how to appropriately check blood glucose and use an inhaler. The
ultimate goal of the seminars and health fair was to encourage the ICL students
and the Roosevelt community to sign a pledge to adhere to their medication
regimens as prescribed.
We also collaborated with students from Harper
College School of Nursing, Dentistry, and Massage Therapy and the Dietetic
Technician program to organize an interprofessional health fair. The health
fair was scheduled in the afternoon following the diabetes mellitus and COPD
seminar. At the health fair, student pharmacists, under the supervision of
faculty members, provided blood pressure screenings, counseled on inhaler technique
and blood glucose monitoring, and medication adherence. The other healthcare
professional students provided counseling on nutrition and dental care, blood
pressure screenings as well as neck and shoulder massages. The SYF initiative allowed
students in the healthcare field to come together interprofessionally to
educate the Roosevelt community about blood pressure, nutrition, dental
hygiene, and how to appropriately check blood glucose and use an inhaler. The
ultimate goal of the seminars and health fair was to encourage the ICL students
and the Roosevelt community to sign a pledge to adhere to their medication
regimens as prescribed.
More
Officers and Board of Directors
TOM WESTERKAMP
President 224-948-1528
tom_westerkamp@baxter.com
CHRIS RIVERS
Immediate Past President
Chairman, Nominations Committee
708-202-7240
criversrx@gmail.com
MIKE FOTIS
President-Elect
michael.fotis@northwestern.edu
MIKE WEAVER
Treasurer
815-599-6113
mweaver@fhn.org
KATHY KOMPERDA
Secretary
630-515-6168
kkompe@midwestern.edu
TRAVIS HUNERDOSSE
Director, Educational Affairs
Travis_Hunerdosse@rush.edu
EDWARD RICKERT
Director, Government Affairs
312-423-9308
erickert@kdlegal.com
JENNIFER ELLISON
Director, Marketing Affairs
Jennifer.C.Ellison@osfhealthcare.org
JENNIFER PHILLIPS
Director, Professional Affairs
Assistant Editor, KeePosted
630-515-7167
jphillips@midwestern.edu
LINDA FRED
Director, Organizational Affairs
217-383-3253
linda.fred@carle.com
ANN JANKIEWICZ
Chairman, House of Delegates
312-942-5706
ann_m_jankiewicz@rush.edu
ELIZABETH ENGEBRETSON
Technician Representative
847-570-4239
EEngebretson@northshore.org
DAVID TJHIO
Chairman, Committee on Technology
816-885-4649
david.tjhio@cerner.com
JENNIFER ARNOLDI
Chairman, New Practitioners Network
JeArnol@gmail.com
JACOB GETTIG
Editor & Chairman, KeePosted Committee
630-515-7324 fax: 630-515-6958
jgetti@midwestern.edu
DESI KOTIS
Regional Director North
312-926-6961
dkotis@nmh.org
MARK LUER
Regional Director South
mluer@siue.edu
SCOTT BERGMAN
Regional Director Central
scbergm@siue.edu
MARC MCDOWELL
President, Student Chapter
University of IL C.O.P.
marc.mcdow@gmail.com
ALEXANDRA HABANEK
Student Representative
University of IL C.O.P.
ahaban2@uic.edu
CHRIS RADUNZ
President, Rockford Student Chapter
University of IL C.O.P.
radunz@uic.edu
AYUMI ODA
President, Student Chapter
Midwestern University C.O.P.
aoda47@midwestern.edu
BRANDON ORAWIEC
President, Student Chapter
Chicago State University C.O.P.
borawiec@csu.edu
KRISTINE MAN LIMOS
Student Representative
Chicago State University C.O.P
KmanLimo@csu.edu
KELCEY CORRELL
President, Student Chapter
Southern Illinois University S.O.P
kelceycorrell@gmail.com
ANTHONY ALBIANI
President, Student Chapter
Roosevelt University C.O.P.
aalbiani@mail.roosevelt.edu
JOANNA KASPER
President, Student Chapter
Rosalind Franklin University C.O.P.
joanna.kasper@my.rfums.org
SCOTT MEYERS
Executive Vice President, ICHP Office
815-227-9292
scottm@ichpnet.org
ICHP AFFILIATES
JENNIFER PHILLIPS
President, Northern IL Society (NISHP)
630-515-7167
jphillips@midwestern.edu
JULIA SCHIMMELPFENNIG
President, Metro East Society (MESHP)
jschimmelpfen@sebh.org
MEGAN METZKE
President, Sangamiss Society
memiller8@yahoo.com
ED RAINVILLE
President, West Central Society (WCSHP)
309-655-7331x
ed.c.rainville@osfhealthcare.org
Vacant Roles at Affiliates —
President, Rock Valley Society; Southern IL Society; Sugar Creek Society
Welcome New Members!

| New Members | Recruiter |
|---|---|
| Ida Chen | |
| Anh Dinh | |
| Wesley Wang | |
| Julie Podlasek | Tamra Holland |
| Ciby Chacko | |
| Michael Kassa | |
| Tihitina Yewondwosen | |
| Jason Alonzo | Kyle Shick |
| Annette Elens | |
| Daniel June | |
| Jeff Gatti | |
| Pavan Surti | |
| Ryan Zimmerman | |
| Tauseef Salim | Bernice Man |
| Mohammed Emaaduddin | |
| Tashel Gandhi | |
| Felix Velazquez | |
| Jill Kellerman | |
| Wuhibeselassie Habte | |
| Zach Olson | |
| Carrie Park | |
| Abdel Bello | |
| Christina Patel | |
| Danielle Cameau | |
| Faisal Khan | |
| Dolapo Ajayi | |
| Inga Aleksonis | |
| Cheryl Hipshur | |
| Lynda Haseltine | |
| Iliana Jacobo | |
| Allison Wright | |
| April Henson | |
| Francis Pham | |
| Haolin Zhang | |
| Nancy Edwards | |
| Damiete Whyte | |
| Abraham Avalos | |
| Florence Emeka | |
| Jennifer Ajide | |
| Tola Omogboyegun | |
| Syed Munawer | |
| Ina Henderson | Norman Garges |
| Melissa Walas | |
| Sarah Schoenherr | |
| Joel Dembosky | |
| Tobias Doherty | |
| Brittany Wiecinski | |
| Jordan Medvid | |
| Grace Cameron | |
| Amy Reznick | Brandon Orawiec |
ICHP PHARMACY ACTION FUND (PAC) Contributors
Contributions listed consist of donations from the past 12 months.
GENERAL ASSEMBLY GUILD - $1000 & More
Dan Ciarrachi
Kevin Colgan
Edward Donnelly
Andrew Donnelly
Dave Hicks
ICHP
James Owen Consulting Inc.
Frank Kokaisl
Scott Meyers
Michael Novario
Michael Rajski
Edward Rickert
Michael Short
Carrie Sincak
Avery Spunt
Michael Weaver
Patricia Wegner
Thomas Westerkamp
SPRINGFIELD SOCIETY - $500-$999
Jered Bauer
Scott Bergman
Ginger Ertel
Kenneth Foerster
Linda Fred
Ann Jankiewicz
Jan Keresztes
Kathy Komperda
Leonard Kosiba
Despina Kotis
Richard Lewis
Huzefa Master
John & Joycelyn McCann
William McEvoy
Anna Nowobilski-Vasilios
Christina Rivers
Miriam Smith-Mobley
JoAnn Stubbings
Cathy Weaver
Paul Zega
CAPITOL CLUB - $250-$499
Sheila Allen
Margaret Allen
Peggy Bickham
Jaime Borkowski
Timothy Candy
Rauf Dalal
Drury Lane Theater
Sandra Durley
Starlin Haydon-Greatting
George MacKinnon
Janette Mark
Heather Minger
Jennifer Phillips
Edward Rainville
Jennifer Rogers
Justin Schneider
Kathryn Schultz
Heidi Sunday
Jill Warszalek
Alan Weinstein
LINCOLN LEAGUE - $100-$249
Tom Allen
Anonymous
Jen Arnoldi
Jerry Bauman
Jill Borchert
Se Choi
Scott Drabant
Nancy Fjortoft
Nora Flint
Michael Fotis
Jacob Gettig
Gireesh Gupchup
Joann Haley
Joan Hardman
Travis Hunerdosse
James Jansen
Vern Johnson
Zahra Khudeira
Mary Lee
John LeGrand
Kristopher Leja
Phyllis Lulinski
George Lyons
Gloria Meredith
MWU COP Student Chapter
Peggy Reed
Katie Ronald
Rochelle Rubin
Don Shadensack
Kristi Stice
GRASSROOTS GANG - $50-$99
Sean Chantraparout
Jordan Cohen
Mark Deaton
Rhonda DePasquale
John Esterly
Lois Honan
Charlene Hope
Diana Isaacs
Gerald Jablonski
Kim Janicek
Dwaine Keller
Colleen Kielch
Kati Kwasiborski
Kim Lim
Mark Luer
Scott Metzger
Shannon Pace
Douglas Shafer
Barbara Smith
Lucas Stoller
Carrie Vogler
Marie Williams
CONTRIBUTOR - $1-$49
Daniel Abazia
Nitika Agarwal
Pat Bagnara
Brett Barker
Elvira Becker
Kathy Brandon
Amanda Bryant
Christina Corcoran
Maricar Curry
Colleen Czerniak
Gabrielle Daniels
Agnes Dominic
Judy Douglas
Jeanne Durley
Kathy Eakright
Karen Eckhart
Lisa Edmond
Lara Ellinger
Jennifer Ellison
Brooke Griffin
Milena Griffith
Susan Hamilton
Eva Hurth
Richard Januszyk
George Jossel
Alex Lomahan
Bella Maningat
Sarah Matias
Ann Marie McDermott
Lindsay McNeely
Virginia Nash
Karen Nordstrom
Walter Ogle
Gopi Patel
Dina Porro
Jeremy Raschke
Jolee Rosenkranz
Jeri Rothman
Mark Ruscin
Ann Ryan
Kim Scarsi
Allison Schriever
Wade Seggerman
Jennifer Splawski
Brandi Strader
Kodanda Uppuluri
Ellen Voelker
Shari Weyland
Laura Woskobnick

