Official Newsjournal of the Illinois Council of Health-System Pharmacists
Spring Meeting Poster Abstracts
Student Research Poster Abstracts
STUDENT RESEARCH POSTER ABSTRACTS
On Site #8 – Student Research
Title: Concurrent use of benzodiazepines and opioids: a drug utilization review-based investigation in a community hospital
Submitting Author: Ashley Riley, PharmD Candidate
Authors: Ashley M. Riley, PharmD candidate, Southern Illinois University Edwardsville; Kristi D. Stice, PharmD, BCPS, Executive Director of Pharmacy and Quality Systems, Decatur Memorial Hospital.
Organization: Southern Illinois University Edwardsville School of Pharmacy
Abstract
Purpose: Concurrent use of benzodiazepines and opioids places patients at increased risk of oversedation. Pharmacists are in a unique position to be able to provide prescribers with drug expertise, contributing to safe and optimal patient care. Through utilization of intervention tools and electronic health system reports, pharmacists can identify patients who are at risk for oversedation events related to concurrent benzodiazepine and opioid therapy. The goal of this retrospective drug utilization review-based quality improvement project is to improve patient outcomes and maximize patient safety related to opioids and benzodiazepines in the hospital setting.
Methods: Drug utilization reports specific to the medical and surgical nursing floors of a single hospital site were obtained. Data collected included the number of patients prescribed opioids and benzodiazepines concurrently, the number of patients prescribed opioids, the number of naloxone reversals in patients prescribed opioids, and the number of pharmacist interventions related to concurrent use. Prescriber and pharmacist education was presented and a report was constructed within the electronic health record system to help pharmacists identify patients on concurrent opioid and benzodiazepine therapy. Pharmacists were educated on how to generate the report and were encouraged to track interventions made addressing concomitant medication orders. Data was collected before and after implementation of the electronic health record report and prescriber education.
Results: A total of 70 patients were on concurrent opioid and benzodiazepine therapy in October 2017. A total of 60 patients were on concurrent opioid and benzodiazepine therapy in November 2017. Concurrent drug utilization decreased in 2018, with records of 51 patients in October and 36 patients in November. The surgical nursing floor had higher incidence of concurrent use compared to the medical nursing floor. A total of 20 pharmacist interventions were recorded in 2018 specific to the surgical nursing and medical nursing hospital floors. A total of 705 patients were prescribed opioids during their hospital stay in 2017 compared to 678 patients in 2018. Naloxone administrations decreased from 6 administrations in 2017 to zero administrations in 2018. Overall, there needs to be more studies conducted to determine the relationship between pharmacist methods of communication for intervention and changes in prescribing patterns.
Conclusions: There was a clinically significant reduction in the number of patients on concurrent opioid and benzodiazepine therapy, which was mirrored by a reduction in naloxone reversals as well. These findings suggest that opioid and benzodiazepine stewardship may play a role in reducing adverse events and increasing patient safety overall.
********************************************************************************************************************
On Site #9 – Student Research
Title: A Retrospective, Single Center Study Evaluating COPD Management and Hospital Readmissions
Submitting Author: Lauren Ballweg, PharmD Candidate
Authors: Lauren Ballweg, PharmD Candidate; Carrie N. Vogler, PharmD, BCPS, SIU School of Medicine.
Organization: Southern Illinois University Edwardsville
Abstract
Purpose: Chronic Obstructive Pulmonary Disease (COPD) contributes to 5% of global deaths and billions in health care spending. The increased attention of health care spending and the push towards value-based services has lead Centers for Medicare and Medicaid Services (CMS) to take a closer look at patients with COPD, and the rates of hospital admissions and readmissions. This shift in focus comes with the intent of improving quality of life, decreasing exacerbations and disease progression, and provides a role for pharmacists to ensure proper medication prescribing and utilization. The GOLD Guidelines provide recommendations for COPD medications throughout different stages of disease progression; initial treatment, step up therapy and exacerbations. The primary objective of this study is to assess the hospital discharge medications for COPD after a hospitalization due to an exacerbation. This study will evaluate the COPD medications used and the recurrence of hospital readmission rates among this population.
Methods: The study was conducted via retrospective chart review of patients admitted to SIU Internal Medicine Hospitalist services at Memorial Medical Center between December 1, 2017 and July 1, 2018. Eligible patients were identified by ICD 10 codes indicative of COPD or acute COPD exacerbation. Once participants were identified the medications used for the management of COPD were assess and compared to the recommendations of the GOLD 2018 Guidelines. Primary outcomes included 30 day all cause readmission rates for patients with documented COPD; COPD medications prescribed at discharge and the appropriateness of dosing compared to GOLD guidelines; and hospitalization due to COPD exacerbation.
Results: Presented at meeting
Conclusions: Presented at meeting
********************************************************************************************************************
On Site #10 – Student Research
Title: Does The Infusion Time of IVIG Matter in Kawasaki Disease?
Submitting Author: Joseph Griffin, PharmD Candidate
Authors: Joseph Patrick Griffin, PharmD Candidate, Chicago State University; Angela Powell, PharmD Candidate, Chicago State University; Shannon Rotolo, PharmD, Clinical Pharmacist, University of Chicago Medicine; Palak Bhagat, PharmD, Clinical Pharmacist, University of Chicago Medicine; Allison Bartlett, MD, Associate Professor Pediatrics, Section of Infectious Diseases, University of Chicago Medicine.
Organization: Chicago State University / University of Chicago Medicine
Abstract
Purpose: Evaluate if there is a difference in the incidence of coronary aneurysms in those who received an Intravenous Immune Globulin (IVIG) 2g/kg dose over 10-12 hours as compared to those who received a dose over less than 10 hours.
Methods: Patients diagnosed and treated for Kawasaki Disease with IVIG at University of Chicago Medicine will be determined by drug utilization reports. The reports will include patients who received IVIG between September 1, 2008 and August 31, 2018. Data will be collected through chart review and patients will be divided into two groups based on duration of infusion (less than 10 hours or 10-12 hours). The primary endpoint will be the incidence of coronary aneurysms. The secondary endpoint will be the resolution time of acute phase reactants and defervescence. The safety endpoints will measure the risk of thrombosis and renal dysfunction.
Results: Presented at meeting
Conclusions: Presented at meeting
********************************************************************************************************************
On Site #11 – Student Research
Title: A comparison of renal outcomes among targeted immunotherapies
Not presented – Results not available at time of meeting.
On Site #12 – Student Research
Title: Analyzing the Role of Pharmacists in Overcoming Inadequate Documentation of Angiotensin Converting Enzyme Inhibitor Induced Drug Reactions in the Electronic Medical Record (Updated title)
Submitting Author: Myesha Tabriz, PharmD Candidate
Authors: Myesha Tabriz, PharmD Candidate, University of Illinois at Chicago (UIC) College of Pharmacy; Reham Awad, PharmD Candidate, University of Illinois at Chicago (UIC) College of Pharmacy; Alvin Godina, PharmD, BCPS, Roosevelt University/Advocate Christ Medical Center; Marc McDowell, PharmD, BCPS, Advocate Christ Medical Center.
Organization: University of Illinois at Chicago College of Pharmacy / Advocate Christ Medical Center
Abstract
Purpose: Angiotensin Converting Enzyme Inhibitor (ACE-I) induced drug reactions such as a dry cough or angioedema are common drug related adverse reactions experienced by patients. Improper documentation of such drug related adverse events, or the lack thereof, may pose severe or life threatening risks to patients if left unnoticed by health care providers. Therefore, the objective was to identify the prevalence of undocumented or inadequately documented ACE-I induced reactions in the banner of the electronic medical record (EMR). Furthermore, the chart review will examine the accuracy of medication induced drug reaction documentation and will assess the role of pharmacists’ in improving proper documentation in the EMR banner.
Methods: The charts of all patients enrolled in the Advocate Christ Medical Center (ACMC) outpatient congestive heart failure (CHF) clinic were reviewed from December 18, 2018 to January 11, 2019. Initially, the patient banner in Cerner PowerChart was assessed for documentation of an ACE-I adverse reaction. Subsequently, the patient chart was reviewed utilizing the “chart search” function with key words such as “ACE-I” for instances of reported ACE-I adverse effects elsewhere in the EMR. The data that was collected included whether or not the patient experienced an ACE-I adverse reaction, whether or not it was documented correctly, and if it was documented by a pharmacist. Correct documentation was assessed based on proper listing of the drug or drug class that caused the adverse effect, followed by what the adverse effect was, and when the adverse effect occurred.
Results: There was a total of 804 patients that were enrolled in the ACMC outpatient CHF clinic that were analyzed in this study. Of the 804 patients, 117 patients had an unintended side effect to an ACE-I such as a dry cough and angioedema. Of the 117 patients, 38 cases had correct documentation of a noted adverse effect to an ACE-I in the banner of the EMR, 39.47% of which were documented by a pharmacist. Additionally, there were 43 cases of inadequate documentation of ACE-I induced adverse reactions with only 9.3% being documented by a pharmacist. Inadequate documentation comprised of an ACE-I reported in the banner as a warning without indicating the adverse reaction that the patient experienced or the onset. Moreover, there were 36 cases of ACE-I induced adverse reactions that were present in the patient’s chart; however, were not documented in the banner. The 36 cases that were not documented in the EMR banner comprise 30.77% of the total allergies that were found among the heart failure patients that were analyzed.
Conclusion: Overall, there is a higher incidence of ACE-I induced adverse reactions that were mis-documented or not documented compared to those that were correctly documented which allows us to conclude that improvements must be implemented in order to achieve proper documentation in the EMR. Unfortunately, there is a lack of available guidelines for proper documentation of allergies and significant adverse reactions within patients’ health record. Therefore, future implications from this study include the standardization of allergy documentation for all healthcare professionals to follow in order to overcome the discrepancy and errors observed in the current system due to the higher incidence of inadequate documentation completed by healthcare professionals outside the field of pharmacy.
Additionally, based on the results, it is evident that pharmacists do not currently play a major role in documentation of drug induced reactions in the EMR. Over the years, pharmacists have gained the role of completing medication reconciliation interviews; therefore, pharmacists’ role should expand to include documentation of patient allergies and drug induced reactions. The role expansion could help overcome issues that were observed in the EMR such as missing information of the drug-induced reaction, time that the reaction occurred, as well as incorrect information being documented under the allergy section of the EMR banner.
If we were to improve the study, a larger population would be analyzed to further solidify our conclusion. Additionally, the data analysis would include the quantification of re-prescribing of an ACE-I in the incidents of correct, incorrect, or mis-documentation as a measure of patient safety. Lastly, the study would further support the need for pharmacists to be responsible for conducting medication reconciliation interviews and documenting it in the EMR. To conclude, this study calls for a standardization of allergy and drug induced reaction documentation as well as the expanded role of the pharmacist in this setting.
********************************************************************************************************************
On Site #41 – Student Research
Title: Nalbuphine as a Primary Parenteral Opioid for Acute Pain in a Large Community Hospital: A Retrospective Review.
Submitting Author: Danielle Vahlkamp, PharmD Candidate
Authors: Danielle Vahlkamp, PharmD Candidate, Southern Illinois University Edwardsville School of Pharmacy; Amanda Daniels, PharmD, BCPS, HSHS St. Elizabeth's Hospital; Chris Herndon, PharmD, FASHP, Southern Illinois University Edwardsville School of Pharmacy.
Organization: Southern Illinois University Edwardsville School of Pharmacy
Abstract
Purpose: To determine if intravenous (IV) nalbuphine could be a reasonable, alternative parenteral analgesic option to treat acute pain in a hospital when compared to first-line pain medications such as intravenous morphine during drug shortages.
Methods: This retrospective chart review occurred at HSHS St. Elizabeth’s Hospital in O’Fallon, IL between January 1, 2018 and June 30, 2018. Patients admitted to HSHS St. Elizabeth’s Hospital who received IV morphine or IV nalbuphine for the treatment of acute pain were included in analysis. The primary outcome was the average pain score during an individual hospital stay. Secondary outcomes consisted of required change in parenteral opioid during hospital stay, opioid presence at admission, change in dose from initiation, delayed discharge due to uncontrolled pain, opioid related adverse effect, and opioid prescription at discharge.
Results: A total of 138 participants were included in the study. Only 123 were included in the primary outcome after 15 were excluded for the utilization of multiple pain scoring systems. Neither the primary outcome nor any of the secondary outcomes were found to be statistically significant, which suggests that there is no difference in efficacy or safety of parenteral morphine and nalbuphine. Although there was not statistical difference between groups in required dose changes, there was a trend toward an increased frequency in the morphine group.
Conclusions: The data suggests that nalbuphine is as effective as morphine for acute pain management in an inpatient setting when parenteral analgesia is required, with no statistical difference in adverse drug reactions, required dose changes, or in adverse drug reactions. Having an option for treating acute pain that would provide equal pain relief as a long-time, first-line agent while having less frequent and severe side effects could be clinically significant. However, larger, more detailed studies are needed.
********************************************************************************************************************
On Site #42 – Student Research
Title: Dispense this, not that! Requirements for confident opioid dispensing
Submitting Author: Ashley Riley, PharmD Candidate
Authors: Ashley M. Riley, PharmD Candidate, Southern Illinois University Edwardsville; Katrina A. Trentham, PharmD Candidate, St. Louis College of Pharmacy; Nicole M. Gattas, PharmD, BCPS, FAPhA, Associate Professor of Pharmacy Practice, St. Louis College of Pharmacy; Amy M. Tiemeier, PharmD, BCPS, Director, Community Partnerships & Associate Director, Experiential Education & Associate Professor, Pharmacy Practice, St. Louis College of Pharmacy; Halvor T. Olsen, PharmD, Pharmacy Clinical Services Manager, Walmart Health and Wellness; Amy E. Bias, PharmD, Pharmacy Clinical Services Manager, Walmart Health and Wellness; Chris M. Herndon, PharmD, BCACP, Professor, Pharmacy Practice, Southern Illinois University Edwardsville School of Pharmacy.
Organization: Southern Illinois University Edwardsville School of Pharmacy
Abstract
Purpose: As opioid overdose deaths continue to rise across the United States, healthcare providers are taking action to recognize and combat this crisis. Pharmacists play a key role in opioid stewardship, with prescriber and pharmacist communication essential in satisfying corresponding responsibility. This survey aims to identify key information necessary for pharmacists to confidently and responsibly dispense prescribed opioid medications in accordance with laws, policies, and professional judgement. Once identified, key information could be formatted into a universal form or checklist for use by prescribers and pharmacists. A universal tool would improve interdisciplinary communication, reduce patient care delays, promote safe and effective use of opioids, as well as in overall improved patient outcomes. 2.
Methods: The Dispense this, not that! Requirements for confident opioid dispensing survey is a 16-item survey tool (Qualtrics, Provo, Utah, USA) that was distributed electronically to members of the Illinois Pharmacists Association (IPhA) and Missouri Pharmacy Association (MPA) in late 2018. Participation was voluntary and anonymous. The survey questions were designed to identify key information perceived as necessary for pharmacists to confidently dispense opioid prescriptions, as well as information regarding demographics, work setting, location, and general knowledge. The Institutional Review Boards of both Southern Illinois University Edwardsville and St. Louis College of Pharmacy approved the study.
Results: A total of 274 surveys were submitted from members of the Illinois Pharmacists Association and Missouri Pharmacy Association. The majority of pharmacists (greater than 50% of respondents) reported dispensing opioids without the following information: diagnosis, diagnosis code, prior pharmacologic and nonpharmacologic treatment attempted, patient reported pain severity, past medical history, and previous treatment trials with opioids. Information that was deemed not necessary for dispensing opioids by the majority of respondents was patient family history and patient imaging. The majority of respondents deemed the last fill date of any opioid for the patient and confirmation that the prescription drug monitoring database had been reviewed by the prescriber or prescriber’s agent as information that should be required documentation for all opioid prescriptions.
Conclusions: Our findings suggest that, ideally, pharmacists would require documented information from prescribers that is not currently mandated to be on opioid prescriptions. There needs to be improvements in prescriber and pharmacist communication regarding opioid prescriptions in order to satisfy corresponding responsibility, improve patient safety, and improve pain management.
********************************************************************************************************************
On Site #43 – Student Research – Winner Best Student Poster
Title: A Retrospective, Single Center Study Evaluating Readmission Rates and Medications for Patients with Heart Failure with Preserved Ejection Fraction
Submitting Author: Troy Kramer, PharmD Candidate
Authors: Troy Kramer, PharmD candidate; Carrie Vogler, PharmD, Southern Illinois University Edwardsville School of Pharmacy; Mukul Bhattarai, MD, Memorial Medical Center; Robert Robinson, MD, Memorial Medical Center.
Organization: Southern Illinois University Edwardsville
Abstract
Purpose: Heart failure with preserved ejection fraction (HFpEF) has significantly less guideline driven treatment options compared to hearth failure with reduced ejection fraction (HFrEF). This stems from a lack of trials demonstrating medications with improved clinical outcomes for this patient population. The primary objective of this study is to determine which medications and dosages are related to readmission rates for HFpEF patients.
Methods: A retrospective, single center, chart review was performed on patients with HFpEF at an academic medical center. The study was approved by the institution’s IRB. Heart failure patients between the ages of 18-89 with an ejection fraction ≥45% reported on an ECHO were included in the study. Demographic data was also collected. Primary outcomes include 30 day all cause readmission rates along with 30, 60, and 90 day heart failure related readmission rates. Other primary outcomes include prescribing patterns of heart failure medications at discharge and medications prescribed that could be potentially harmful medications in patients with heart failure. Secondary outcomes include patient safety by comparison of readmission rates. Descriptive statistics will be used to analyze the data.
Results: Presented at meeting
Conclusion: Presented at meeting
********************************************************************************************************************
On Site #44 – Student Research
Title: Acute pain management for patients with an opioid dependence disorder receiving Suboxone, naltrexone or methadone
Submitting Author: Erin Lindstrom, PharmD Candidate
Authors: Carrie N. Vogler, PharmD, BCPS, Clinical Associate Professor, Southern Illinois University Edwardsville School of Pharmacy; Katelyn Conklen, PharmD, BCPS, Clinical Pharmacist, Memorial Medical Center; Erin M Lindstrom, PharmD candidate.
Organization: Southern Illinois University Edwardsville School of Pharmacy
Abstract
Purpose: Opioid dependence disorders are treated with medications that alter the opioid receptor response to the offending agents. These actions are desirable for preventing opioid abuse but complicate the treatment for acute pain episodes. The purpose of this study it to determine how acute pain is being treated in this population.
Methods: A retrospective chart review at a non-profit academic medical center was conducted from 3/31/2015 to 3/31/2018 and approved by the institutional review board. Patients admitted to the hospital that are 18-89 years old experiencing acute pain and receiving Suboxone (buprenorphine/naloxone), naltrexone, or methadone for the indication of opioid dependence disorder will be included in this study. Patients on hospice will be excluded. Data will be collected regarding age, gender, reason for hospital admission, significant social history, significant medication history, significant past medical history, opioid dependence therapy, adjuvant therapy used, discharge medications, pain scores and the amount of daily oral morphine milligram equivalents (MME) received. The primary outcomes include type and amount of medication used for inpatient pain management. Safety outcomes include naloxone use, any respiratory rate less than 8 breaths per minute, and daily MME above 50 mg or 90 mg.
Results: Presented at meeting
Conclusion: Presented at meeting
********************************************************************************************************************
On Site #45 – Student Research
Title: Application of the Utah Bleeding Risk Score to LVAD Supported Patients at Advocate Christ Medical Center: A Retrospective Study (Updated title)
Submitting Author: Andrew McInerney, BS, PharmD Candidate
Authors: George Gavrilos, PharmD, MA, Advocate Christ Medical Center; Tatyana Lawrecki, PharmD, BCPS, Advocate Christ Medical Center; Krystina Chickerillo, FNP, ACNS-BC; Nora Krause, FNP, ACNS-BC; Tracy Aicher, FNP, ACNS-BC; Nicole Graney, ACNS-BC; Andrew McInerney, BS, PharmD Candidate, University of Illinois at Chicago College of Pharmacy; Marc McDowell, PharmD, BCPS, Advocate Christ Medical Center; Devin Mehta, MD, Advocate Christ Medical Center; Muhyaldeen Dia, MD, Advocate Christ Medical Center.
Organization: Advocate Christ Medical Center
Abstract
Purpose: Continuous-flow left ventricular assistant devices (CF-LVAD) have improved survival rates in advanced heart failure patients; however, gastrointestinal (GI) bleeding is commonly seen post-implant, resulting in further health complications, increased healthcare expenses, and increased mortality. Recently, researchers at the Utah Transplantation Affiliated Hospitals program developed the Utah Bleeding Risk Score (UBRS) to estimate bleeding risk in this patient population (Yin, et al.). Their study identified seven pre-implant variables most predictive for post-implant GI bleeding. The aim of this study is to evaluate CF-LVAD patients at Advocate Christ Medical Center (ACMC) who have experienced bleeding post-implant and apply the UBRS tool to this patient population.
Methods: CF-LVAD recipients (all devices) at ACMC between 2012 and 2017 who experienced post-implant GI bleeding were evaluated. The following variables were assessed, and patients were assigned one or two points for: age >54 years (1 point), history of previous bleeding (2 points), coronary artery disease (1 point), chronic kidney disease (1 point), severe right ventricular dysfunction (1 point), mean pulmonary artery pressure <18 mm Hg (2 points), and fasting glucose >107 mg/dL (1 point). The risk of each patient having a GI bleed post-implant was then applied using the UBRS, defined as: low (0–1 points), intermediate (2–4), and high risk (5–9). Corresponding 3-year GI bleeding rates found by Yin and colleagues were 4.8%, 39.8%, 83.8% in each risk group respectively.
130 of 562 (23.1%) patients implanted with a CF-LVAD from January 2012 – December 2017 experienced at least one episode of post-implant GI bleeding. Variables assessed are listed below:
Variable |
Results N=130 (%) |
Age >54 |
114 (87.7) |
History of Previous Bleeding |
20 (15.4) |
Coronary Artery Disease |
77 (59.2) |
Chronic Kidney Disease |
31 (23.8) |
Severe Right Ventricular Dysfunction |
3 (2.3) |
Mean Pulmonary Artery Pressure <18 mmHg |
7 (5.4) |
Fasting Glucose > 107 mg/dL |
85 (65.4) |
Utah bleeding scores are listed below:
Risk Score |
Results N=130 (%) |
Low (0–1 Points) |
14 (10.7) |
Intermediate (2–4 Points) |
99 (76.2) |
High (5–9 Points) |
17 (13.1) |
The mean UBRS was 2.83.
Conclusions: Yin and colleagues found the UBRS to be a simple predictive model based on pre-implant clinical factors that can effectively risk stratify CF-LVAD patients based on their probability of GI bleed. In their study, they observed an intermediate risk of GI bleed in all CF-LVAD supported patients based on UBRS. In the subset of CF-LVAD supported patients at ACMC who experienced a post-implant GI bleed, the same intermediate risk probability was observed. Yin’s study found a three-year, 39.8% risk of GI bleed post-implant for intermediate risk patients, and while a direct correlation cannot be made between our two patient populations at this time, we observed a 23.1% overall incidence of post-implant GI bleeding in CF-LVAD supported patients over a five-year period, the majority (76.2%) of whom were found to be at intermediate risk. Prospective, multicenter validation studies should be conducted to further elucidate the accuracy and usefulness of this tool in clinical practice.
********************************************************************************************************************
On Site #46 – Student Research
Title: Rocuronium versus succinylcholine in the traumatically injured brain: A prospective observational cohort (RVSTIB)
Submitting Author: Ammarah Nadeem, PharmD Candidate
Authors: Ammarah Nadeem, PharmD Candidate, Advocate Christ Medical Center; Chuxian Tang, PharmD Candidate, Advocate Christ Medical Center; Samson Tang, PharmD Candidate, Advocate Christ Medical Center; Marc McDowell, PharmD, BCPS, Advocate Christ Medical Center; Sabrin Jaber, PharmD, Advocate Christ Medical Center.
Organization: Advocate Christ Medical Center
Abstract
Purpose: According to the Centers for Disease Control and Prevention, there were approximately 2.8 million traumatic brain injury (TBI)-related emergency department (ED) visits in 2013. Patients with a TBI require rapid sequence intubation (RSI) to prevent hypoxia and death. A recent retrospective study suggests that the use of succinylcholine in patients with severe TBI is associated with increased mortality. However, due to rocuronium’s longer duration of action compared to succinylcholine, this may obscure neurological examination or delay treatment for seizure potentially leading to worse outcomes. This study aims to evaluate the incidence of mortality in patients with a TBI after being administered succinylcholine or rocuronium. (104).
Methods: This is a prospective, single center observational study performed at a large tertiary community teaching hospital in patients greater than 18 years of age presenting with a traumatic brain injury (TBI) requiring rapid sequence intubation (RSI) in the emergency department (ED). Patients who received more than one paralytic or received a paralytic other than rocuronium or succinylcholine for the purpose of RSI, had a surgical airway placed, were< 18 years of age, pregnant, sustained an in-hospital or out-of-hospital cardiac arrest prior to intubation, or had an attempt to intubate outside the ED were excluded. The primary outcome of this study is incidence of mortality. The following data points will be collected: age, sex, race, height, weight, pre-intubation Glasgow Coma Score, baseline serum creatinine and potassium, type of traumatic head injury (defined as blunt or penetrating), mechanism of injury, additional injuries, number of intubation attempts, pre-intubation vitals (oxygen saturation, systolic and diastolic blood pressure, and heart rate), sedative induction agent and dose used for RSI, paralytic agent and dose used for RSI, incidence of mortality, total length of stay (LOS), intensive care unit LOS, type of intracranial injury (defined as: subarachnoid hemorrhage, subdural hematoma, epidural hemorrhage, or intraventricular hemorrhage), presence of mid-line shift, mass effect, or skull fracture, and history of anticoagulant or antiplatelet use. Data will be collected without patient identifiers and analyzed using descriptive statistics. (226).
Results: Out of ten total patients, six were administered succinylcholine and four were administered rocuronium. The incidence of in-hospital mortality was similar in both groups (33% vs 54%, p=0.54). Succinylcholine was associated with a non-significant increase in hospital (6.5 vs 1.8, p=0.10) and ICU LOS (14.8 vs 4.8, p=0.17). (48).
Conclusion: In TBI patients, there is no difference between rocuronium and succinylcholine in the incidence of in-hospital mortality when used for RSI. There was also no difference between groups in ICU or hospital LOS. Larger studies are required in order to meet power and determine significance. (45).
********************************************************************************************************************
On Site #47 – Student Research
Title: Diluted single-syringe administration of adenosine for the rapid conversion of supraventricular tachycardia in the Emergency Department
Submitting Author: Alexandria Nudo, PharmD Candidate
Authors: Alexandria Nudo, PharmD Candidate, Advocate Christ Medical Center; Kevin Johns, PharmD Candidate, Advocate Christ Medical Center; Sonal Sahni, PharmD Candidate, Advocate Christ Medical Center; Robert Mokszyck, PharmD, BCPS, Advocate Christ Medical Center; Neal Lyons, PharmD, BCPS, Advocate Christ Medical Center; Allyson Greenberg, PharmD, BCPS, Advocate Christ Medical Center; Mary Hormese, PharmD, BCPS, Advocate Christ Medical Center; Marc McDowell PharmD, BCPS, Advocate Christ Medical Center.
Organization: Advocate Christ Medical Center
Abstract
Purpose: Supraventricular tachycardias (SVT) are a common cause for emergency department visits. Adenosine is an effective treatment to abate SVT, however differing methods exist for administration. No studies have prospectively evaluated differing methods of administration in a large number of patients. To evaluate the efficacy of adenosine in a single-syringe diluted with normal saline compared to the standard two-syringe method for rapid conversion of SVT to normal sinus rhythm.
Methods: A single center, prospective, observational study was conducted from November 1, 2016 through February 28, 2018 on patients presenting to the emergency department in SVT treated with adenosine. Drug was prepared by the pharmacist and method of administration was at the preference of the physician. Adenosine was either prepared as a single-syringe combined with a 0.9% NaCl flush to a total of 20ml or as the conventional two separate syringes. Rates of conversion from SVT to normal sinus rhythm were recorded.
Results: Presented at meeting
Conclusions: Presented at meeting
Contents
Columns
March Board of Pharmacy Update
Collaborative Pharmaceutical Task Force Deliberations (March 2019)
Collaborative Pharmaceutical Task Force Deliberations (April 2019)
ICHP Leadership Spotlight Interview - Alifiya F. Hyderi, PharmD
ICHP Leadership Spotlight Interview - Jared Sheley, PharmD
Features
Student Chapter Video Contest 2019
Spring Meeting Platform Presentations
Spring Meeting Poster Abstracts
Spring Meeting Poster Abstracts
Spring Meeting Poster Abstracts
College Connection
Chicago State University College of Pharmacy
Midwestern University Chicago Collge of Pharmacy
Roosevelt University College of Pharmacy
Rosalind Franklin University College of Pharmacy
Southern Illinois University Edwardsville School of Pharmacy
University of Illinois at Chicago College of Pharmacy
More
ICHP Pharmacy Action Fund (PAC)
Regularly Scheduled Network Meetings
Chicago Area Pharmacy Directors Network Dinner
3rd Thursday of Odd Months
5:30pm
Regularly Scheduled Division and Committee Calls
Executive Committee
Second Tuesday of each month at 7:00 p.m.
Educational Affairs
Third Tuesday of each month at 11:00 a.m.
Government Affairs
Third Monday of each month at 5:00 p.m.
Marketing Affairs
Third Tuesday of each month at 8:00 a.m.
Organizational Affairs
Fourth Thursday of each month at 12:00 p.m.
Professional Affairs
Fourth Thursday of each month at 2:00 p.m.
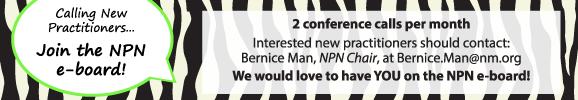
New Practitioner Network
Second Thursday of each month at 5:30 p.m.
Technology Committee
Second Friday of each month at 8:00 a.m.
Chicago Area Pharmacy Directors Network Dinner
Bi-monthly in odd numbered months with dates to be determined. Invitation only.