Print This Article
Educational Affairs : Impact of Pharmacist-Led Medication Reconciliation Programs on Readmission Rates, Costs, and Patients' Outcomes During Transition of Care: A Systematic Review
by Marija Andreevski,PharmD Candidate, Martina Bidzhova, PharmD Candidate, Ernestas Sutas, PharmD Candidate, Abby Kahaleh BPharm, MS, MPH, PhD Roosevelt University College of Pharmacy
Discussion
The purpose of this systematic review is to evaluate the benefits of pharmacist-led patient care programs during transition of care, based on economic, clinical, and humanistic outcomes (ECHO). The goal is to identify and clarify gaps in the current understanding of pharmacist provided medication reconciliation services on reducing 30-day readmission rates, increasing patient cost savings, and improving patients’ quality of life. In our efforts to review these programs, we hope to provide more insight into beneficial strategies that employ medication review with the goal to result in positive health and economic outcomes.
Background
Description of the problem
Transition of care presents a significant challenge to health care providers. The vast number of physicians, nurses, and other health care personnel involved in treating and discharging a patient increases the odds of miscommunication and can result in a variety of medical errors. It is estimated that approximately 60% of medication errors happen during transition of care.1 In fact, because preventable transition of care errors make up such a large portion of all medication errors, the Joint Commission included Medication Reconciliation as a national patient safety goal for 2017.2
In addition to patient safety, poorly coordinated transitions of care can negatively affect treatment outcomes and lead to increased health care expenses. Insurance companies - especially the federally and state subsidized Medicare/Medicaid programs that cover elderly, disabled, and patients below the poverty line - are very concerned about the increase in mortality risk and the substantial financial expenses associated with frequent hospital readmissions.3 Approximately 3.3 millions adults were readmitted within 30-days in 2011, with the associated total health care costs of $41.3 billion.3 Seniors 65+y/o on Medicare made up 55.9% of all readmissions, while patients covered by Medicaid and 18-64y/o made up 20.6% of all readmission.3 In 2012, the Centers for Medicare and Medicaid Services (CMS) began to institute the directives described in the Affordable Care Act (ACA), which lead to reduced reimbursement payments for certain types of readmissions (ex; stroke, CHF) within the 30-day period following the discharge from the hospital.4 The resulting change in the hospital health care model from quantity-of-service to quality-of-service, provided hospitals with a financial incentive to reduce their readmission rates.
Description of the condition
The ACA instituted a shift in the US health care model, with a bigger focus on the quality of service and preventative measures. The new policy ties reimbursement rates and other incentives to several key metrics, such as 30-day readmission rate, which forced the entire health care system to search for new strategies that would satisfy the required criteria. Pharmacist-led medication reconciliation programs have grown in importance over the years because such programs provide pharmacists with an opportunity to oversee the entire treatment process, which reduces costs and medication errors.
Description of the intervention
Medication reconciliation and management service is a clinical process with pharmacists providing medication optimization, counseling and education to patients either pre-discharge or post-discharge from the hospital environment. The service can be provided in a variety of different ways including face-to-face, telephonic, and electronic interactions. The systematic review includes face-to-face and telephonic medication management sessions, with a focus on reducing 30-day readmission rate. Secondary benefits of medication reconciliation programs are also examined as they pertain to the economic and patient related quality of life outcomes.
How the intervention is important
The Centers for Medicare and Medicaid Services (CMS) and the Joint Commission express concern regarding patient safety and the positive treatment outcomes during transition of care. The National Patient Safety Goal for 2017 features medication reconciliation and patient education as one of the key points for hospital excellence, while CMS continues to update the Hospital Readmissions Reduction Program with new diagnosis conditions that should be treated in one admission within the 30-day period.5 Pharmacists can help reduce medication errors through medication reconciliation programs due to their broad access to patient treatment information. This helps to reduce errors that occur due to poor communication within the health care system during the transition of care period, and it can also optimize prescription treatment regimen for each individual patient. It could also lead to a reduction in 30-day readmissions, which would result in less financial penalties for hospitals per CMS rules, while increasing patient safety, quality of life, and satisfaction.
Why the review is important
Review of current studies is necessary to understand the benefits and costs associated with employing medication reconciliation programs during transition of care. This review can benefit hospitals in their decision to adopt or reject pharmacist-led medication management programs or other patient care projects, by looking at the overall clinical, economic, and humanistic outcomes. Medication reconciliation programs are associated with certain costs, such as hiring additional pharmacists, so it is necessary to have a complete understanding of the benefits and risks of medication reconciliation programs during transition of care.
Objectives:
The objectives evaluated in this review included an evidence-based assessment of pharmacist-led medication reconciliation interventions in reducing hospital readmission rates, lowering health care costs, and improving patients’ quality of life. The purpose of the review is to determine if such programs will be beneficial if implemented and whether or not they will yield positive results based in the ECHO model. The systematic review analyzes the influence of pharmacist-led medication reconciliation, patient education, and post-discharge follow-up within the confines of this model.
Methods:
Types of studies:
The review includes fifteen studies conducted in the US in the past seven years, published in English, which studied the benefits and drawbacks of pharmacist-led medication review projects. These studies were prospective or retrospective cohorts, or randomized control trials.
Types of participants:
All studies included patients who used health care services in the United States.
Inclusion criteria:
All studies included in this review had to be conducted in a US health care system between 2010 and 2017, and had to be published in English. The studies had to include pharmacist-led medication review and intervention programs and had to evaluate the outcomes on these programs either on an economical, clinical, or humanistic level.
Types of interventions:
Interventions consisted of different types of medication therapy management, including therapy regimen assessment and optimization, medication replacement, discontinuation, initiation, and/or dose and frequency adjustments. Pharmacists also conducted patient education pre-discharge, along with face-to-face or telephonic post-discharge follow-up.
Types of outcomes measured:
1. Primary outcome:
A. Impact of medication reconciliation programs on reducing hospital readmission rates within the 30-days post-discharge.
2. Secondary outcomes:
A. Impact of medication reconciliation programs on:
a. Reducing healthcare costs.
b. Reducing the number of hospital and ED visits.
c. Reducing medication errors and ADE.
d. Improving patients’ quality of life.
Search method used for identification of studies:
Our search was conducted through PubMed, Medline Complete and EBSCO Host online database. Search terms used to find the studies include: “MTM”, “medication reconciliation”, “pharmacist-led programs”, “medication therapy management”, “medication review”, pharmacist-led hospital programs”. All information and data was organized, analytically reviewed and revised individually by 3 of the authors.
Data collection:
Selection of studies
Studies were individually selected and analyzed by 3 authors. All studies were further evaluated by each researcher and if the study was approved by all three, it was included in the review. Titles and abstracts were reviewed, findings examined, and outcomes confirmed through collective discussion. The initial research contained 28 studies and 15 of them were included in the comprehensive research; 13 studies did not fit our inclusion and exclusion criteria and as such were not included in the evaluation. Three types of outcomes were researched and analyzed: hospital readmission rates, cost savings, and improvements in quality of life as they pertain to the outcomes of the ECHO model.
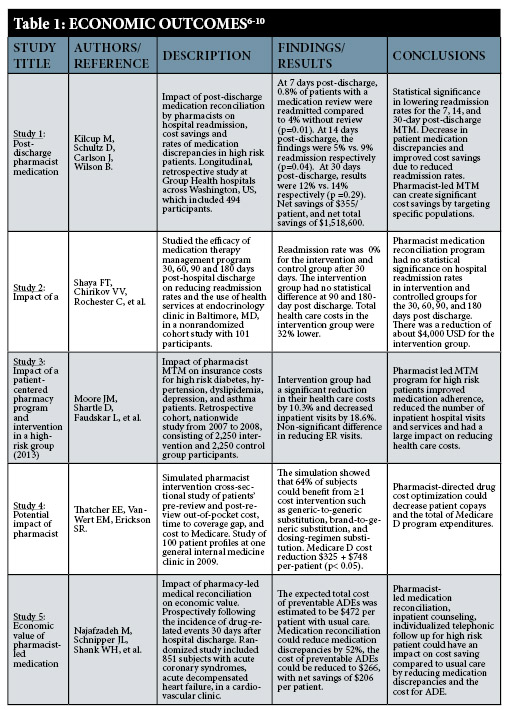
Data extraction
The selected studies were ranked based on the primary and secondary outcomes and the inclusion and exclusion criteria. The study with the most relevant information within an outcome domain (i.e., economic, clinical, humanistic), was ranked as “1” and the study with the least relevant information was ranked as “5”. The studies were then placed into a table, with the most relevant study being listed as the first entry in the table, and the others in the descending order based on their relevance.
Assessment of risk of bias:
The following criteria were used:
- Study funding
- Design of the study
- Study sample size
- Methods used for data analysis
- Study population
- Patient self-selection
- Examination of confounders
Limitations:
Conducting a review for evaluating the effects of pharmacist-led medication reconciliation programs during the transition of care process can be difficult due to the lack of randomization and the imbalance of important covariates between the intervention and control groups. Small sample sizes can impact the power to detect significant differences between groups. Studies conducted at a single site can lead to statistically different results in comparison to other hospitals due to their geographical and/or socioeconomic limitations. Inability to see actual patient data due to poor communication between health care facilities/systems can lead to the misinterpretation of true treatment outcomes in cases where patients are readmitted elsewhere. High risk and low risk patients can be hard to compare due to different classifications among the research studies.
Measures of treatment effect:
The following measures were used to assess treatment effect: reduction in 30-day readmission rates, total net cost savings for each patient and the health care system, reduction in medication errors and ADEs, patient satisfaction, and improvement in quality of life.
Results Summary:
Summary of main results:
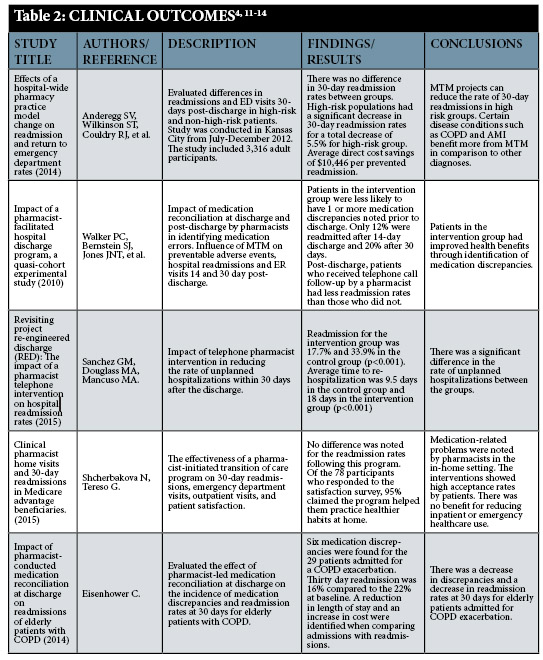
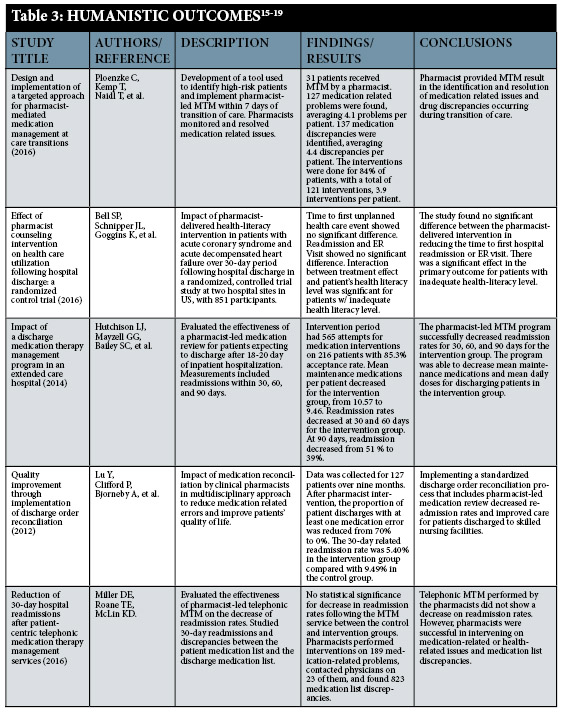
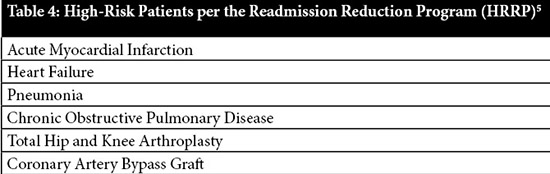
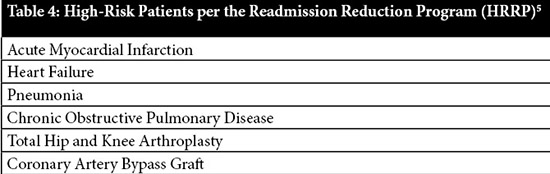
Medication reconciliation programs show evidence in being able to reduce medication errors, improve costs, and increase patients’ quality of life. This systematic review focused on the effectiveness and benefits of pharmacist-led medication reconciliation programs during the transition of care process. For the purpose of this review, we were primarily concerned with the relationship between these programs and 30-day readmission rates. The 30-day readmission rate statistics were chosen because this measurement is utilized by CMS to calculate hospital reimbursements in several readmission categories.5 In our findings medication reviews produced a clinically significant readmission rate reduction in patient populations considered as high-risk and not across the board for the general public. However, while the definition of who is considered a “high-risk” or “low-risk” patient varied among our studies, one of the limitations of this systematic review is that positive clinical outcomes appear to be closely associated with patients’ medical literacy level and the cause for their admission to a hospital. In comparison to the clinical aspect of medication reconciliation programs, the economic and humanistic outcomes are not limited to high-risk patient populations. Pharmacist-led medication reviews demonstrated significant individual health cost savings for the majority of patients and the total reduction in expenses for insurance companies. It also showed valuable improvements in patients’ quality of life by decreasing medication discrepancies, adverse drug events and other medication complications.5
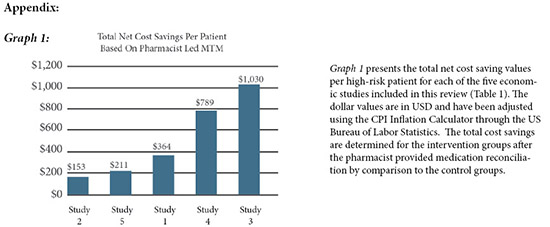
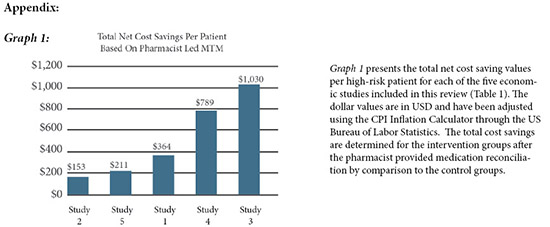
Net reduction in health care costs was averaged through all five studies to be between $153-$1,030 USD per patient for participants receiving medication reconciliation, particularly for those with a high-risk health conditions. Advanced age, high-risk dyslipidemia, hypertension, diabetes, asthma, acute coronary syndrome and other health status variables were used to classify patients as “high-risk” in order to determine the maximum cost savings made possible with the use of medication review programs during the transition of care process.5 This review shows the positive benefits of pharmacists’ interventions in reducing transition of care issues and medication list optimization. A reduction in errors was seen during transition of care, particularly for patients deemed as high-risk and/or with inadequate health literacy.
Conclusions:
In the fifteen studies evaluated in this review, medication reconciliation consistently showed positive results in increasing patients’ quality of life while decreasing the overall health care expenses for the majority of patients and providers of health care services. However, medication reconciliation programs do not appear to make a statistically significant impact in reducing the 30-day readmission rates in low-risk populations or populations with adequate health literacy levels. Therefore, we suggest that hospitals consider carefully the characteristics of their patient population when determining whether to use medication reconciliation solely for the purpose of reducing their 30-day readmissions rates. Due to the unique position that pharmacists have in the treatment process, pharmacist-led medication review remains a valuable option for managing transitions of care because this can increase patient safety via medication reconciliation, optimization, and patient education. For the most part, the majority of these benefits are seen only in the long-run or in specific patient populations.7,17 We feel that hospitals should utilize pharmacist-led medication review during transitions of care due to the overall positive effects in every population, and specifically in patients who can be classified as high-risk. Hospitals should implement pre-discharge medication review to optimize treatment regimens, decrease medication errors, and increase patient safety. Face-to-face medication management performed in hospital settings for inpatient hospitalizations should be prioritized due to the easy and direct access to the patient. Post-discharge telephonic follow-up is a low cost method to further monitor and counsel patients, but it is not always as viable as pre-discharge medication reconciliation when patients cannot be contacted. We suggest further studies to be performed by each individual hospital to evaluate its own benefits of such programs. ■
References
- American College of Clinical Pharmacy, Kirwin J, Canales AE, et al. Process indicators of quality clinical pharmacy services during transitions of care. Pharmacotherapy. 2012;32(11):338.
- The Joint Commission. National patient safety goals 2017. Available at: https://www.jointcommission.org/standards_information/npsgs.aspx. (accessed 2017Jul 12.)
- Conditions with the largest number of adult hospital readmissions by payer, 2011. The HCUP report: Healthcare cost and utilization project (HCUP): Statistical briefs; 2014 ASI 4186-20.172; Statistical brief no. 172. 2014.
- Anderegg SV, Wilkinson ST, Couldry RJ, et al. Effects of a hospitalwide pharmacy practice model change on readmission and return to emergency department rates. Am J Health Syst Pharm. 2014;71(17):1469-1479.
- Centers for Medicare and Medicaid Services. Readmissions reduction program. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. (accessed 2017 Jul 20).
- Kilcup M, Schultz D, Carlson J, et al. Postdischarge pharmacist medication reconciliation: Impact on readmission rates and financial savings. J Am Pharm Assoc. 2013;53(1):78-84.
- Shaya FT, Chirikov VV, Rochester C, et al. Impact of a comprehensive pharmacist medication-therapy management service. J Med Econ. 2015;18(10):828-837.
- Moore JM, Shartle D, Faudskar L, et al. Impact of a patient-centered pharmacy program and intervention in a high-risk group. J Manag Care Pharm. 2013;19(3):228.
- Thatcher EE, VanWert EM, Erickson SR. Potential impact of pharmacist interventions to reduce cost for medicare part D beneficiaries. J Pharm Pract. 2013;26(3):248-252.
- Najafzadeh M, Schnipper JL, Shrank WL, et al. Economic value of pharmacist-led medication reconciliation for reducing medication errors after hospital discharge. Am J Manag Care. 2016;22(10):654.
- Walker PC, Bernstein SJ, Jones J, et al. Impact of a pharmacist-facilitated hospital discharge program: A quasi-experimental study. Arch Intern Med. 2009;169(21): 2003-10.
- Sanchez GM, Douglass MA, Mancuso MA. Revisiting project re-engineered discharge (RED): The impact of a pharmacist telephone intervention on hospital readmission rates. Pharmacotherapy. 2015;35(9):805-812.
- Shcherbakova N, Tereso G. Clinical pharmacist home visits and 30-day readmissions in Medicare advantage beneficiaries. J Eval Clin Pract. 2016;22(3):363-368.
- Eisenhower C. Impact of pharmacist-conducted medication reconciliation at discharge on readmissions of elderly patients with COPD. Ann Pharmacother. 2014;48(2):203-208.
- Ploenzke C, Kemp T, Naidl T, et al. Design and implementation of a targeted approach for pharmacist-mediated medication management at care transitions. J Am Pharm Assoc (2003). 2016;56(3):303-309.
- Bell SP, Schnipper JL, Goggins K, et al. Effect of pharmacist counseling intervention on health care utilization following hospital discharge: A randomized control trial. J Gen Intern Med. 2016;31(5):470-477.
- Hutchison LJ, Mayzell GG, Bailey SC, et al. Impact of a discharge medication therapy management program in an extended care hospital. Consult Pharm. 2014;29(1):33-38.
- Lu Y, Clifford P, Bjorneby A, et al. Quality improvement through implementation of discharge order reconciliation. Am J Health Syst Pharm. 2013;70(9):815.
- Miller DE, Roane TE, McLin KD. Reduction of 30-day hospital readmissions after patient-centric telephonic medication therapy management services. Hosp Pharm. 2016;51(11):907-914.