Official Newsjournal of the Illinois Council of Health-System Pharmacists
2017 Best Practice Award Winner
Implementation of Integrated Telepharmacy Services Achieve a Health-System Standard of Pharmacy Care
Feature Article
by Sandra M. Salverson , PharmD, BCPS and Jerry Storm, RPh

WINNER

The 2017 Best Practice Award Winner, Implementation of Integrated Telepharmacy Services Achieve a Health-System Standard of Pharmacy Care, is available as a home-study for CPE credit. To earn your CPE credit, you must read the manuscript below in the September/October 2017 issue of KeePosted and then go toCEsally.com to answer the self-assessment questions and complete your credit. Once you have logged in to your CEsally.com account, search on Implementation of Integrated Telepharmacy, add to your To Do List, be sure and save CE, and then go to your To Do List to complete the process. If you have questions on how to set up your CEsally account, please call the ICHP office at 815-227-9292.
Peoria, IL
OSF Healthcare System
Target Audience
- Identify three functions ePharmacists can perform within a telepharmacy model.
- Recognize one clinical outcome and one dispensing outcome from integrating telepharmacy services into a health-system model of pharmacy care.
- Identify the role of the pharmacy technician in a pharmacy model with integrated telepharmacy services.
- Recognize the impact 24/7 pharmacist prospective review of medication orders has on dispensing doses from night-rooms.
 This program is provided by the Illinois Council of Health-System Pharmacists. The Illinois Council of Health-System Pharmacists is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. This program is equivalent to 0.5 contact hour (0.05 CEU) of pharmacy continuing education.
This program is provided by the Illinois Council of Health-System Pharmacists. The Illinois Council of Health-System Pharmacists is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. This program is equivalent to 0.5 contact hour (0.05 CEU) of pharmacy continuing education.
Introduction
Many health-systems participate in quality care and/or value-based reimbursement programs. The commitment to sharing risk within payment models means if quality care is provided, health-systems will receive reimbursement for those achievements. If quality care is not provided, payment received will continue to decline the more the target is missed. This change in the reimbursement model has healthcare-systems searching for ways to achieve significant financial efficiencies and improve quality. Mergers and acquisitions continue to occur in response to the need for economies of scale. As a result, many health-systems now contain a blend of hospital sizes.
The costs of both appropriate medication use and suboptimal medication use comprises approximately 10% of the total dollars spent in the United States.1 Optimizing medication use within a health-system is collaborative and requires partnerships across disciplines and geographies of the health-system.2 In 2013, a survey of pharmacy services in small and rural hospitals in Illinois demonstrated approximately 23.5% - 31% use a drug-distribution model of care and approximately 50% deliver patient-specific clinical services the majority of time.3 Another study4 reported rural facilities, defined as an average daily census of 49 or fewer inpatients, were less likely than larger hospitals to demonstrate safe medication practices and were less likely to support a full-time pharmacist due to limited patient volume and/or lack of financial resources. The pharmacy enterprise needs to advocate for and optimize the value of drug therapy and medication use safety. The challenge within the large health-system models is to implement these solutions consistently across an entire enterprise that contains tertiary-referral medical centers, rural community hospitals, and critical access hospitals.
Purpose/Goal
The aim of the health-system is to provide consistent quality care for people in the communities they live. In 2012, the health-system opted to pursue an operating organizational structure to manage care for patient populations, enhance decision making, increase agility, increase service consistency, improve clinical care, and improve cost management. In 2014, health-system administration asked pharmacy services to functionally transform. In lieu of operating independent pharmacy departments within each respective hospital, the objective was to form one operational department for the entire health-system and to optimize service delivery. Using the existing human resources, administration requested pharmacy services design a model of care that ensured all patients have access to the same level of pharmaceutical care, improved patient outcomes, and improved medication outcomes associated with the medication use process.
Description of the Program
The health-system includes eleven hospitals in urban and rural settings: one tertiary referral medical center with a children’s hospital, six community hospitals, and four critical access hospitals. The health-system shares the same electronic medical record with computerized provider order entry and bar-code medication administration. Two-thirds of the hospitals used automated dispensing cabinets as the core medication distribution system.
Senior pharmacy leadership conducted interviews with administrators, pharmacy leaders, nursing leaders, medical staff involved in pharmacy and therapeutics work, and pharmacists across the health-system to determine 1) what medication use and pharmacy practices are evidence-based and effective and 2) the top concerns/gaps in care. Table 1 reports the results of the gap analysis and top priorities identified. The redesigned pharmacy practice model recommended all hospitals include: around-the-clock order verification, around-the-clock emergency department order verification, patient education, discharge medication reconciliation review, antimicrobial stewardship, and focused pharmacy dosing services.
Table 1. Pharmacy Services Gap Analysis and Care Model Priorities Pre and Post-Functional Transformation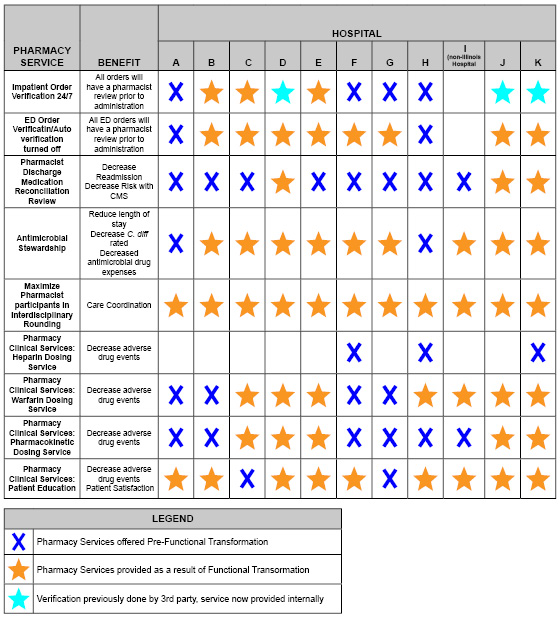
The new model of pharmacy care implemented centralized patient care services through ePharmacy, a virtual telemedicine service. ePharmacists prospectively verify orders around-the-clock for every single hospitalized patient within the health-system. ePharmacists review discharge medication reconciliation and identify potential errors in both the visit summary and discharge scripts to prevent adverse events and readmissions prior to every patient’s discharge. ePharmacists also manage first-dose consults for antibiotics and warfarin (under the auspices of collaborative drug therapy management (CDTM) agreements with each hospital’s independent medical staff). Pediatric ePharmacy, supported by the health-system’s children’s hospital, manages the health-system’s pediatric orders, consults, and discharge medication reconciliation review. Pharmacists and technicians on-site at the hospitals are responsible for medication distribution and medication compounding. Pharmacists at the hospital sites educate patients receiving any oral anticoagulants, participate in interdisciplinary rounds, practice antimicrobial stewardship services, and perform the daily consult dosing services for antibiotics, warfarin, and heparin (under the auspices of CDTM agreements). Pharmacists functioning located at the critical access hospitals function in a hybrid model. The provide telepharmacy services for the entire health-system and the services expected for site pharmacists. Figure 1 below exhibits the model implemented.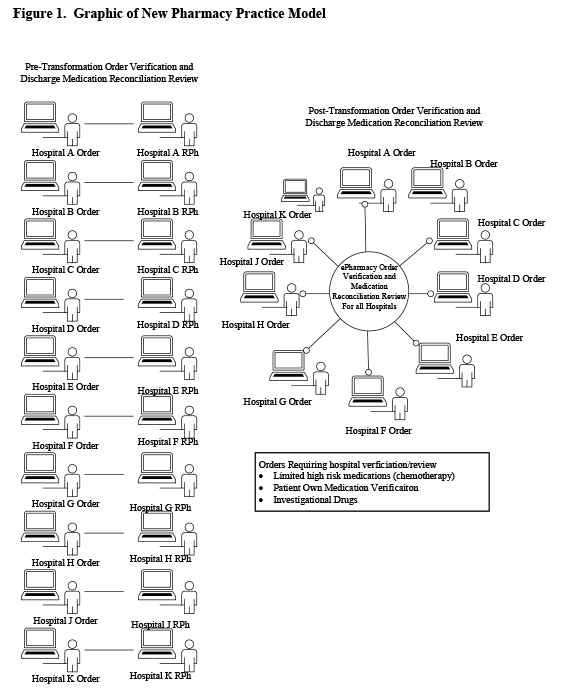
Execution of pharmacist prospective order review around-the-clock throughout the health-system allowed the development and implementation of a standard process for after-hours dispensing when a pharmacist is not physically present at a hospital. The objective was to minimize nurses’ need to use the after-hours night room/cabinet and almost completely eliminate the need for nurses to compound IV infusions when the pharmacist is not on-site. Medication distribution systems were aligned and implemented to maximize automated dispensing cabinet use. Automated dispensing cabinets are all profiled, with the exception of procedure areas. Override medication lists permitting bypass of prospective pharmacist review were redesigned and limited to medications for patient emergencies.
Implementation of around-the-clock pharmacy services throughout the health-system granted full coverage of pharmacist managed dosing services offered. CDTM agreements were aligned and implemented for warfarin, heparin, vancomycin, and aminoglycosides.
Experience with and Outcomes of the Program
Order Verification and After-hours Dispensing Practices
Prior to the practice model change, average turn-around times for medication review and nursing access to medications in automated dispensing cabinets averaged 140 – 180 minutes for high priority orders, and 180 minutes for routine orders. Implementation of ePharmacy services yielded high priority order review with medications accessible in 15 minutes or less; routine orders review and medication access occurs in 60 minutes or less, consistently. Prospective pharmacist review of orders around-the-clock and re-design of the medication distribution system in hospitals without an around-the-clock pharmacist physically present resulted in a 95% absolute reduction in the number of non-automated dispensing cabinet dispenses during pharmacy closed hours. Nurse compounding of sterile preparations decreased by 87%. Table 2 summarizes the changes in doses dispensed by nurses after-hours. It eliminated the need for nurses to enter the pharmacy after-hours.
Table 2. Changes in Doses Prepared and Dispensed by Nurses After-Hours
| Mean Number of Non-Automated Dispensing Cabinet Doses Dispensed | Mean Number of Nurse Compounded Sterile Preparations | |
| Pre-Pharmacy Practice Model Change (Oct 15 - Mar 15) | 500 | 33 |
| Post-Pharmacy Practice Model Change (Oct 16 - Mar 17) | 25 | 4 |
Pharmacist Discharge Medication Reconciliation Review
Discharge medication reconciliation review was a standard of care within the health-system prior to the model changes. Pre-transformation, pharmacists reviewed 65% of patients discharged. Post-transformation, ePharmacists review 97% of patients discharged. ePharmacists identify at least one drug related problem (drug-drug interaction, drug duplication, inappropriate dose, inappropriate duration, or undertreated condition) and correct the problem(s) for twenty percent of patients immediately prior to discharge. Examples of problems identified and resolved include: omission of anti-hypertensives for a patient admitted for hypertensive crisis, omission of anti-platelet agent for post-myocardial infarction, duplicate prescriptions for rivaroxaban with two unique set of instructions to start on same day, and unnecessary continuation of antibiotics when the course of therapy was documented as complete.
Anticoagulation Management
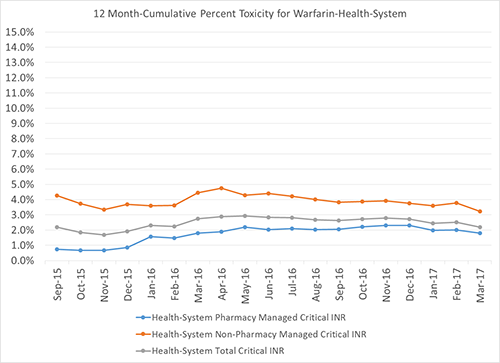
Prior to aligning into one operational department, 50% the hospitals offered pharmacist managed warfarin services. After the operational alignment, all hospitals offer anticoagulation management. The service manages 80% of the warfarin patients within the health-system. Toxicity, as defined by an INR greater than 4.5, began at 0.7% and averages 2.0% post model and patient load increase. Toxicity for patients not managed by pharmacy began at 4.3% and now averages 2.9% for the entire health-system. Overall the health-system maintains a toxicity rate of 2.2% (Figure 2).
Figure 2. Critical INRs for the Health-System
Antimicrobial Stewardship
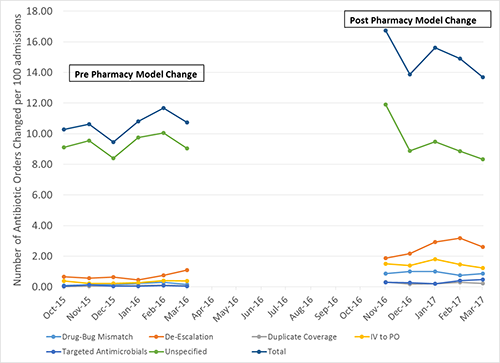
During the time of the model change, a system-wide antimicrobial stewardship program was implemented. Two infectious disease pharmacotherapists mentor and guide pharmacists at each hospital to perform targeted interventions: drug-bug mismatch, de-escalation, duplicate coverage, and intravenous to oral conversions. Figure 3 summarizes the number of documented changes to antimicrobial orders pre- and post-model change. Overall antibiotic use decreased 0.9% across the health-system.
Figure 3. Accepted Antimicrobial Stewardship Pharmacist Recommendations
Patient Education
Patient education was not a priority for pharmacists within the health-system. Centralized order verification allows more pharmacists to leave the pharmacy and interact with patients. A goal was set to educate patients receiving any oral anticoagulants (warfarin or a direct thrombin inhibitor) prior to discharge. Pharmacists now educate 75-85% (410 – 450 patients/month) of patients receiving an oral anticoagulant. This meets both the Joint Commission National Patient Safety Goal expectations and targets one of the health-system’s high risk populations for readmissions.
Clinical Outcomes
Pharmacist documentation of drug-related problems and resolution was an expectation throughout the health-system. Pharmacist document recommendations using the taxonomy described by Hoth et al.5 Figure 4 summarizes the difference in drug problems identified and resolved pre and post model change. The identification and prevention of adverse drug related events (allergy, management of actual adverse drug event, drug-drug interaction, drug-disease interaction, contraindication, therapeutic monitoring for toxicity, or lack of standard preventive care) did not change substantially. Optimization of medication therapies (no indication, untreated condition, undertreated condition, alternative therapy, minimal/no therapeutic effectiveness, dose adjustments for organ dysfunction, duplicate therapy or inappropriate schedule), excluding medications associated with a CDTM agreement, increased by 167%.
Figure 4. Resolution of Drug Related Problems Associated with the New Pharmacy Practice Model

Discussion of Innovative Aspects of the Program and Achievement of Goals
There are very few descriptions of how the integration of a comprehensive around-the-clock telepharmacy service impacts an entire health-system’s ability to meet the critical requirements for health-system pharmacy practice6-10, as outlined in the ASHP Pharmacy Practice Model Summit.11 Remote review of medication orders by pharmacists when the hospital pharmacy is closed has demonstrated a decrease in the number of potential adverse events reported within critical access hospitals.7-9 A pharmacist-managed reconciliation service using telepharmacy demonstrated improved discharge medication lists and documentation received by patients.10 The experiences published thus far report benefit to the critical access hospitals and do not describe an integrated health-system approach. The ASHP statement published in May 2017 calls for further research to be conducted to establish best practices.12
The integration of a centralized telepharmacy service into the health-system practice model allowed for expanded pharmacy services for a broad range of hospital sizes and types without the addition of additional resources. The integrated model achieved patient centered outcomes and correction of prescribing errors and drug related problems, similar to Sankaranarayanan et al.8 The model demonstrated outcomes at all hospitals and was not limited to the critical access hospitals alone. The model allows the provision of specialized services (pediatrics, antimicrobial stewardship) and expertise that typically would not be robustly implemented within the critical access and small rural hospital setting.3-4 All hospitals now have the ability to provide recommended pharmaceutical care for all patients: medication reconciliation, review of orders before administration of the first dose, individualized treatment and monitoring plans, provision of patient education, daily drug monitoring, and participation in patient care rounds. The health-system also delivers consistent services for high-risk patients as well: anticoagulation management, antimicrobial stewardship, streamlined medication orders, pharmacokinetic evaluation, monitoring, and dosing, and renal dose adjustments.
Conclusion
Integrated telepharmacy services with the redistribution of pharmacist resources increased patient access to pharmacists. The new model yields consistent pharmacy services throughout one health-system, identifies and resolves more drug-related problems than the previous federated model.
References
- National Center for Health statistics, Center for Disease Control and Prevention. Health expenditures (2014 data). https://www.cdc.gov/nchs/fastats/health-expenditures.htm (accessed 2017 Jun 17).
- Knoerr, S. Stewardship of the pharmacy enterprise. Am J Health-Syst Pharm 2014; 71:1204-9.
- Crawford SY, Schumock GT, Ursan JD, et al. Comparison of pharmacy services at critical access hospitals and other rural and small hospitals in Illinois. Am J Health-Syst Pharm 2013;70:1313-21.
- Cochran G, Jones K, Xu L, et al. Prevalence of evidence-based safe medication practices in small rural hospitals. RUPRI Center for Rural Health Policy Analysis. Rural Issue Brief. Brief No 2008-1. https://cph.uiowa.edu/rupri/publications/issuebriefs/IssueBrief2008-1.pdf (accessed 2017 Jun 17).
- Hoth AB, Carter BL, Ness J, et al. Clinical Pharmacist Recommendation Taxonomy Pharmacotherapy 2007;27(5):639-646.
- Garrelts JC, Gagnon M, Eisenberg C, et al. Impact of a telepharmacy in a multi-hospital health-system. Am J Health-Syst Pharm 2010;67:1456-62.
- Wakefield DS, Ward MM, Loes JL, et al. Implementation of a telepharmacy service to provide round-the-clock medication order review by pharmacists. Am J Health-Syst Pharm 2010;67:2052-7.
- Sankaranarayanan J, Murante LJ, Moffett LM. A retrospective evaluation of remote pharmacist interventions in a telepharmacy service model using a conceptual framework. Telemedicine and e-Health. 2014; 10(20): 893-901.
- Peterson CD, Rathke A, Skwiera J, et al. Hospital telepharmacy network: delivering pharmacy services to rural hospitals. J Pharm Technol 2007; 23:158-65.
- Keeys C, Kalejayie B, Skinner M, et al. Pharmacist managed inpatient discharge medication reconciliation: a combined onsite and telepharmacy model. Am J Health-Syst Pharm 2014; 71:2159-66. Shane R. Critical requirements for health-system pharmacy practice models that achieve optimal use of medicines. Am J Health-Syst Pharm 2011; 68:1101-11.
- Alexander E, Butler CD, Darr A, et al. ASHP Statement on telepharmacy. Am J Health-Syst Pharm 2017; 74:e236-41.
Contents
Features
2017 Best Practice Award Winner
Columns
College Connection
University of Illinois at Chicago (Rockford)
More
Officers and Board of Directors
ICHP Pharmacy Action Fund (PAC) Contributors
Regularly Scheduled Network Meetings
Chicago Area Pharmacy Directors Network Dinner
3rd Thursday of Odd Months
5:30pm
Regularly Scheduled Division and Committee Calls
Executive Committee
Second Tuesday of each month at 7:00 p.m.
Educational Affairs
Third Tuesday of each month at 11:00 a.m.
Government Affairs
Third Monday of each month at 5:00 p.m.
Marketing Affairs
Third Tuesday of each month at 8:00 a.m.
Organizational Affairs
Fourth Thursday of each month at 12:00 p.m.
Professional Affairs
Fourth Thursday of each month at 2:00 p.m.
New Practitioner Network
Second Thursday of each month at 5:30 p.m.
Technology Committee
Second Friday of each month at 8:00 a.m.
Chicago Area Pharmacy Directors Network Dinner
Bi-monthly in odd numbered months with dates to be determined. Invitation only.