Official Newsjournal of the Illinois Council of Health-System Pharmacists
 Directly Speaking
Directly Speaking
It's Time to Trade Shoes
by Scott A. Meyers, Executive Vice President
I came home from the meeting with several important takeaways. The first huge takeaway is that patients deserve better education than they often get from us – and I’m talking about all of us. Many times patients go home on new medications that require special administration (e.g., injections, infusions, special inhalers) or have medications that require special timing or other requirements that if not followed can nullify their effect or cause additional problems. This shouldn’t be new to any of us. But are we owning the responsibility to make sure the patients not only receive an explanation of these requirements but actually understand them, can repeat them and even demonstrate them? Or do we assume that the community pharmacy that provides the medications in question provide the important and detailed training that should accompany them? We all know what the assume-game leads to, if not just watch the early part of “The Bad News Bears” circa 1976!
Counseling patients that are headed home doesn’t sound like it has anything to do with our long-term care colleagues but in fact, when pharmacists don’t counsel and educate a patient or their caregiver appropriately, they often end up in a long-term care facility. I heard some real horror stories from patient advocates who presented. The most embarrassing was the patient’s daughter who told the advocate, “The nurse in the hospital was kind enough to take a few minutes to show me how to do the injection.” Where was the clinical pharmacist? Who provided the medications for home use and why didn’t they make sure the caregiver was ready for the challenge?
The second takeaway related to medication reconciliation. Long-term care pharmacists are faced with the same med-rec challenges that hospital pharmacists face. They often receive hand-written discharge summaries (by the nursing staff) that fail to contain all the medications the patient should take or at least have access to if needed. You know the problems you face on the inpatient side when you try to determine what a new admission is on at home. Did we get all the OTCs, herbals and supplements? What was the green pill really supposed to treat? What kind of sugar pill was it that you’ve been taking and how often do you take it? You have those questions everyday if you’re performing med-rec, and the same thing is true of the long-term care pharmacist. However, they also deal with confused patients and caregivers who assume that they should restart some of the medications they were on before their hospitalization even though they weren’t getting them in the hospital and they don’t appear on the discharge summary. Maybe it’s time to look at your discharge system and see if the medication summary can’t be improved.
Hospitals are now being paid for performance and penalized for readmissions too soon. Our colleagues in the long-term care field can have a dramatic impact on readmission if we develop a stronger relationship with them. And when they do send someone back to the hospital from a rehab or nursing home facility, they can ease our workload by communicating an accurate medication history. I really think we need to build new relationships with the folks who receive more and more of our patients as the population ages.
A third takeaway is that it’s never too early to establish a Medical Power of Attorney” for yourself, your spouse, parents and other loved ones. Having the medical power of attorney in place protects you and your family members from unnecessary stress and expense. Hopefully you’ll never have to exercise that power of attorney but chances are very good that eventually you will. Having it in place makes care much easier. So maybe these shoes don’t belong to the long-term care folks but rather someone you love.
So what can the hospital pharmacist do to make life better for their patients when they leave the hospital? Make sure the patient or their caregiver or both, fully understand how, what and why of taking each medication to help reduce readmissions or admissions to the nursing home. If that requires establishing a medication education team, make sure it is overseen by pharmacists even if nurses are utilized. Develop iron-clad medication lists that go out with every discharge regardless of whether the patient is headed home, rehab or the nursing home.
Be prepared and willing to provide needed information to the pharmacist that picks up the patient on the other side of the discharge. They are health care providers and HIPAA allows you to provide the appropriate and critical information. Encourage patients to develop and build a relationship with a local pharmacy. When you find a pharmacy that does a great job with patient care, recommend it. You can do that! Make sure you and your family have established your medical powers of attorney. You hope to never use them, but preparation now will be priceless later.
I thoroughly enjoyed the time I spent at the ASCP Spring Meeting and Exhibition, and I learned more than I thought I would. I now feel stronger than ever that ICHP and all of Pharmacy needs to work harder on the continuity of care, transitions of care or whatever you prefer to call it. I hope that more will come from my experiences at this meeting and only time will tell.
One other nugget from the meeting, ASCP President, Sean Jeffrey announced at the meeting that ASCP will be changing their name! The Board of Directors feels strongly that the pharmacist members of ASCP are more than consultant pharmacists and there certainly should be a better description of their membership. My vote is the Association of Senior Care Pharmacists…I’m all for saving logos and acronyms!
Contents
Features
History of Organized Hospital Pharmacy in Illinois: Organizational Relationships
Columns
College Connections
Pathways to Pharmacy in a Physics Class
A Reflection on Institutional Pharmacy
More
Officers and Board of Directors
ICHP Pharmacy Action Fund (PAC) Contributors
Regularly Scheduled Network Meetings
Chicago Area Pharmacy Directors Network Dinner
3rd Thursday of Odd Months
5:30pm
Regularly Scheduled Division and Committee Calls
Executive Committee
Second Tuesday of each month at 7:00 p.m.
Educational Affairs
Third Tuesday of each month at 11:00 a.m.
Government Affairs
Third Monday of each month at 5:00 p.m.
Marketing Affairs
Third Tuesday of each month at 8:00 a.m.
Organizational Affairs
First Tuesday of each month at 1:00 p.m.
Professional Affairs
Fourth Thursday of each month at 2:00 p.m.
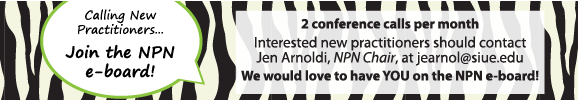
New Practitioner Network
Second Thursday of each month at 5:30 p.m.
Technology Committee
Second Friday of each month at 8:00 a.m.
Chicago Area Pharmacy Directors Network Dinner
Bi-monthly in odd numbered months with dates to be determined. Invitation only.